Chief Complaint: "Double vision"
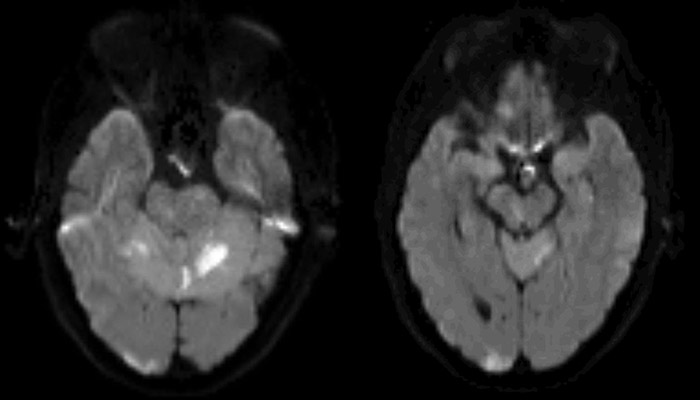
A 53 year-old female presents as a referral from her neurosurgeon with a complaint of double vision. It was acute in onset, painless, and first noticed two weeks prior, immediately upon awakening from a cerebral angiogram with aneurysm stenting and coiling. She has a history of a dissecting left posterior cerebral artery (PCA) aneurysm and underwent coil embolization 5 months prior to presentation. Unfortunately, only 80% of the aneurysm was coiled, which led to her repeat cerebral angiogram with stenting and re-coiling of the remaining aneurysm. The procedure was complicated by decreased flow in several of the posterior circulation arteries, a small thrombus at the origin of the left PCA, and a complicated deployment of the pipeline stent. Following the procedure, she was noted to have a deteriorating neurologic status and an MRI was obtained that showed multiple subacute infarcts in the bilateral thalami, right occipital pole, right paramedian midbrain, cerebellar vermis, and both cerebellar hemispheres (Figure 1).
 |
She complains of binocular diplopia that is vertical in nature. It has been constant and non-progressive since the onset. It is relieved with closing of either eye. The diplopia is unchanged in any particular gaze direction or head positioning and is similar for both distance and near.
 |
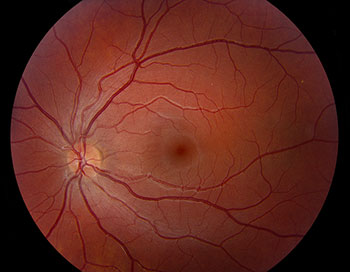 |
Right ocular tilt reaction – skew deviation, fundus torsion, and torticollis, secondary to posterior circulation infarction
The patient was able to achieve sensory fusion with 7 prism diopters of base down prism over her left eye. A Fresnel prism of this strength was placed on the left lens of her glasses. Given the comitant nature of her deviation, she was able to fuse well in all directions of gaze. She was scheduled to follow-up in the Neuro-ophthalmology clinic in 3 months time to assess for any change in her alignment or resolution of her diplopia.
A skew deviation is a vertical misalignment of the eyes that is caused by damage to the otolithic input to the ocular motor nuclei. When accompanied by binocular torsion, torticollis, and a tilt in the subjective visual vertical, it is termed the ocular tilt reaction. Lesions causing this are classically localized to the posterior fossa and can be from a variety of causes, but are many times a result of an acute lesion, such as ischemic stroke, demyelination, trauma, iatrogenic/post-surgical, hemorrhage, or tumor affecting the brainstem, cerebellum, or vestibular structures or pathways. It is thought that the ocular tilt reaction is likely a vestigial remnant of the primitive otolithic righting reflex that is tonically suppressed under normal physiologic conditions in frontal-eyed species (i.e., humans) in the interest of single binocular vision and only becomes manifest in the presence of pathology.
The vestibular system plays a major role in control of head-eye posture in the roll plane – the plane in which the head or body tilt or rotate from side to side. The vestibulo-ocular system has a primary function to maintain eye position and stabilize fixation during movements of the head or whole body in this plane. In the labyrinth of the inner ear, the semi-circular canals sense angular acceleration while the otoliths (saccules and utricles) sense linear acceleration of the head in space. Bilateral input from these structures projects to the central vestibular system that in-turn modulates extraocular muscle tone (via the vestibulo-ocular reflex) to maintain eye position and stable foveation during changes in head position. Input from this system also plays a role in spatial perception and in postural tonus of the head and body (via the vestibulo-spinal reflex).
Under normal physiologic conditions, a change in head or body position in the roll plane initiates asymmetric sensory input from the vertical semicircular canals and utricle to the central vestibular system as a response. For example, consider a leftward body tilt in the roll plane (Figure 4). Physiologically, this would initiate a compensatory rightward ocular tilt reaction. If the body is tilted to the left, it causes the left eye to be lower in space than the right. The compensatory skew deviation will cause subsequent upward rotation of the lowermost left eye and downward rotation of the uppermost right eye to realign them. Also, when the body is tilted to the left, there is a torsional deviation of both eyes toward the left. The compensatory ocular counter-roll results in incyclotorsion of the left eye and excyclotorsion of the right eye relative to the head, so that there is no torsion of the eyes relative to space. The third component of the physiologic ocular tilt reaction is the compensatory head tilt or torticollis that will more closely realign the head with the gravitational vertical. In the example of a leftward body tilt in the roll plane, this will result in a compensatory rightward head tilt.
In a pathologic ocular tilt reaction, a unilateral lesion (or stimulation) of the utricle or its pathways will result in asymmetric vestibular input to the central nervous system (CNS) that mimics a change in body position in the roll plane as sensed by the CNS (Figure 4). This will result in two main findings: 1) an ocular tilt reaction in the absence of any true body tilt in the roll plane - this can be tonic or paroxysmal and can be a complete ocular tilt reaction or partial with only certain components becoming manifest (i.e., only a skew deviation or only synkinetic ocular torsion), and 2) a tilt in the subjective visual vertical – a perception by the patient that vertical orientation is different from what is true vertical. Patients are usually asymptomatic from this and do not perceive a tilt in their perception of the world until placed in artificial testing situations that eliminate external cues. Given that the ocular torsion is in the same direction as the patient's perception of vertical, it is thought that this may be the driving force for all components of the ocular tilt reaction – to realign the eyes and body with the subjective and CNS perception of true gravitational vertical.
The otolithic and graviceptive pathways that mediate vestibular input and modulate the vestibulo-ocular reflex begin peripherally with sensory organs of the otoliths in the labyrinth of the inner ear and project to the ipsilateral vestibulocochlear nucleus (CN VIII) at the ponto-medullary junction via the vestibular portion of CN VIII (Figure 5). This pathway then decussates to the contralateral side at the level of the pons to ascend the brainstem in the medial longitudinal fasciculus (MLF) to the supranuclear centers for vertical-torsional eye movements in the rostral midbrain. The rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) contains the excitatory burst neurons that generate vertical and torsional saccades. The interstitial nucleus of Cajal (INC) contains the inhibitory burst neurons for vertical and torsional saccades and also acts as the neural integrator for vertical and torsional gaze holding; it likely plays a major role in producing the ocular tilt reaction. These nuclei send signals to the ocular motor nuclei (oculomotor nucleus (CN III), trochlear nucleus (CN IV) and abducens nucleus (CN VI)) that will in-turn modulate extraocular muscle tone and eye position.
Knowing the above anatomy of the pathway can help with localization of a causative lesion. For example, diminished input from the right utricle anywhere along the pathway will cause asymmetric vestibular input from the right and will result in the CNS perception that the head is being tilted to the left in the roll plane thereby producing a right ocular tilt reaction (Figure 5). The causative lesion will be ipsilateral if it is located caudal to the decussation of the otolithic pathway in the pons and will be contralateral if is located rostral to the decussation. For example, an ipsilateral ocular tilt reaction can occur with lesions of the utricle/labyrinth, vestibular nerve, or lateral medulla (i.e., in Wallenberg syndrome) that are all caudal to the decussation of the graviceptive pathway fibers in the pons; a contralateral ocular tilt reaction can occur with lesions that affect the rostral pons, MLF (i.e., in conjunction with internuclear ophthalmoplegia), the midbrain or INC (i.e., in dorsal midbrain syndrome) that are all rostral to the decussation of the graviceptive pathway fibers in the pons. There are a variety of etiologies that can affect these areas, but, as stated previously, stroke, demyelination, trauma, iatrogenic/post-surgical, and tumor are common etiologies. Furthermore, there are multiple otolithic projections to the cerebellum. Lesions of the cerebellum are also known to cause complete or partial ocular tilt reactions.
Patients with lesions affecting the otolithic input to the ocular motor nuclei do not always present with the entire spectrum of the ocular tilt reaction (i.e., skew deviation, ocular torsion, and torticollis), but can present with variable components and severity of each. An isolated skew deviation typically presents as a fairly comitant, acquired, vertical misalignment of the eyes with a full range of extraocular movements. There is usually some degree of incyclotorsion of the hypertropic eye or excyclotorsion of the hypotropic eye (or both), which help differentiate it from CN IV palsy. These patients typically report vertical diplopia. There are variations of skew deviation including comitant, incomitant, paroxysmal, periodic alternating, lateral alternating, and transient neonatal that will not be discussed in this article. As discussed above, synkinetic cyclorotation of the eyes and a tilt in the subjective visual vertical may be asymptomatic to patients, and can easily be missed on examination unless specifically sought.
The direction of torsion of the eyes will be the same as the direction of the ocular tilt reaction (i.e., in a right ocular tilt reaction there will be incyclotorsion of the left eye, excyclotorsion of the right eye, or both – torsion of the eyes to the right). This is also true of the head tilt (i.e., a right ocular tilt reaction will have a right head tilt). The hypotropic eye in the skew deviation will correspond to the side of the ocular tilt reaction (i.e., a hypotropic right eye will be present in a right ocular tilt reaction with a corresponding skew deviation).
The majority of ocular tilt reactions are transient with spontaneous recovery in many cases. As a temporizing symptomatic measure, the vertical diplopia can be treated with prisms and is typically very amenable to this therapy given the comitant nature of the vertical deviation. Botulinum toxin injections into the extraocular muscles have also been used with some success. In patients with persistent skew deviation with vertical diplopia, prism, repeated botulinum toxin, or strabismus surgery (typically vertical rectus muscle recession) can be offered. It is important to note that these treatments will not eliminate the head tilt component of the ocular tilt reaction, as this, along with the synkinetic ocular torsion, are a compensatory mechanism to realign the head and eyes with gravitational vertical.
Etiology
|
Signs
|
Symptoms
|
Treatment
|
Kirkpatrick CA, Thurtell MJ. Ocular Tilt Reaction: 53-year-old female complaining of vertical diplopia following a stroke and found to have a skew deviation, fundus torsion, and torticollis. Dec 31, 2014; Available from: https://eyerounds.org/cases/200-OTR.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.