
The University of Iowa
Department of Neurology and Department of Ophthalmology and Visual Sciences
Optic neuritis is the inflammation of the optic nerve. It can occur secondary to autoimmune, infectious, or inflammatory disorders and is strongly associated with multiple sclerosis (MS). It is the presenting symptom in 15-20% of cases of MS, but frequently occurs in the absence of MS.[1] In addition, 65% of patients with multiple sclerosis will suffer from optic neuritis at some point during the course of the disease.[2] Optic neuritis causes substantial visual impairment and potential long-term visual defects in addition to serving as an important prognostic indicator for future development of demyelinating diseases such as multiple sclerosis. Fortunately, in most cases, optic neuritis recovers either spontaneously or with treatment. Recovery can be partial or absolute, depending largely upon severity and co-existing conditions.
It typically affects younger individuals with a median age at onset in the early thirties, but has been reported in patients as young as four. It has an estimated annual occurrence rate of 5.1/100,00 in the United States, and is more commonly seen in women than in men.[3] Much of the information regarding the natural history of optic neuritis, its treatment, and its relationship with multiple sclerosis has been acquired from the Optic Neuritis Treatment Trial (ONTT). This was a large clinical trial that followed optic neuritis patients over time which allowed for evaluation of the natural history of the disease and response to corticosteroid treatment.[4] This review will focus on demyelinating optic neuritis, as this is the most common type of optic neuritis.
The pathophysiology of optic neuritis is not entirely understood. It is believed to be an inflammatory immune response that leads to demyelination of nerve axons which in combination leads to poor nerve conduction. The longer the portion of optic nerve that is involved, the more likely there is to be a conduction deficit, which is why involvement of longer portions of the nerve result in poorer visual outcomes.[5] Increased systemic and CSF T-cell activity has been documented in patients with active optic neuritis, suggesting T-cell involvement in the disease process.[6]
Many cases of optic neuritis resemble MS in their pathophysiology, and are believed to be autoimmune in nature. In these patients, CD4+ T cells which are specific for myelin become activated in the periphery and are able to cross the blood-brain barrier. These CD4+ T-cells then recruit other cells such as macrophages and granulocytes which contribute to the inflammatory response and ultimately degrade myelin. TH17 cells also appear to play a role by increasing inflammation through the release of various cytokines such as IL-17.[7]
There may also be a vascular component to the pathophysiology as 25% of patients with optic neuritis demonstrate blood vessel abnormalities such as inflammatory cells in the media. In addition, patients with vascular changes have a higher risk of developing MS.[8]
Un-myelinated axons of retinal ganglion cells converge like spokes of a wheel at the optic disc to form the optic nerve. The axons of the optic nerve become myelinated immediately posterior to the optic nerve head. The optic nerve leaves the orbit via the optic canal through the sphenoid bone and continues to the optic chiasm. At this point the fibers conducting signals from the nasal fibers (temporal visual fields) decussate, whereas those carrying information from the temporal retina (nasal visual fields) continue to travel ipsilaterally. The fibers after the chiasm are called the optic tract, which synapses in the lateral geniculate bodies of the thalamus before the visual information is then conducted to its final destination in the occipital cortex. Optic neuritis is a condition that affects the optic nerve, thus the myelinated nerve fibers that run from the optic disc to the optic chiasm. [9] In rare cases the optic tract may be affected.
Optic neuritis is most commonly associated with the symptoms of vision loss and eye pain. Pain is present in many cases of optic neuritis (92% according to ONTT) and is usually most prominent with eye movement. Vision loss typically occurs over a period ranging from a few hours to days with a wide variety of visual field defects that can be seen; ranging from diffuse visual field loss to a cecocentral scotoma (a scotoma involving both the central vision and the natural blind spot simultaneously). Altitudinal defects have been reported, but are more typical of an ischemic optic neuropathy. In the ONTT vision decreased to a median of 20/60 initially and the majority of patients returned to 20/20 within one month. Although visual acuity typically returns to near normal, visual changes such as diminished color perception and decreased acuity in dim light often persist.[1]
The diagnosis of optic neuritis can typically be made on the basis of a thorough history and ophthalmologic exam. Almost all patients will possess an afferent pupillary defect, and about a third of patients will have disc edema at presentation, which is usually mild and easily missed. Disc edema is typically seen in patients with involvement of the bulbar portion of the optic nerve, whereas its absence suggests involvement of the intracranial portion. The presence of hemorrhages around the disc is rare and decreases the likelihood of optic neuritis as the diagnosis.[1]
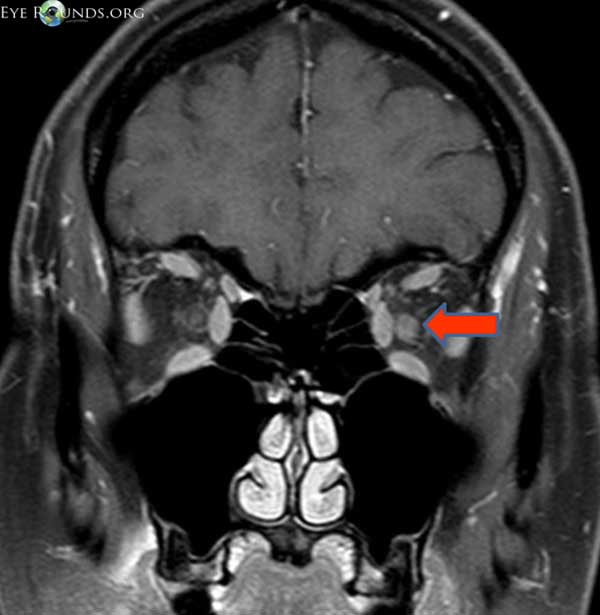
Most patients also receive gadolinium-enhanced magnetic resonance imaging (MRI) which serves two purposes. The first is to differentiate optic neuritis from other potential diseases of the optic nerve. The vast majority of patients will show enhancement of the optic nerve in a contrast enhanced MRI (Figure 1). This enhancement can occur in both the intrabulbar and intracranial portions of the nerve.[10]
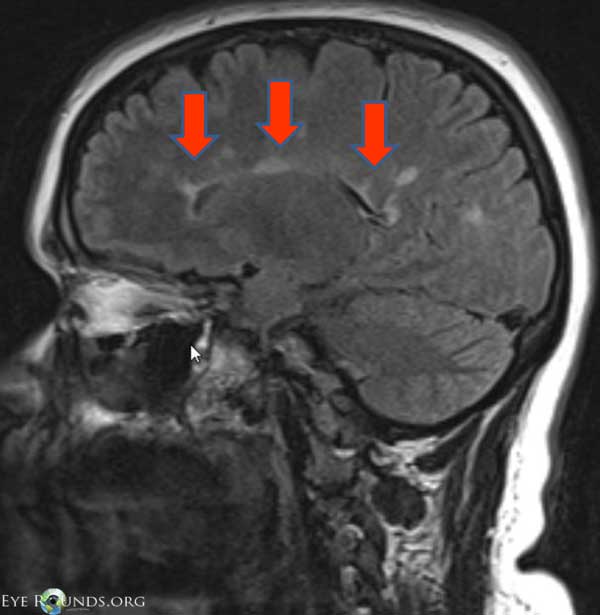
The second purpose of an MRI scan is to evaluate the risk of progression to MS. The ONNT showed that up to 50% of patients with optic neuritis will go on to develop multiple sclerosis. This trial also demonstrated that in patients with white matter lesions on MRI around 72% eventually developed multiple sclerosis versus only 25% of those with no white matter lesions, thus giving MRI an important role in determining risk of MS development (Figure 2).[11]
Most patients (>85%) with optic neuritis will have a final visual acuity in the affected eye of 20/25 or better with less than 1% of patients being legally blind in that eye. Visual symptoms are typically actue in onset and progress over the first couple of weeks. The majority of patients will begin to show rapid improvement in vision beginning in the 3rd or 4th week. Improvements can continue to be seen up to one year after the onset of optic neuritis.[12] After optic neuritis, atrophy and pallor of the nerve can be seen after 4 to 6 weeks. Some degree of atrophy of the nerve is seen even in patients with good visual recovery.
About 35% of patients will experience recurrent optic neuritis. Patients with optic neuritis who develop MS typically have a worse visual prognosis and a higher rate of recurrence.[13]
Treatment with intravenous (IV) followed by oral corticosteroids has been shown to decrease the amount of time required to recover visual acuity; however, the end visual acuity of patients treated with corticosteroids is not significantly different from those treated with placebo. Treatment with steroids also does not seem to decrease the percentage of patients who will go on to develop MS in the long-term. Interestingly, treatment with oral corticosteroids alone was found to increase the rate of recurrent optic neuritis and is therefore not recommended.[14]
The decision to treat is left to the physician and their patient who must weigh the benefit of a faster recovery of visual function with the potential adverse effects of systemic corticosteroid treatment. At the University of Iowa, we typically treat most cases of optic neuritis according to ONTT with a course of IV corticosteroids followed by oral prednisone. If there are white matter lesions on MRI at presentation, we refer the patient to neurology for continued surveillance for possible MS. With the introduction of MS treatment options, it appears that fewer recurrences of optic neuritis are observed in this group.