
The University of Iowa
Department of Ophthalmology and Visual Sciences
April 6 2015
Blepharoptosis or ptosis (pronounced "TOE-sis") is defined as drooping of the upper eyelid. Ptosis can be bilateral or unilateral and can be difficult to identify unless a proper exam is performed. Ptosis is relatively common in the general population and while frequently regarded as a purely cosmetic issue, ptosis can be visually disabling and may be a sign of underlying systemic disease. Ptosis affects men and women equally and there is little data regarding incidence differences between races (1). Comprehensive studies that investigate the incidence and prevalence of ptosis are lacking, but one study looking at individuals 50 years of age and older in England discovered that 11.5% had some form ptosis and that the prevalence of ptosis increased greatly with age (2). While involutional ptosis is the most common cause of ptosis in older populations, there are many etiologies that affect all age groups. Before characterizing the different etiologies of ptosis it is important to have baseline knowledge of the anatomy of the eyelid and how to perform a proper eyelid exam.
The muscles responsible for eyelid retraction are the levator palpebrae superioris, Müller's muscle, and the frontalis muscle. Of these three, the levator muscle is the predominant muscle of eyelid retraction. It is a skeletal muscle that is under voluntary control from cranial nerve (CN) III (oculomotor nerve). The levator originates from the lesser wing of the sphenoid bone. As it traverses the orbit, it broadens and becomes a fibrous aponeurosis that inserts on the anterior aspect of the tarsal plate. The upper eyelid skin crease is formed by attachments of the aponeurosis to the orbicularis muscle and skin. Müller's muscle contributes 1-2 mm of eyelid elevation. It is under sympathetic innervation and can lead to mild ptosis when fatigued or dysfunctional, such as in Horner's syndrome. Phenylephrine eyedrops are used to assess Müller's muscle function and are routinely used for pre-operative planning prior to a planned resection of the muscle. The frontalis muscle lifts the brows and is a minor contributor to eyelid retraction. It is innervated by CN VII (facial nerve). Patients with ptosis will frequently lift their brows to slightly elevate their eyelids, which consequently may result in a brow ache from overuse.
When evaluating ptosis, it is important to obtain a full history encompassing onset, duration, severity, aggravating/alleviating factors, and variability of the ptosis. Encourage patients to bring past photos to assess chronicity. After a baseline history has been obtained, the physical exam of the eye and eyelid is performed. Patients with ptosis often subconsciously raise their eyebrows and tilt back their head to compensate. Ask patients to relax their brows and place their head in a normal position to better assess the extent of the ptosis. When examining the eyelid for ptosis there are three important measurements that need to be obtained: lid crease height, margin reflex distance (MRD), and levator function.
With the patient looking downward, measure the distance from the upper eyelid margin to the lid crease. The lid crease is formed by attachments of the levator aponeurosis to the overlying orbicularis and skin. In males the lid crease is normally 6-8 mm above the eyelid margin. Women have a slightly higher lid crease, normally measured at 8-10 mm.
Have the patient focus on a focal light source with both eyes and measure the distance from the pupillary light reflex to the upper eyelid margin (MRD1) and lower eyelid margin (MRD2) (Fig 1). MRD1 is normally 4-5 mm while MRD2 is normally 5 mm. Palpebral fissure height (PF) is the distance between the upper eyelid margin and the lower eyelid margin: MRD1 + MRD2 = PF.
In order to isolate the levator, firmly place a finger on the patient's brow to negate the effects of the frontalis muscle. Have the patient gaze downward and place a ruler at the upper lid margin. Next have the patient gaze upward and measure the new position of the upper lid, and record the distance between the two measurements as the levator function. Normal levator function is 13-17 mm.
Ptosis may be congenital or acquired. Congenital ptosis will not be discussed in this primer, but more information can be found in the related EyeRounds article. Acquired ptosis can be further categorized as neurogenic, myogenic, aponeurotic, mechanical, or pseudoptosis (3).
The oculomotor nerve innervates the medial rectus, inferior rectus, superior rectus, and inferior oblique muscles. It also innervates the levator palpebrae superioris and carries parasympathetic innervation from the Edinger-Westphal nucleus. Dysfunction results from ischemia, infection, compression, trauma, and demyelinating disease such as multiple sclerosis. Patients may present with any combination of ptosis, ophthalmoplegia, diplopia, and a poorly-reactive dilated pupil (Fig 2). The ptosis may be profound. Complete CN III palsies can be subdivided into pupil-sparing and pupil-involved. Pupil-sparing CN III palsy is commonly due to ischemic injury in patients with vascular risk factors such as hypertension or diabetes. In older patients (>55) giant cell arteritis should be considered. Pupil-involving CN III palsy often indicates a compressive etiology, as the parasympathetic fibers supplying the pupil travel on the outer, more easily compressed portion of the nerve. Pupil-involving CN III palsies should be attributed to compression from a posterior communicating artery aneurysm until proven otherwise, and as such, they warrant urgent investigation with computed tomography angiography (CTA) or magnetic resonance angiography (MRA).


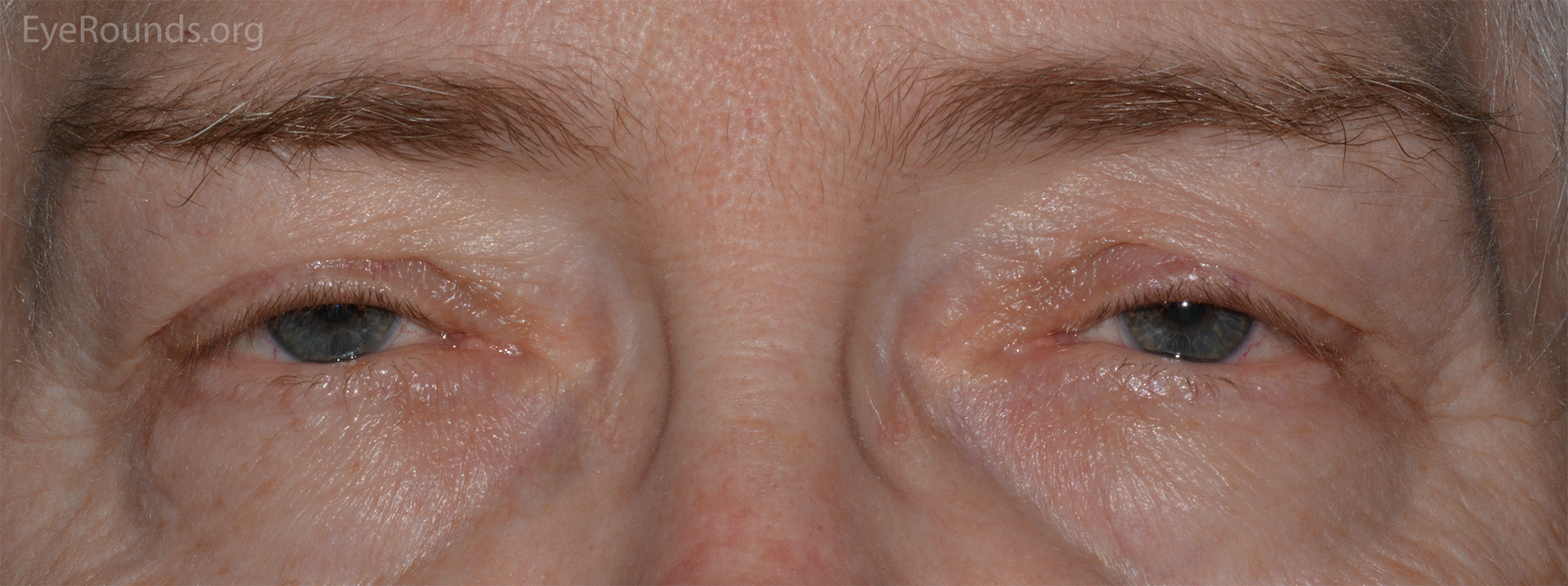
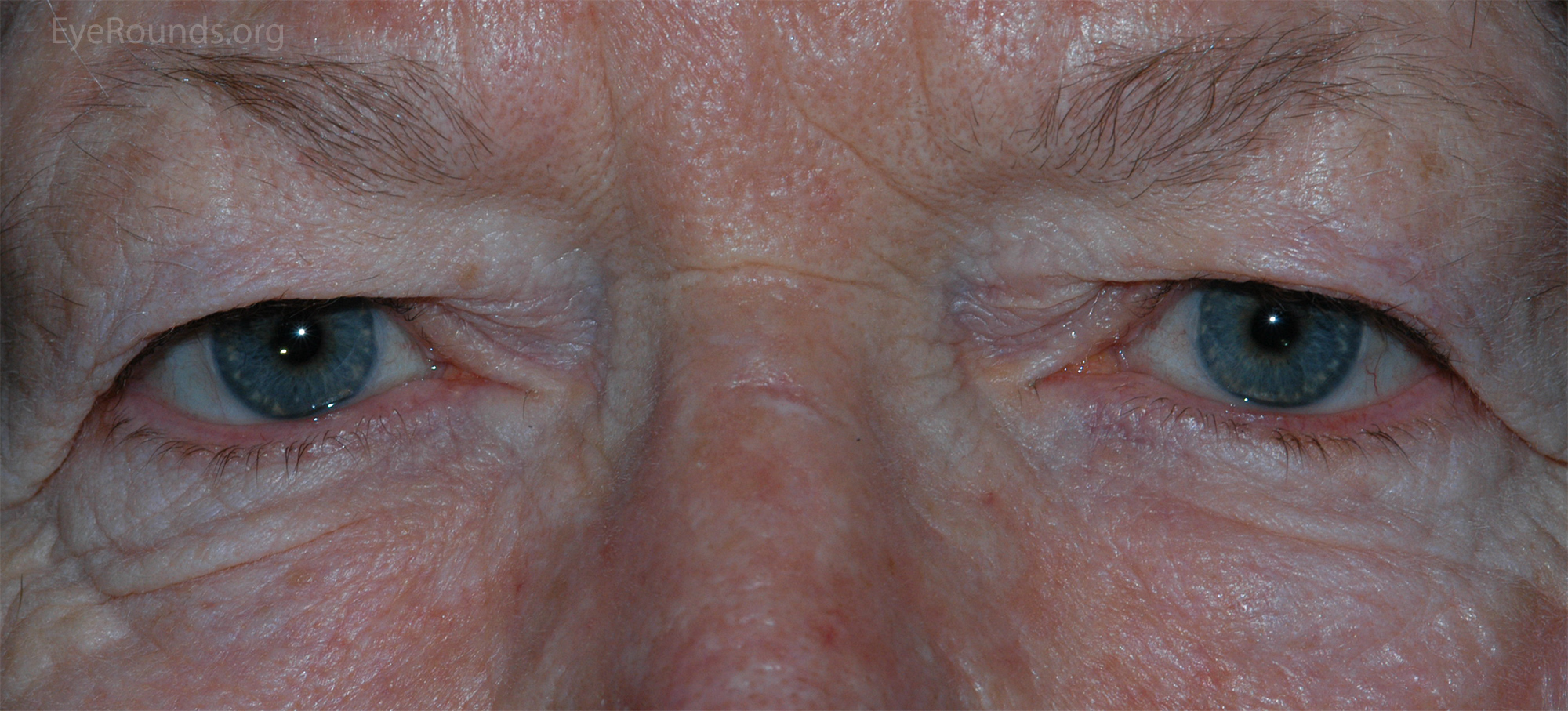
The classic triad for Horner's syndrome includes unilateral ptosis, ipsilateral miosis, and anhidrosis (Fig 3). Since Müller's muscle only contributes 1-2 mm to lid retraction, the associated ptosis is mild. The syndrome results from damage anywhere along the sympathetic pathway, which can be divided by first order neurons (hypothalamus to spinal cord), second order neurons (spinal cord to superior cervical ganglion) and third order neuron (superior cervical ganglion to orbit). It is important to determine which order neuron is involved because Horner's syndrome secondary to involvement of the first or second order neurons may be caused by underlying malignancy. The diagnosis of Horner's syndrome is confirmed if apraclonidine drop testing results in reversal of anisocoria or cocaine drop testing results in exaggeration of anisocoria. Hydroxyamphetamine drop testing is used to localize the level of dysfunction. The drops will result in pupillary dilation if the dysfunction is at the level of the first or second order neurons, while no dilation will occur if the third order neuron is affected. Horner's syndrome is more thoroughly described in the related EyeRounds article.
It is always important to consider myasthenia gravis when examining a patient with ptosis. In 85% of patients with myasthenia, the initial symptoms were either ptosis or diplopia (4). Ptosis in the context of myasthenia gravis can present either bilaterally or unilaterally and can be difficult to distinguish from other forms of ptosis. An important feature of myasthenia is that the ptosis is usually variable, meaning the eyelid position can change on a minute-to-minute basis. Classically the ptosis is more severe in the evening, although all ptosis is worse later in the day or with fatigue. Important physical exam findings include fatigability on prolonged upgaze and an overshoot of the eyelid height when making a saccade from downgaze to primary position (Cogan's lid twitch). The gold standard for diagnosis is serologic confirmation of autoantibodies to the acetylcholine receptors as well as electrophysiological studies. Edrophonium and prostigmine testing are bedside tests that results in temporary elevation of the ptotic eyelid. Cooling the affected eyelid with an ice pack for 2 minutes may also result in temporary reversal of ptosis. The sensitivity of edrophonium testing and ice pack testing is roughly 80% for each test (5,6). Treatment with cholinesterase inhibitor medications often improves the ptosis. Surgery may be considered when medical therapy fails.
OPMD is part of an inherited group of progressive muscular dystrophies and is the most common cause of myogenic ptosis. It is characterized by asymmetric involvement of the levator muscles with progressive dysarthria, proximal limb weakness, and dysphagia. It is typically diagnosed in middle age and is associated with individuals of French Canadian decent. It is also prevalent in the Hispanic population in the U.S. (7,8). OPMD should be suspected in individuals who have an autosomal dominant family history of ptosis and a flat facial expression. Dysphagia is usually not present until later in the course of the disease. Some patients report voice changes but this is rarely documented. The diagnosis of OPMD is confirmed with genetic testing or muscle biopsy. More information regarding OPMD can be found in the related EyeRounds article.
Patients with CPEO present with symmetric, bilateral ptosis and ophthalmoparesis typically in their 30's. CPEO is mitochondrial myopathy and therefore displays a mitochondrial mode of inheritance. Extrinsic eye muscles are particularly vulnerable to certain neuromuscular disorders. These muscles contain a larger volume of mitochondria than any other muscle group, and this results in their preferential involvement in mitochondrial myopathies (9). Symptoms are initially mild and slowly progress to the point of severe ophthalmoplegia. Patients rarely complain of diplopia due to compensatory head movements. Diagnosis is confirmed by muscle biopsy, which shows ragged red fibers. More information on CPEO can be found in the related article.
This syndrome is characterized by early-onset CPEO and retinitis pigmentosa. Other findings include cerebellar ataxia, heart block, diabetes, and cognitive deficits. Patients are at risk of sudden cardiac death and the prognosis is poor, with death usually supervening by the fourth decade.
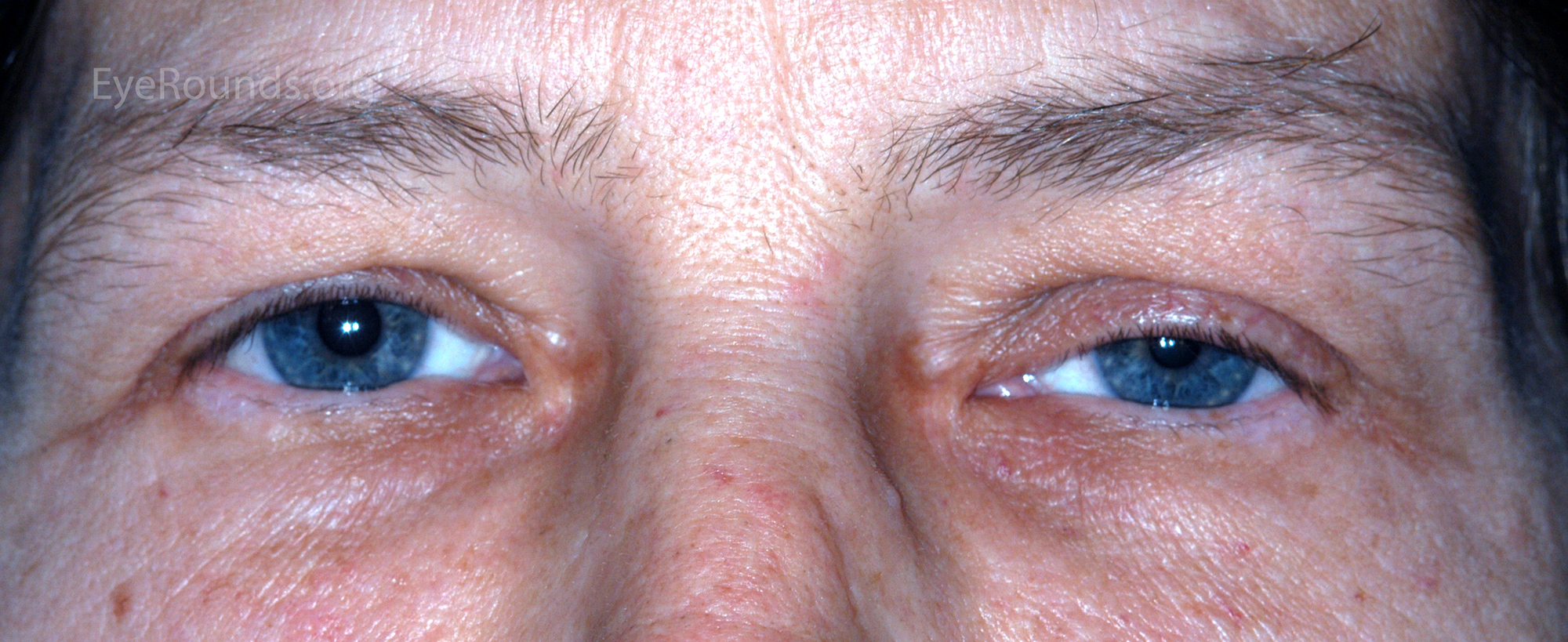
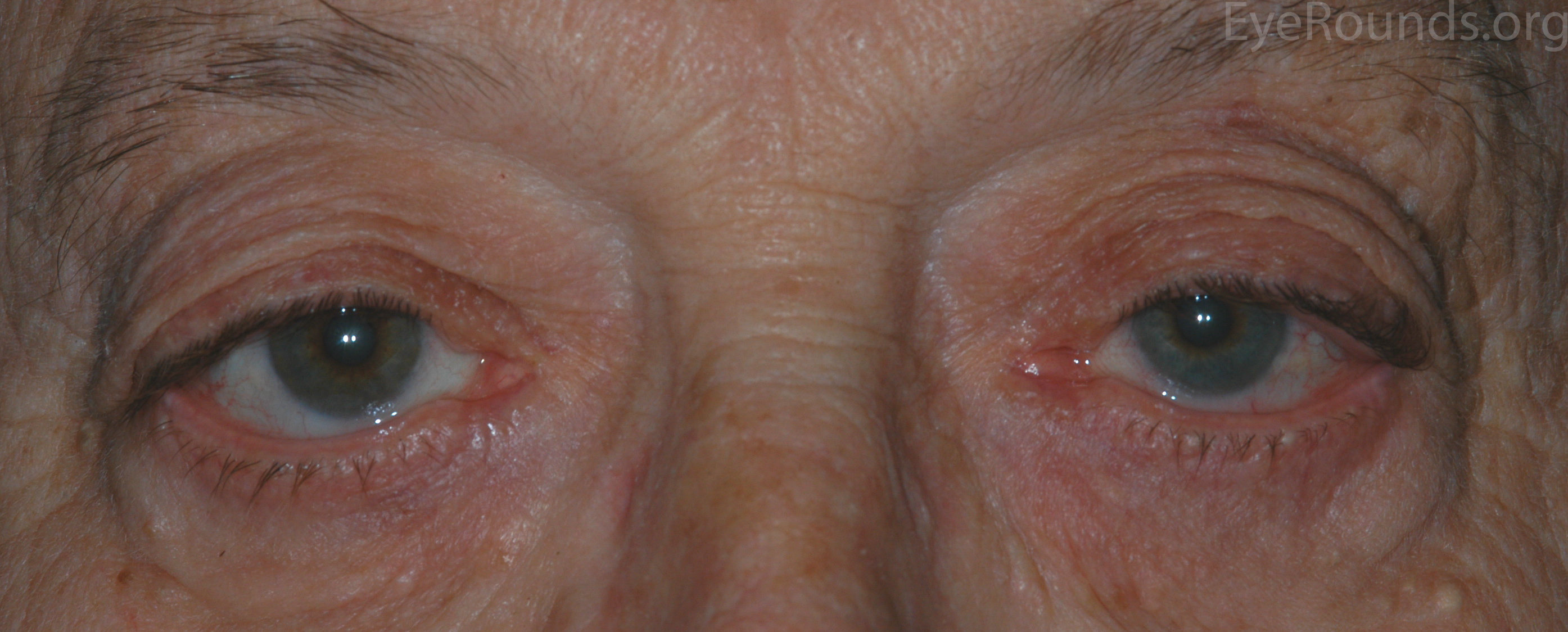
Myotonic dystrophy is a hereditary condition with autosomal dominant inheritance. It is the most common form of adult-onset muscular dystrophy. A defining feature of the disease is myotonia, or a failure of the muscle to relax. The classic description is a patient who is unable to release their grip after a handshake. The condition eventually leads to facial and peripheral muscle weakness (Fig 4). Patients present with bilateral ptosis and a flat facial expression. Myotonic dystrophy can be distinguished from oculopharyngeal dystrophy by the associated systemic findings such as "Christmas tree" cataracts, frontal balding, intellectual impairment, and heart block. In addition, the orbicularis weakness and ocular motility deficits are more prominent in myotonic dystrophy compared to OPMD. Diagnosis is confirmed by genetic testing for an expanded CTG repeat in the DMPK gene.

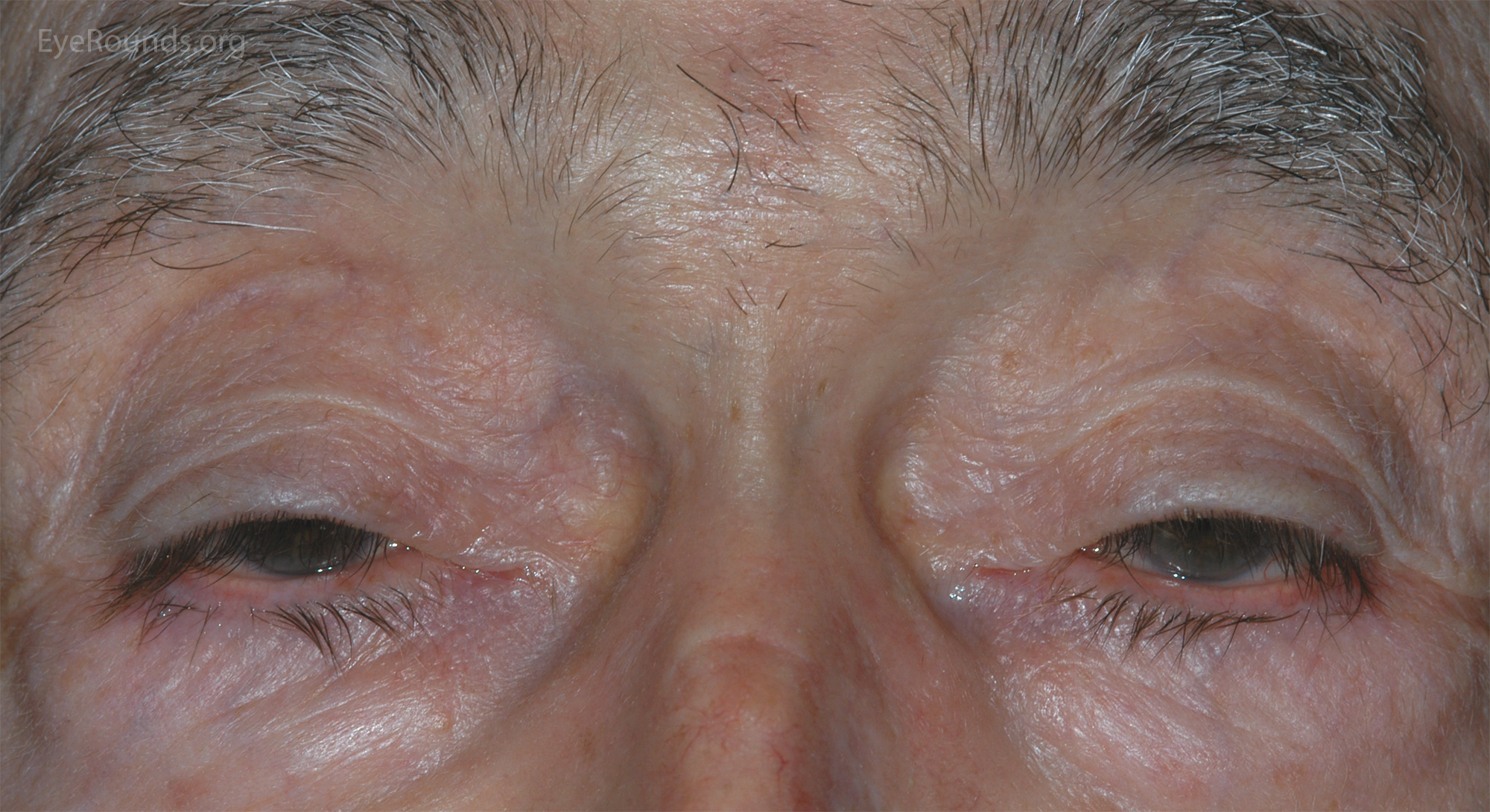
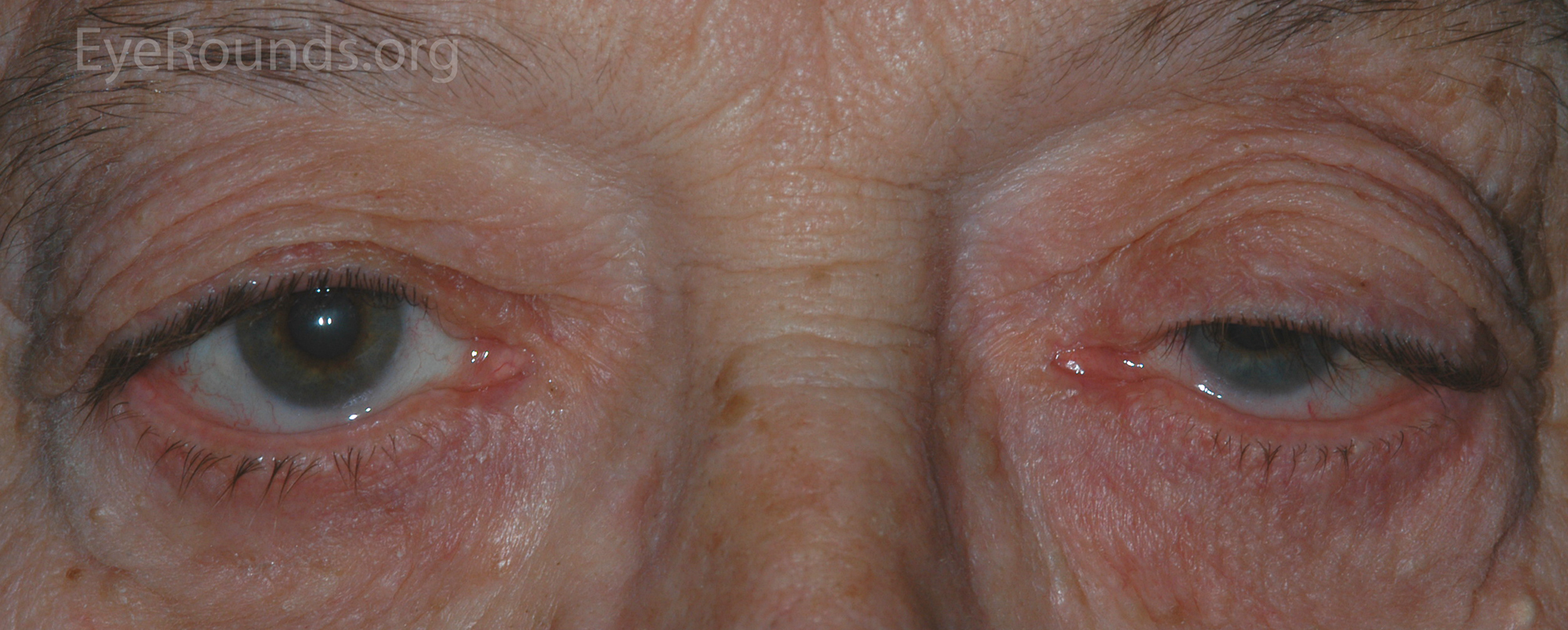
The underlying pathogenesis of aponeurotic ptosis is dehiscence or stretching of the levator aponeurosis connection to the tarsal plate (10). Since this connection is responsible for the formation of the upper lid crease, the crease is often elevated or absent in these cases. Dehiscence of the aponeurosis is often due to involutional changes in older adults and this is the most common cause of ptosis in this population (Fig 5). Involutional ptosis has also been described in relatively younger populations, especially in patients that wear hard contact lenses or chronically rub their eyelids (11). Soft contact lens wear has also been associated with ptosis in some cases (12). The incidence of ptosis in postoperative cataract patients was previously reported to be around 6%, but newer techniques have decreased this incidence (13).
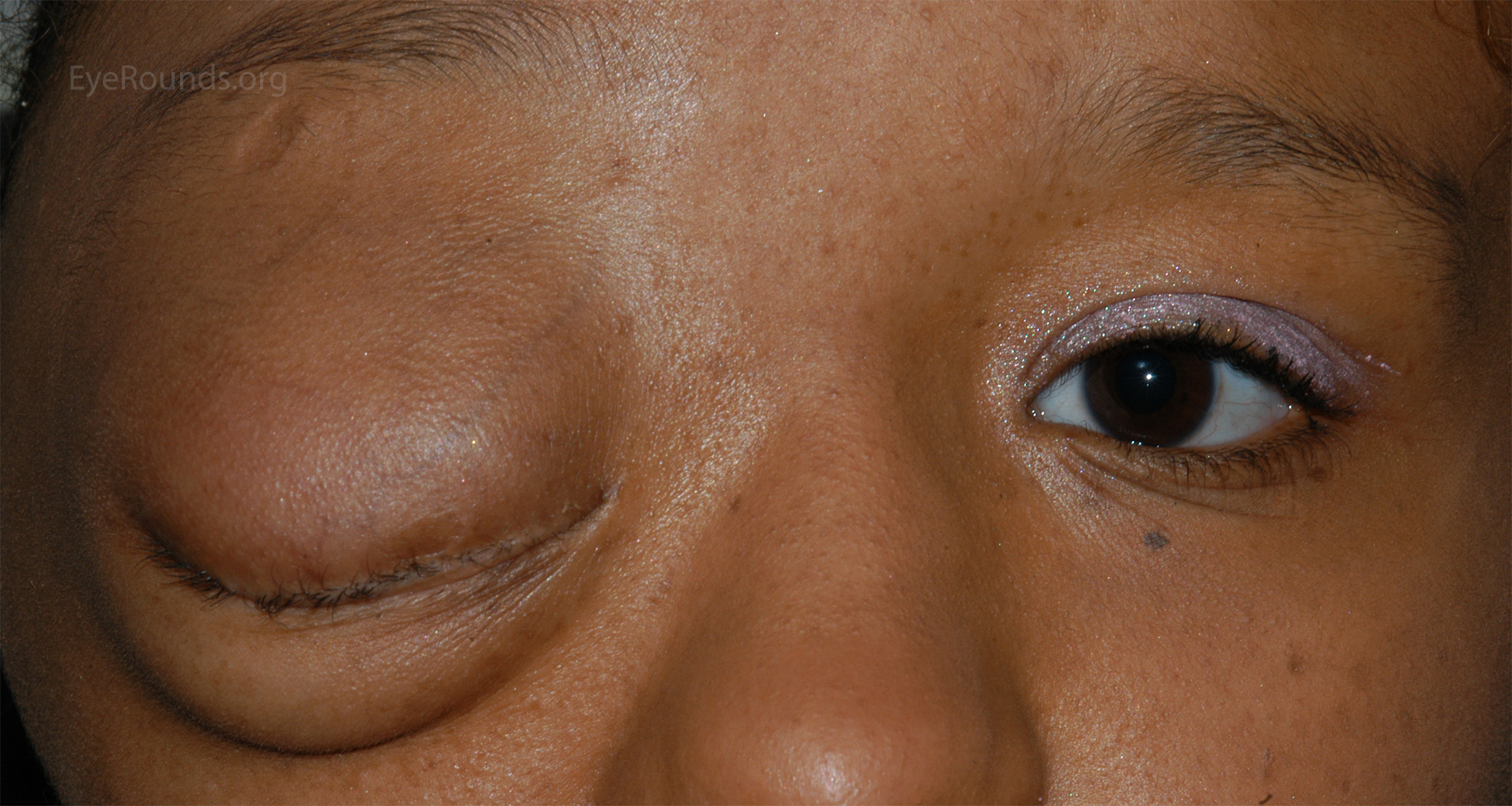
Mechanical ptosis is caused by excess weight of the upper lid. There are a multitude of causes that can be easily distinguished on physical exam. A few common causes are edema, inflammation, tumors, chalazia, dermoid cysts, neurofibromas, and amyloid deposits (Fig 6 & 7).

In cases of pseudoptosis the eyelid appears to be lowered but there is no pathology of the eyelid muscles or aponeurosis. A very common cause of pseudoptosis is dermatochalasis, or redundant eyelid skin, that droops beyond the eyelid margin creating the appearance of ptosis (Fig 8). If this skin is manually lifted, one can assess the position of the underlying eyelid margin to assess for the presence of true ptosis. Asymmetric lid heights due to unilateral upper lid retraction might give the impression of ptosis in the contralateral eye (Fig 9). Enophthalmos may also create the appearance of ptosis due to reduced upward forces on the eyelid. Hypotropia may also result in pseudoptosis due to connections from the superior rectus muscle to the upper eyelid (Fig 10).


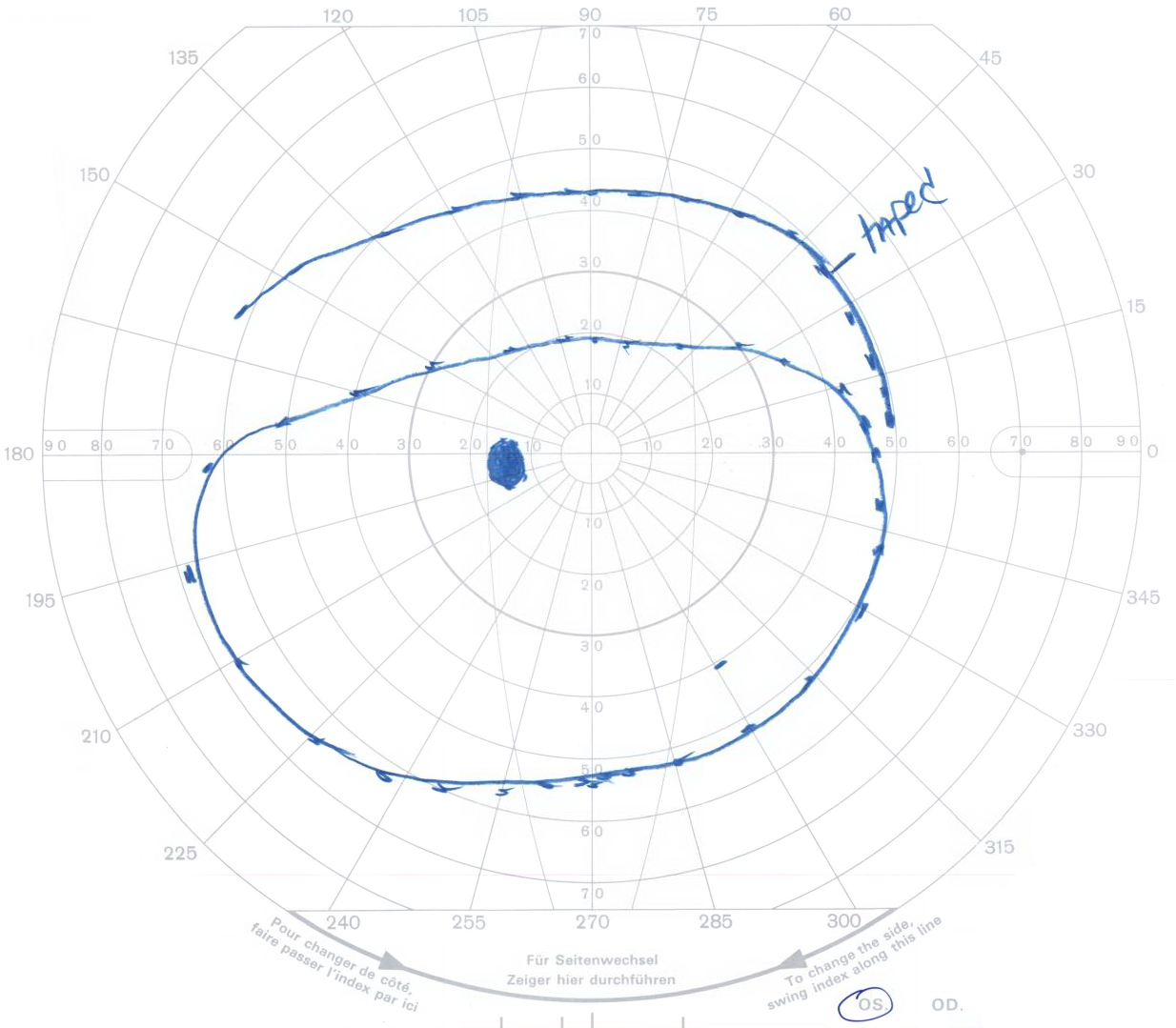
Surgery is appropriate for patients who have limited visual fields (Fig 11) or for cosmetic reasons. There are three surgical approaches to ptosis repair: Muller's muscle conjunctival resection (MMCR), levator advancement (Fig 12), and frontalis sling.
The MMCR procedure utilizes an internal approach to ptosis repair, thereby leaving no visible external scars after the procedure. Resection of Müller's muscle typically provides 1-2 mm of lift. After flipping the upper eyelid, the palpebral conjunctiva and Müller's muscle are resected and the resected ends are sutured together (Video 1). The advantages of MMCR include predictable results, lower rates of reoperation, rapid recovery, less post-operative bleeding, and no intraoperative adjustment (14). Phenylephrine drops, often used for pupillary dilation, are a sympathetic agonist and stimulate Müller's muscle. They are instilled during the pre-operative evaluation to approximate the results of an MMCR operation and determine if the procedure would provide sufficient lift.
This procedure has the ability to offer greater lift than MMCR and can be performed in patients who had unsatisfactory MMCR procedures in the past. An incision is made in the upper eyelid crease to expose the levator aponeurosis (Video 2). The aponeurosis is dissected off Müller's muscle, advanced toward the tarsal plate, and sutured in place. The height and contour of the eyelid can be adjusted intraoperatively after examining the lid appearance with the patient sitting upright. This procedure is effective in patients with at least moderate levator function as the levator muscle is still required to lift the eyelid. An eyelid with poor levator function is also at risk for recurrence of ptosis due to replacement of the normal muscle fibers with fat and fibrous tissue resulting in dehiscence of the suture (15)
Slings are indicated for patients with severe ptosis and poor levator function and for patients with progressive myogenic ptosis (OPMD, CPEO, and myotonic dystrophy). In this procedure the eyelid is suspended by either fascia lata (harvested from the thigh), suture, or alloplastic materials (such as silicone). The sling is sutured to the tarsus using an upper eyelid crease incision (Video 3). It is then passed under the fascia of the brow and secured to the frontalis muscle superiorly using three small incisions above the brow. The eyelid heights are adjusted intraoperatively and the slings are secured. A frontalis sling is indicated in patients with poor or absent levator function because the mechanical movement of the eyelid in such cases is effected solely by the frontalis muscle.
Klejch W, Vislisel JM, Allen RC. A Primer on Ptosis. EyeRounds.org. posted April 6, 2015; Available from: http://www.EyeRounds.org/tutorials/ptosis/