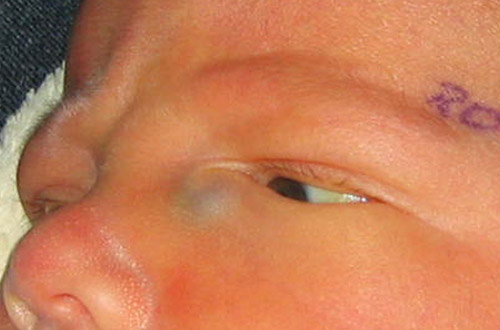
Chief complaint: Full-term 10 day-old female referred to the pediatric ophthalmology clinic by dermatologist for a bluish mass inferior to the right medial canthus.
History of present illness: Initially a cystic lesion was noted on the fetus' face on a 28-week ultrasound. At birth, an elevated, bluish lesion was noted just inferior to the right medial canthus. The lesion did not seem to bother the patient, and it had not changed in size or appearance since birth. The local pediatrician was concerned it was a hemangioma and referred the patient to dermatology. Dermatology subsequently evaluated the patient and referred her to pediatric ophthalmology for further management.
Past Ocular History: Unremarkable
Past Medical History: Unremarkable
Medications: None
Allergies: No known drug allergies
Family History: No known eye disease
 |
 |
A. External exam of infant. Note the purplish swelling inferior to the medial canthal tendon. |
B. The mass is causing upward slanting/displacement of the palpebral fissure nasally. |
The clinical exam features were felt to be classic for and consistent with a congenital dacryocystocele. An examination under anesthesia and probing of the lacrimal system on the right side was planned for three days later. The patient was started on oral Augmentin (amoxicillin/clavulanate), due to concern for early infection of the dacryocystocele.
On the morning of the procedure, the child was seen in the pre-operative area. The mother reported that the prior evening, there had been a large amount of discharge from the medial canthal area, and the swollen, blue cystic area had spontaneously decompressed.
Given that the dacryocystocele had spontaneously decompressed, probing of the nasolacrimal system was deferred. Tobradex (tobramycin/dexamethasone ophthalmic suspension) drops four times a day to the right eye were prescribed for prophylaxis. The child was to follow-up in clinic in one week for further evaluation. No further complications or problems occurred in this infant.
Presentation of congenital dacryocystocele
Congenital dacryocystocele, also known as a dacryocele, often presents shortly after birth. It is an infrequent variant of nasolacrimal duct obstruction (NLDO) and found in only about 1.0% of infants with congenital NLDO.[1]
Congenital dacryocystocele often presents as a bluish, cystic, firm mass inferior to the medial canthus. One study cited the median age of presentation as 7 days of life.[2] It is most commonly unilateral but may be bilateral. Multiple studies have found that the condition is more common in females than in males, secondary to females having a more narrow nasolacrimal duct than males.[2]
Patients with a dacryocystocele may have difficulty breathing or develop infection of the site. Parents may notice that the child has difficulty breastfeeding and develops respiratory difficulty when feeding on the breast ipsilateral to the dacryocystocele.[2]
Often, the diagnosis of congenital dacryocystocele can be made based on clinical findings alone. However, if the diagnosis is in question, a computed tomography (CT) scan or magnetic resonance imaging (MRI) can be used to confirm the diagnosis. Interestingly, the diagnosis can also be made prenatally with ultrasonography.[3] Items that should be considered in the differential diagnosis include: encephalocele, meningocele, and encephalomeningocele. These generally occur superior to the medial canthus, however. These are potentially life-threatening diagnoses that should be promptly evaluated.
Congenital dacryocystocele can be considered a subcategory of congenital NLDO. In both, there is improper drainage of tears; however, they differ in the site of the blockage. In NLDO, the blockage generally occurs distally at the valve of Hasner. Thus, there is backlog of the drainage system leading to a watery eye and epiphora. With a dacryocystocele, there is a functional blockage proximally as well as a blockage distally. This leads to fluid accumulation (amniotic fluid and mucous produced by the lacrimal sac glands) causing distention (Figure 2). The proximal blockage is thought to be caused by failure of the mesoderm to properly canalize during development.[2]
 |
Treatment options for dacryocystocele range from conservative, non-surgical management (massage, observation) to surgical (probing of nasolacrimal system).[3] Initially conservative measures should be tried. This includes digital massage over the area of elevation and prophylactic topical antibiotics. If no response to treatment is seen within 1-2 weeks, probing and irrigation of the lacrimal system either in the clinic or operating room is recommended (Figures 3 and 4). One study reported that approximately 22% of cases spontaneously resolved, while the remainder required surgical intervention.[2]
Should the dacryocystocele progress to dacryocystitis, antibiotics are indicated.[2] As children who develop dacryocystitis are often one month of age or younger, admission to the hospital may be recommended depending on age, medical co-morbidities, and follow-up. Sepsis is a life threatening complication if the infection goes without treatment. If there is an intranasal component (endonasal cyst), marsupialization of the cyst is recommended, and an otolaryngology consult may be appropriate depending on the surgeons experience.[4]
There are several complications that can occur as a result of a dacryocystocele. These include: dacryocystitis, cellulitis, and respiratory compromise. In cases of infection, the child may experience life-threatening sepsis. Therefore, it is important if the child develops concurrent dacryocystitis and cellulitis that they be hospitalized for observation and administration of intravenous antibiotics.[3] Once the infection subsides, probing with or without stent placement is advised.
Rarely, dacryocystocele can be associated with an intranasal cyst. If one opts to try conservative management initially, these children must be monitored for signs of infection or breathing difficulty. Consultation with an otolaryngologist or endoscopic nasal endoscopy should be performed at the time of probing. Should any of the above complications occur, prompt management (antibiotics, probing, surgery) is required.[2]
| A. Decompression of dacryocystocele in the operating room. |
|---|
 |
| B. Subsequent probing and irrigation. |
 |
 |
Diagnosis: Congenital Dacryocystocele
Epidemiology
|
Signs
|
Symptoms
|
Treatment
|
Differential Diagnosis
|
Complications
CT or MRI should be performed if more serious etiology suspected |
Gauger EH, Longmuir SQ. Congenital dacryocystocele with spontaneous resolution. EyeRounds.org. March 7, 2013; available from: http://www.EyeRounds.org/cases/166-dacryocystocele.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.