Chief Complaint: 38-year-old male presented with binocular vertical diplopia
History of Present Illness (History of Present Illness): The patient noted the sudden onset of vertical binocular diplopia which he noticed was greatest in left gaze and was relieved with a chin-up position. There was no history of trauma or any medical illness.
Medical History and Past Ocular History: Unremarkable
Family and Social History: Non-contributory
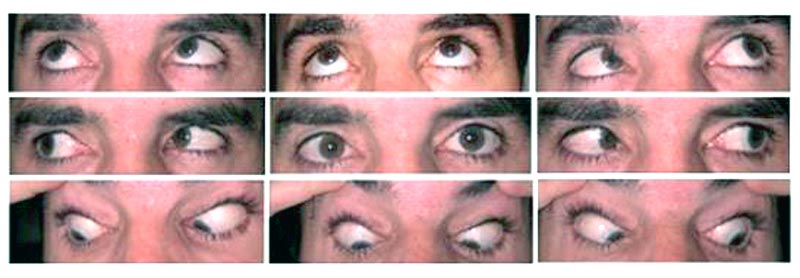 |
Course: The patient's symptoms and motility examination are consistent with restriction of motility involving the right superior oblique. This is in the same anatomical location where a soft, tender mass was noted. Magnetic resonance imaging (MRI) with contrast (see Figure 2) revealed an expansile, nonenhancing 3-4 cm mass of the right ethmoidal sinus with an intraorbital and extraconal extension consistent with a mucocele. The mass appeared to be pressing on the globe causing effacement of the right medial rectus and superior oblique tendon with anterolateral displacement of the trochlea.
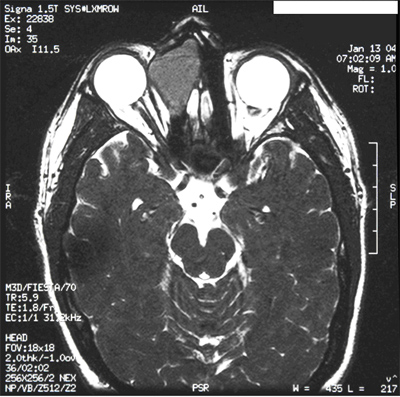 |
The cause of vertical binocular diplopia in this patient was a ethmoidal sinus mucocele pressing on the globe resulting in effacement of the superior oblique tendon with anterolateral displacement of the trochlea thus causing a limitation to elevation in adduction classically known as Brown Syndrome. Following endoscopic removal of the mass the patient was relieved of diplopia and ugze ability in adduction was improved, but moderately limited. The histopathology of the lesion was consistent with a mucocele.
Brown Syndrome was first characterized in 1950 by Harold Whaley Brown as a restrictive limitation to elevation in adduction. On the basis of surgical findings Brown implicated a shortened superior oblique (SO) tendon sheath as the cause of the syndrome. Most subsequent reports have alternatively proposed an abnormality in the trochlear-SO tendon complex as the etiology of restriction to elevation in adduction.
Various etiologies of acquired Brown Syndrome have been described including frontal sinus surgery (Rosenbaum et al, 1985), blepheroplasty (Levine et al, 1975), chronic sinusitis, trauma, inflammatory (Hermann, 1978), systemic lupus erythematosis (Whitefield et al, 1995), and restrictive fibrous bands. High-resolution MRI demonstrated varied abnormalities in both congenital and acquired Brown syndrome such as traumatic or iatrogenic scarring, avulsion of the trochlea, cyst in the superior oblique tendon, inferior displacement of the lateral rectus pulley and fibrous restrictive bands extending from the trochlea to the globe (Bhola et al, 2005).
According to the anatomic abnormalities noted by MRI, four distinct mechanisms of Brown syndrome have been identified: trochlear damage, superior oblique (SO) tendon abnormalities, abnormalities of rectus extra ocular muscle pulleys, and congenital abnormalities of superior oblique muscle (Bhola et al, 2005). MRI can delineate the pathological anatomical abnormalities causing Brown syndrome thereby individualizing surgical management without reliance on extensive exploratory surgery.
EPIDEMIOLOGYIncidence: 1 in 400-450 strabismus cases Etiology based on MRI:
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Bhola RL: Acute Acquired Brown Syndrome: 38-year-old Male with Ethmoidal Sinus Mucocele. Eyerounds.org. December 1, 2005; Available from: http://www.EyeRounds.org/cases/50-Acquired-Brown-Syndrome-Ethmoid-Mucocele.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.