
Atropine sulfate is a muscarinic antagonist that blocks the action of acetylcholine, allowing for the radial pupillary dilatory muscle to contract. A1% (at 1% concentration) results in mydriasis (dilation) and loss of accommodation. Administered topically to the eye, atropine has an effect that lasts up to two weeks, making it optimal for therapeutic use. As an alternative to patching, atropine is used as pharmacologic penalization of the better seeing eye in the setting of amblyopia (1). It may also be utilized to produce mydriasis and/or cycloplegia (2). Low dose atropine (e.g., 0.05%) has been proven to be effective in the prevention of myopia (3).
References:
Hemoglobin A1C is the most widely used clinical measure of blood glucose levels. As such, hemoglobin A1C provides an important measure for diagnosis and monitoring of diabetes and may be an important predictor of retinopathy. A1C values above 6.5% are often considered abnormal, suggesting chronic hyperglycemia (4). Increased hemoglobin A1C levels are associated with increased microvascular complications of diabetes, including neuropathy, nephropathy, and retinopathy (5). Intensive glycemic control should be encouraged since lower A1C levels decrease the progression of diabetic retinopathy (6).
References:
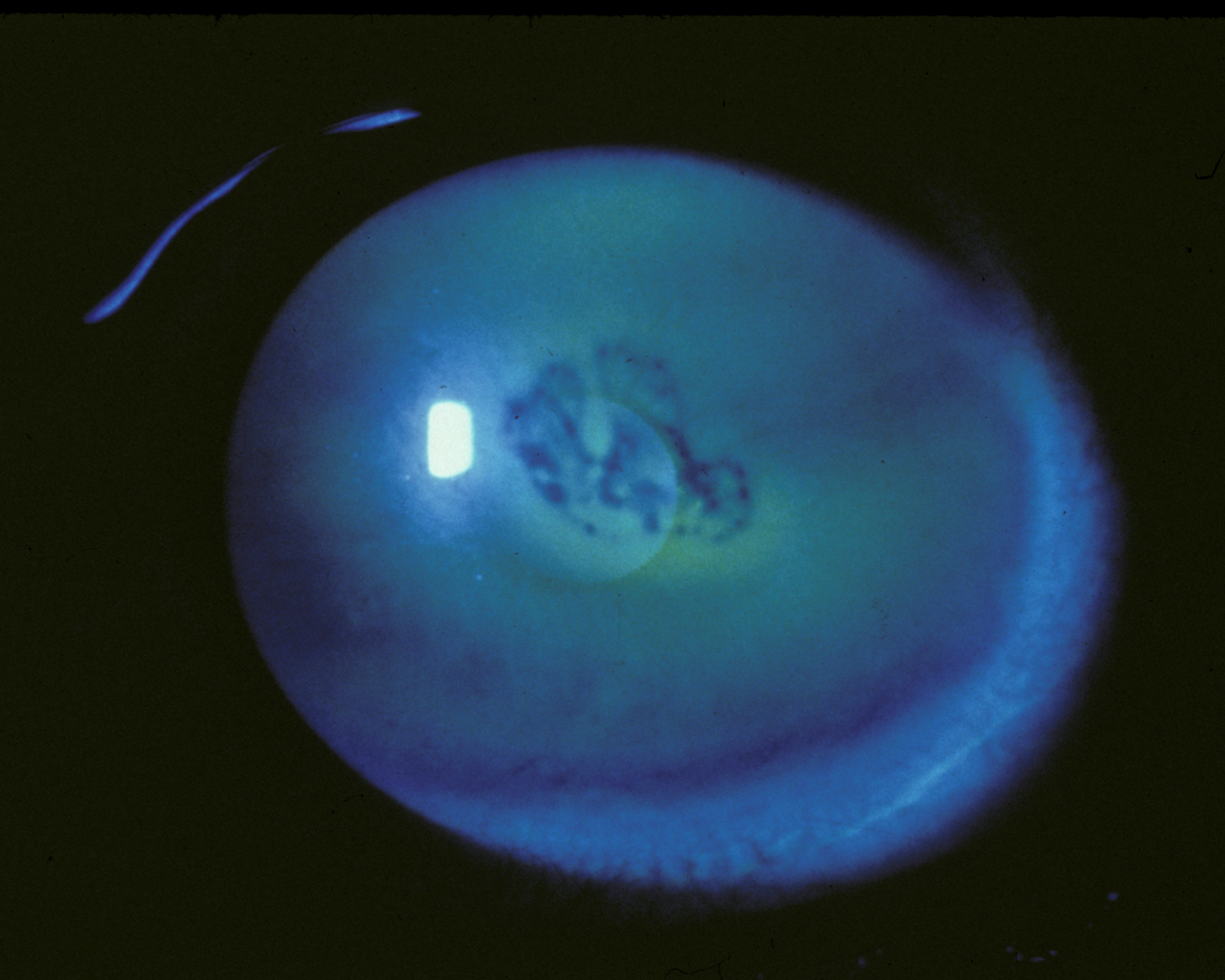
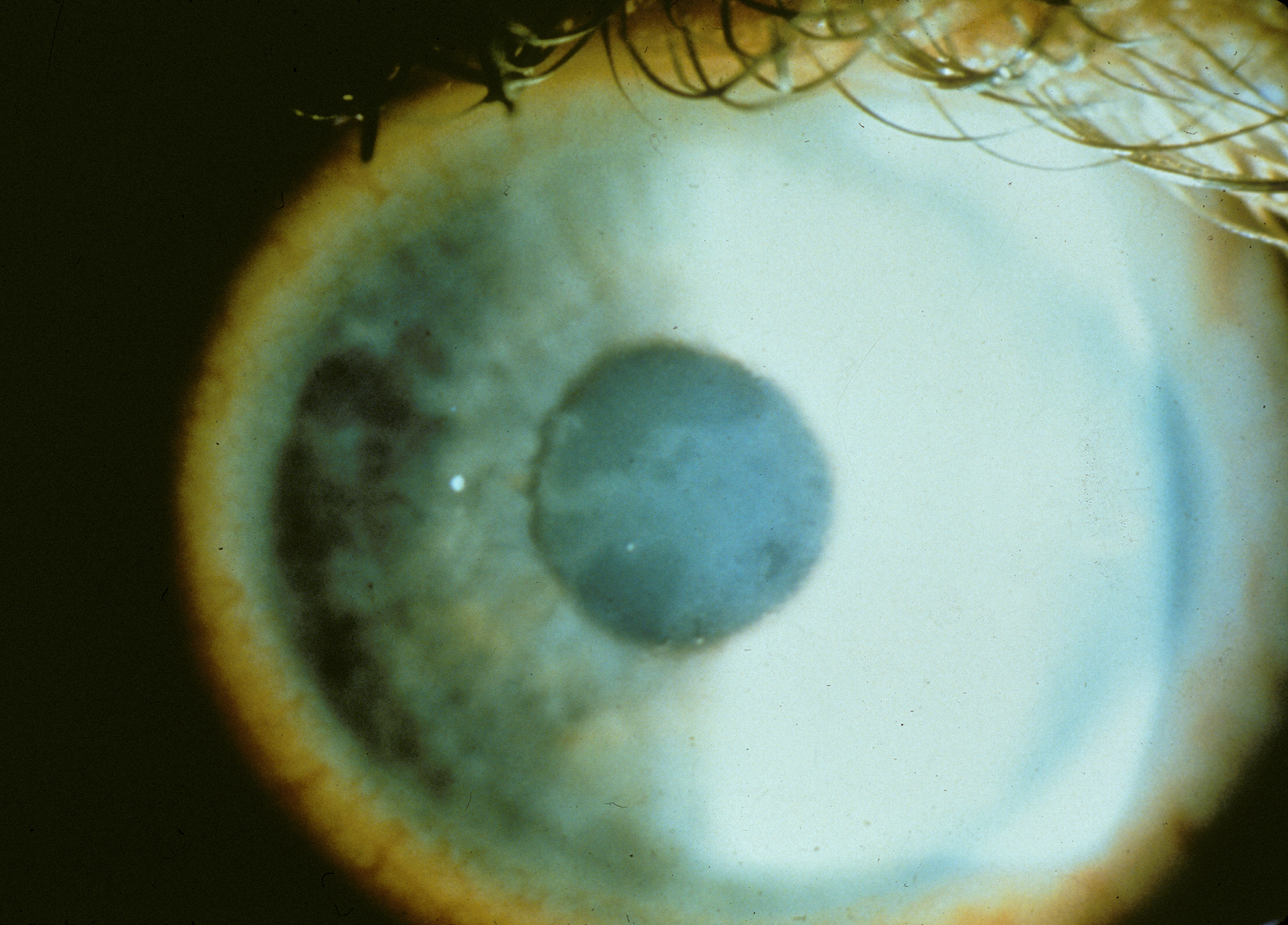
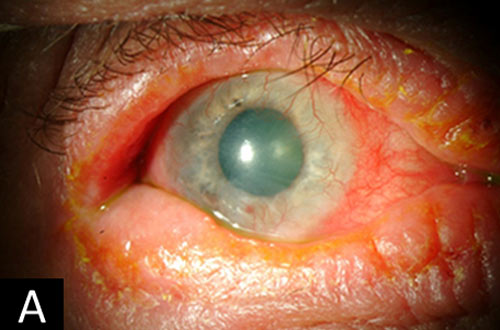
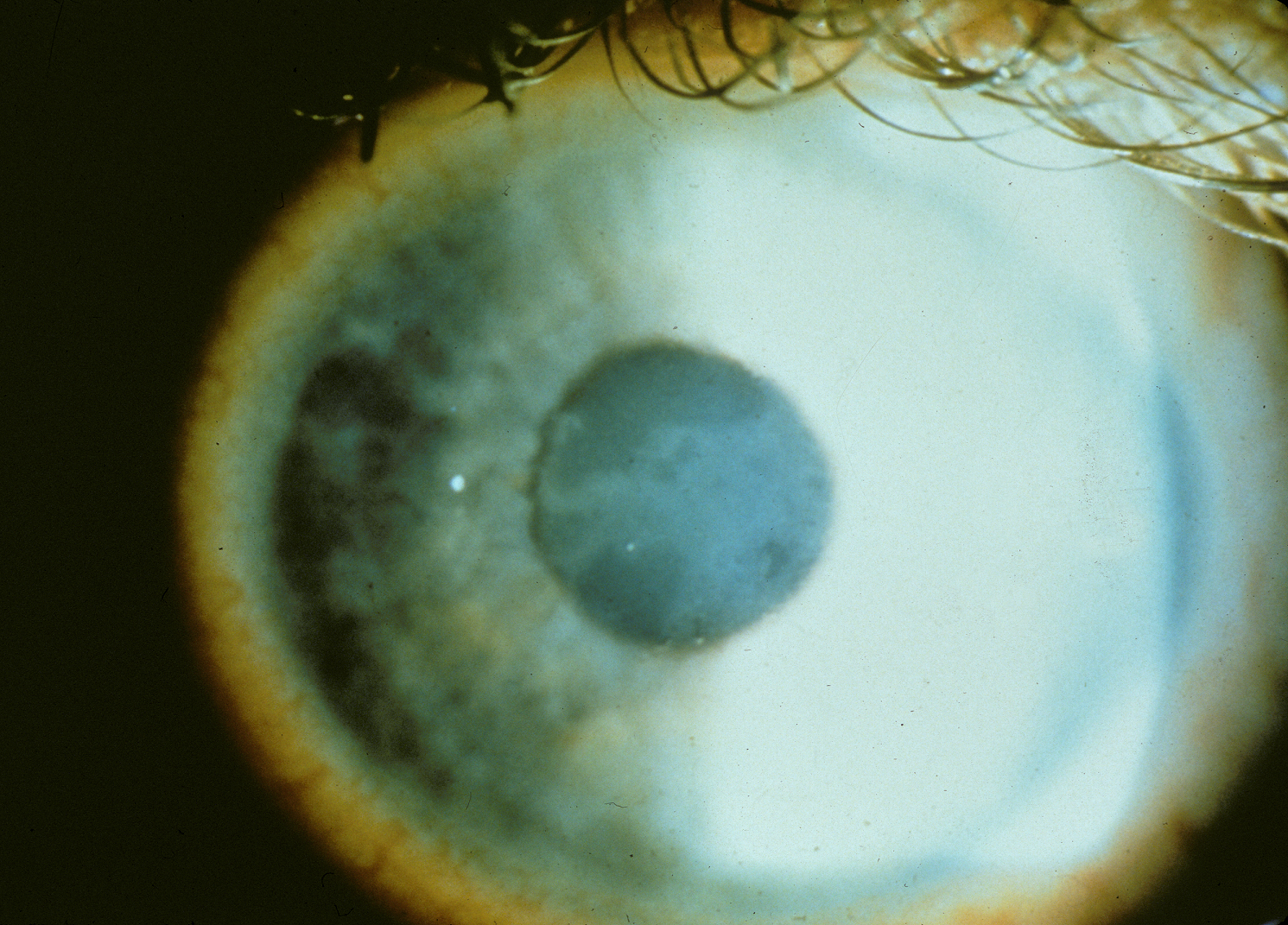
Acute angle closure glaucoma occurs when aqueous humor is trapped behind the iris, causing the iris to bow forward and block the outflow of aqueous humor through the trabecular meshwork. This results in a sudden increase in intraocular pressure, which can lead to permanent vision damage. Typical symptoms of acute angle closure glaucoma include eye pain, nausea, headaches, halos around lights, and blurred vision. Diagnosis may be made with gonioscopy examination of the anterior chamber angle, slit-lamp examination, and/or automatic static perimetry. Treatment includes pharmaceutical or surgical interventions to lower intraocular pressure (7). See below links for further information regarding diagnosis and management.

References:
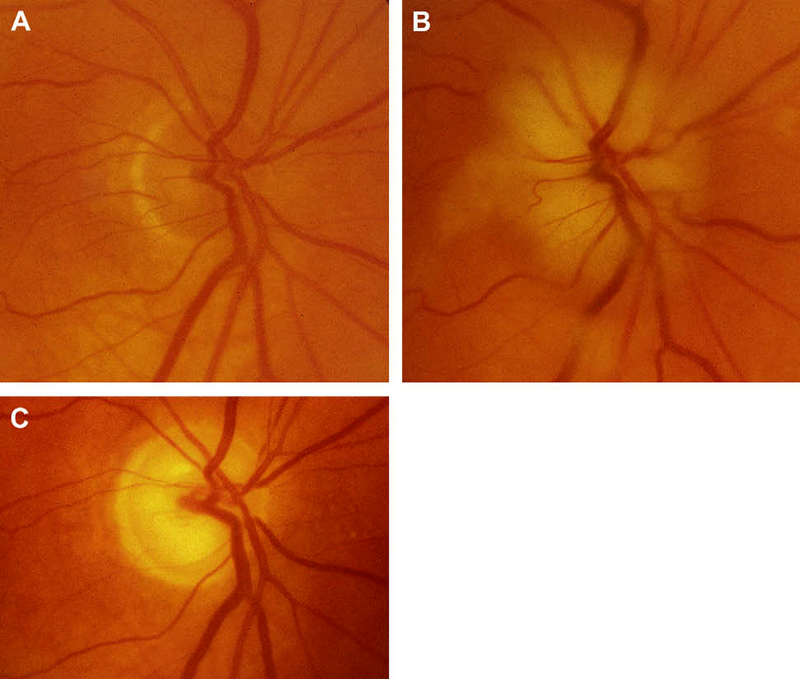
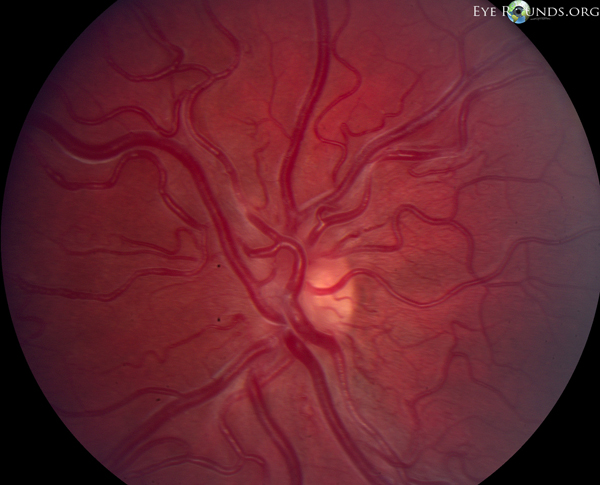
Arteritic anterior ischemic optic neuropathy is an acute and often painful optic neuropathy commonly occurring in patients over age 50. The condition results from acute ischemia of the optic nerve head as a result of giant cell arteritis, a systemic vasculitis that preferentially involves medium-sized and large arteries. Most often, this may involve the posterior ciliary artery, the main source of blood supply to the optic nerve head. Symptoms include transient visual loss, diplopia, and ocular pain, as well as systemic symptoms, such as anorexia, weight loss, jaw claudication, headache, scalp tenderness, abnormal temporal artery, neck pain, myalgia, malaise, and anemia. Ultimately, arteritic anterior ischemic optic neuropathy may result in permanent vision loss. Management primarily involves treatment of giant cell arteritis with immediate and adequate steroid therapy (8). Discussion of diagnosis by temporal artery biopsy and management of A-AION can be found in the below links.
References:
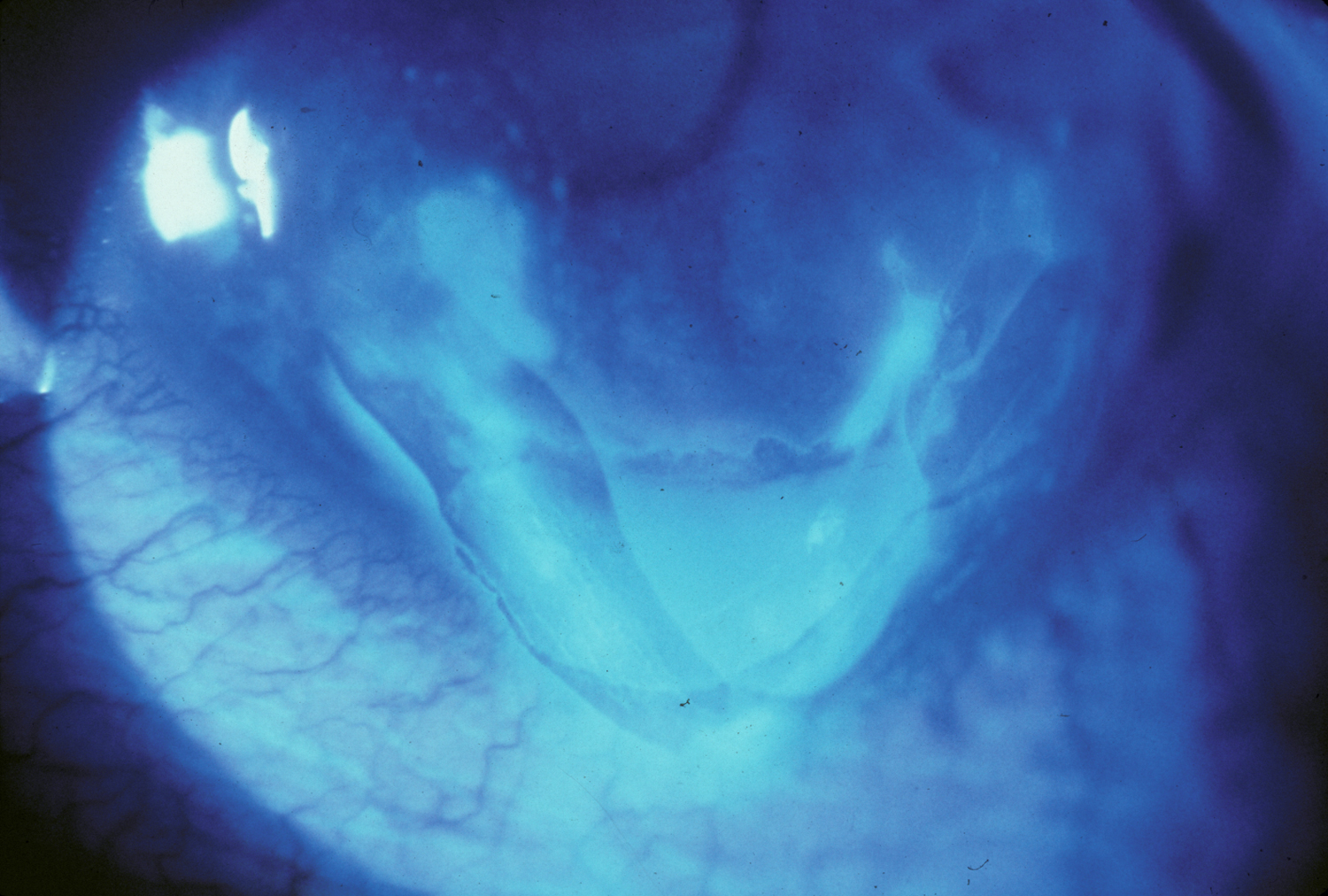
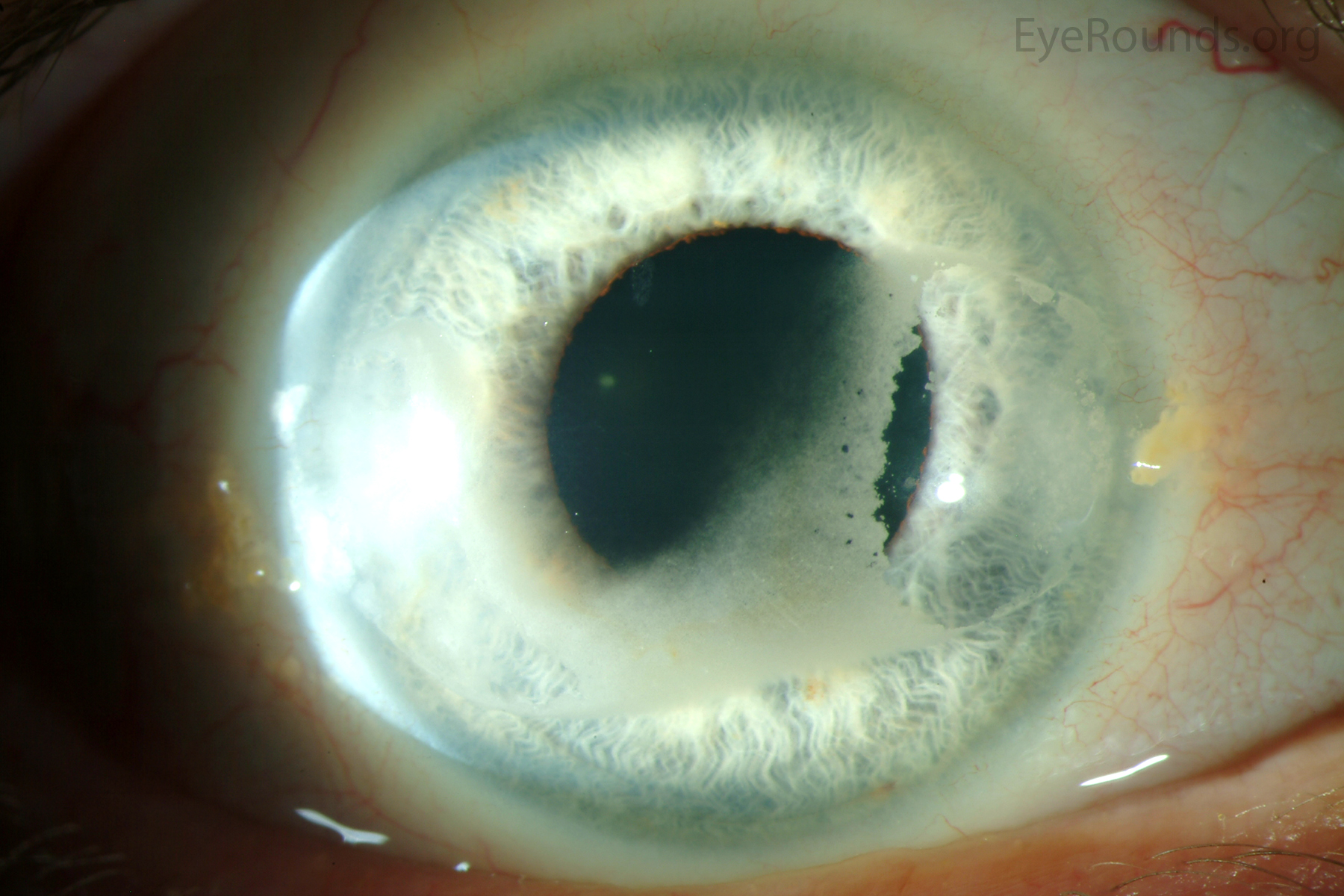
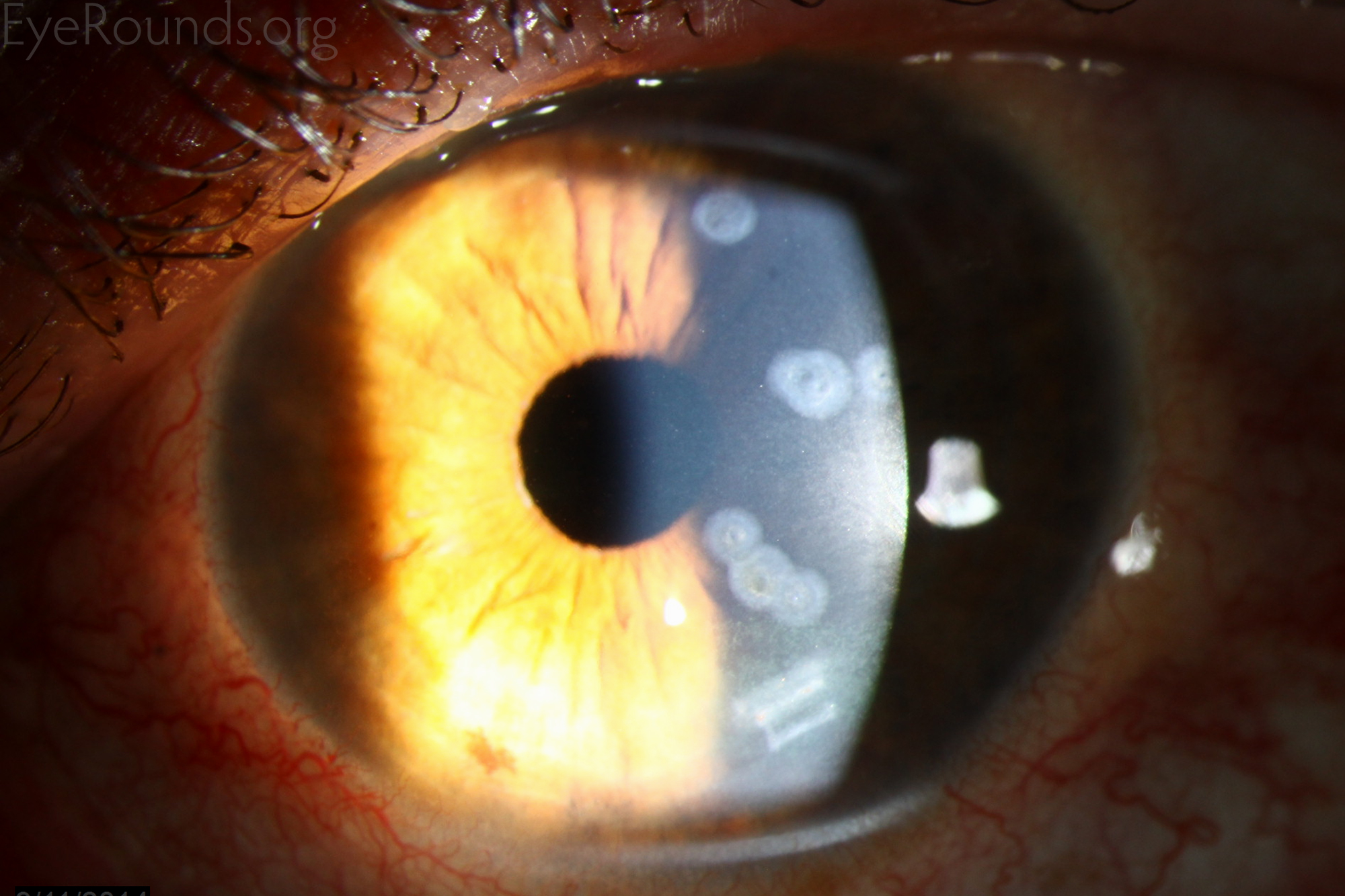
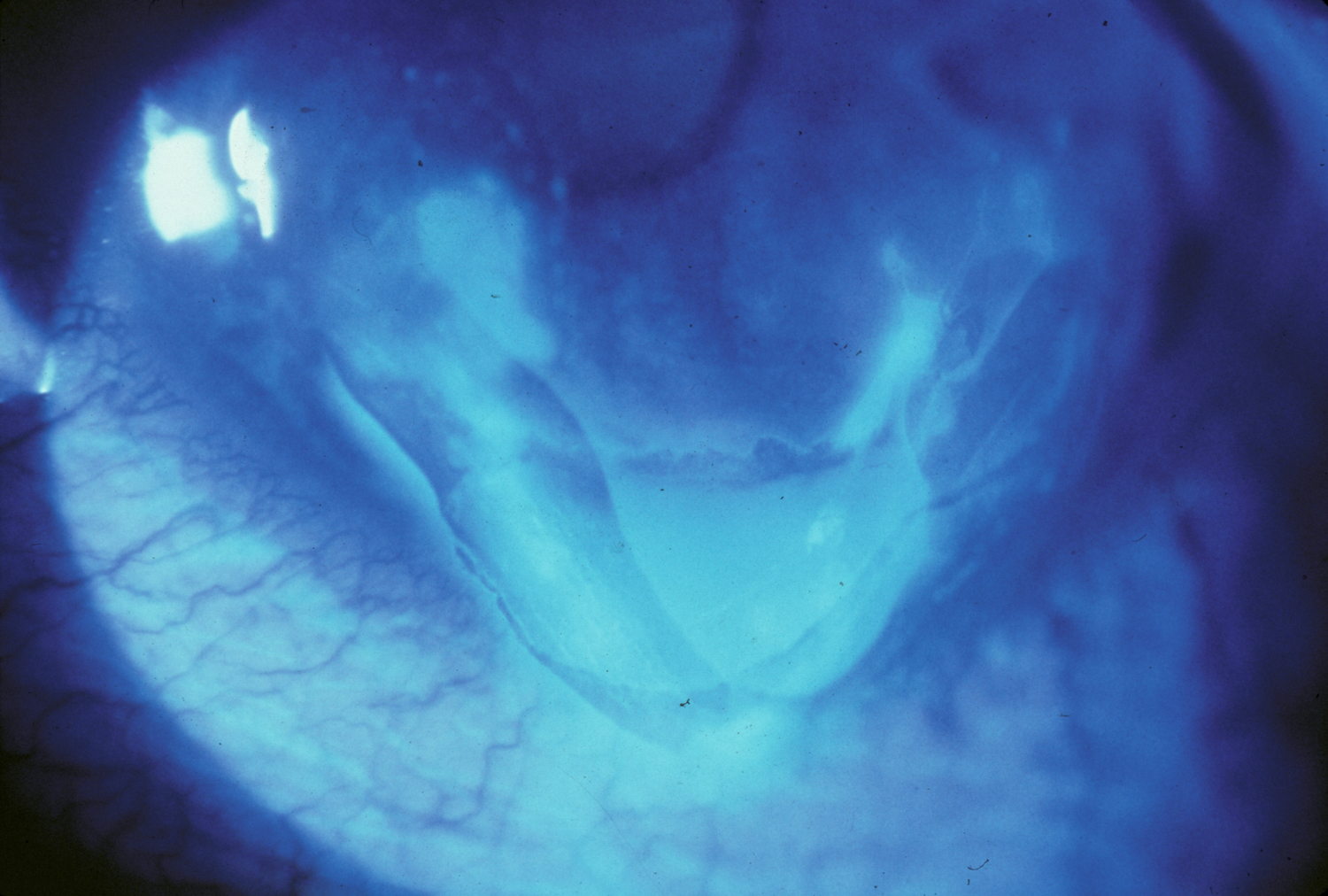
Aphakic bullous keratopathy is the presence of corneal epithelial bullae resulting from edema of the cornea, specifically in the absence of an intraocular lens transplant. This may result from Fuchs corneal endothelial dystrophy, a genetic disorder causing bilateral, progressive endothelial loss. ABK may also be caused by corneal endothelial trauma resulting from various intraocular procedures, such as cataract surgery. Under both circumstances, the corneal endothelium fails to sustain the normal dehydrated state of the cornea, leading to the formation of subepithelial fluid-filled bullae on the corneal surface as the corneal stroma swells. This often causes eye discomfort, impaired visual acuity, loss of contrast, glare, and photophobia. Treatment involves administration of topical dehydrating agents, intraocular pressure-lowering agents, and, in some cases, therapeutic soft contact lenses. Corneal transplant is often curative in the most severe cases (9).

References:
More commonly known as epithelial basement membrane dystrophy (EBMD) or map-dot-fingerprint dystrophy, anterior basement membrane dystrophy is the most common type of corneal dystrophy. The clinical course has two phases: an early phase characterized by recurrent epithelial erosions and a second phase with visual disturbances. This occurs as a result of abnormalities in the formation and maintenance of the epithelial basement membrane adhesion complex of the corneal epithelium. Though the majority of patients remain asymptomatic or experience only minor episodic discomfort, some will complain of recurrent corneal erosions and/or visual disturbances. Management focuses on improving vision and reducing the rate of recurrence of recurrent corneal erosions with application of nighttime lubricating or hyperosmotic ointments, use of bandage soft contact lenses, or, in more severe cases (see below links), treatment with surgical interventions, such as superficial keratectomy (SK).
References:
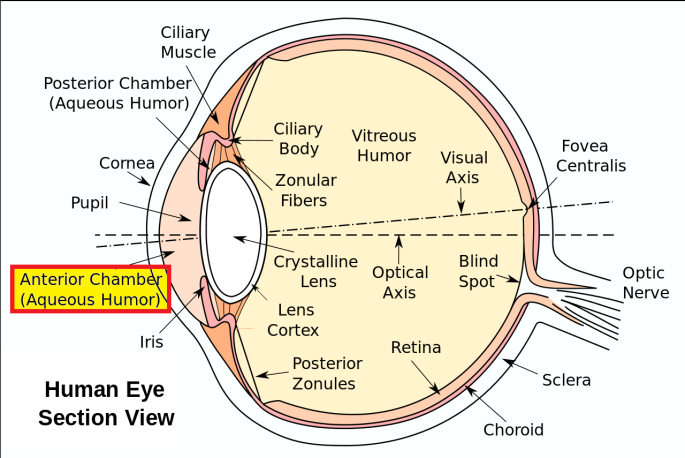
The anterior chamber is the fluid-filled space which lies between the iris and innermost surface of the cornea (the endothelium). This space is filled with aqueous humor, a clear watery fluid similar to plasma but with a low protein concentration. The tutorial link below provides an overview of when and how to place an anterior chamber intraocular lens (ACIOL).
References:
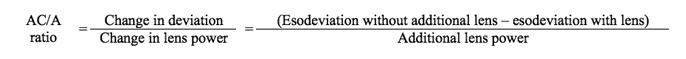
The AC/A ratio describes the relationship between the amount of accommodative convergence (AC) that is induced by a change in accommodation (A). Accommodative convergence refers to the simultaneous inward movement (adduction) of the eyes toward midline in the effort to maintain singular binocular vision when viewing an object (14). Accommodation refers to the change in lens shape which allows the eye to alter focus from distant to near objects (15).
References:
Acetylcholine is a naturally occurring neurohormone that binds at neuromuscular junctions in sympathetic and parasympathetic systems. It may be administered as an ophthalmic agent to produce miosis (constriction of the pupil), particularly during surgery. Direct application causes contraction of the sphincter muscles of the iris, resulting in miosis and contraction of ciliary muscles (accommodation).
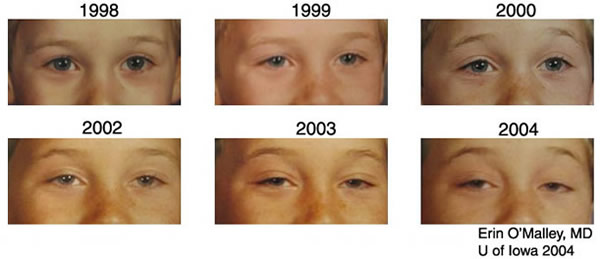
Ach is the primary neurotransmitter for parasympathetic post-ganglionic neurons. Myasthenia gravis (MG) is an autoimmune disease associated with anti-acetylcholine antibodies and decreased activation of post-synaptic Ach receptors. Patients may present with fatigable ptosis, ophthalmoplegia, and/or diplopia. The below cases discusses use of short acting acetylcholinesterase inhibitors for the diagnosis of MG.
References:
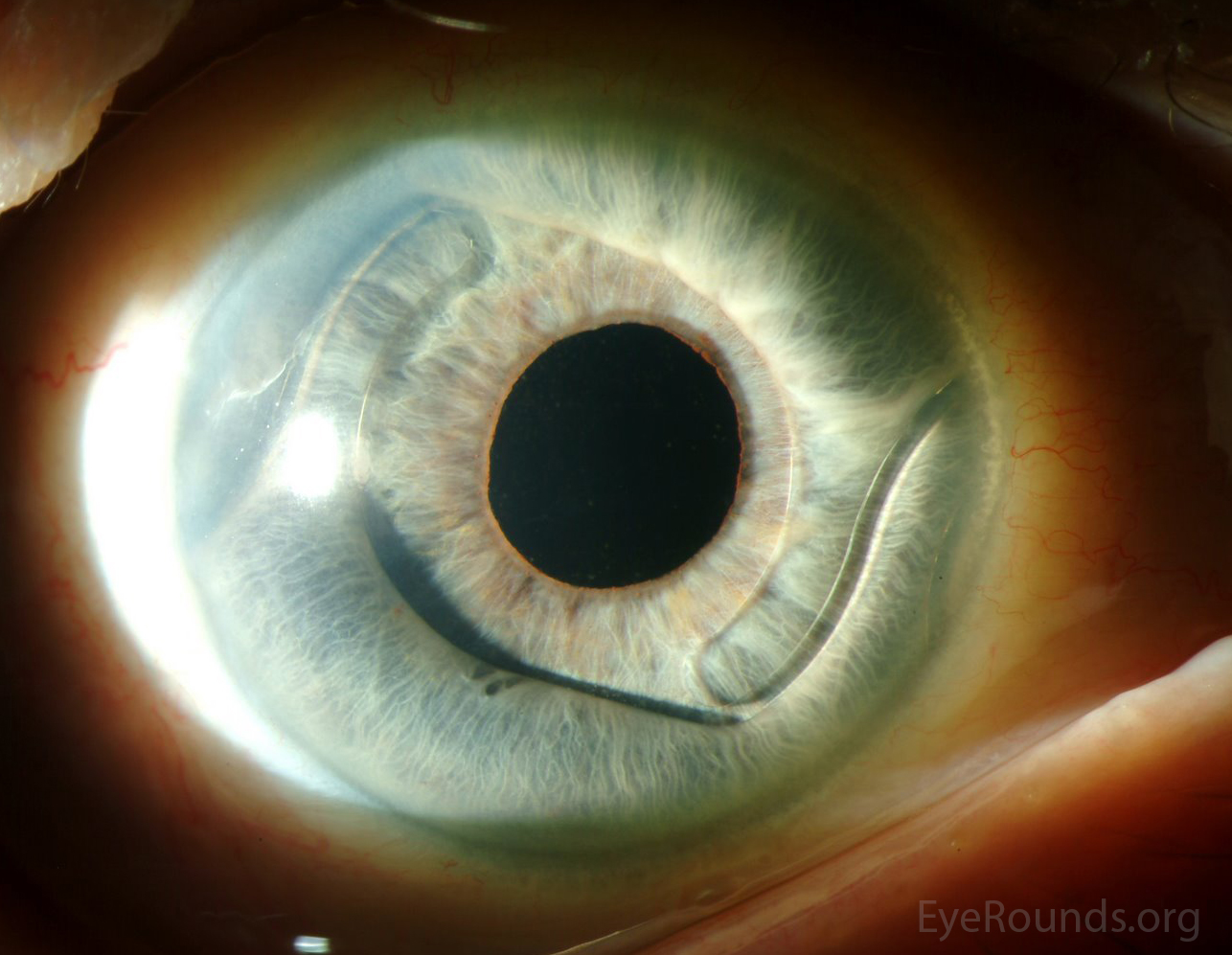
An anterior chamber intraocular lens is an artificial lens placed in the anterior chamber following removal of the natural lens during cataract surgery. Placement of an ACIOL is indicated when capsular support for the placement of a more standard posterior chamber intraocular lens is deficient, as may occur with capsular tear or zonular damage (17). Read more about the technique for ACIOL placement in the tutorial below.
References:
Autosomal dominant refers to one of several patterns of genetic inheritance in which a trait or disorder is passed down through families. In autosomal dominant inheritance, one mutated copy of a gene is sufficient for the person to be affected by the associated disorder or to express the trait coded for by the dominant gene.
Autosomal dominant inflammatory vitreoretinopathy is a hereditary autoimmune uveitis of the eye caused by mutation in the calpain-5 (CAPN5) gene. Clinical features include cataracts, progressive panuveitis, cystoid macular edema, abnormal retinal pigmentation, retinal and iris neovascularization, vitreous hemorrhage, intraocular fibrosis and membrane formation, and tractional retinal detachment (19). Advanced ADNIV leads to blindness and phthisis bulbi. Management includes a combination of immunosuppression with corticosteroids, anti-VEGF agents, and surgical intervention (cataract extraction, retinal detachment repair, glaucoma surgery, etc), when appropriate.

References:
Astigmatic keratotomy is a surgical technique used to correct astigmatism by making paired incisions at the steepest part of the cornea. This causes the cornea to relax and assume a more rounded shape. Recently, this approach has been largely replaced by LASIK surgery (20).

References:
Atopic keratoconjunctivitis (AKC) is a chronic inflammatory disease affecting the eye. The disease is chronic and bilateral, often relapsing with little or no seasonal correlation. Though the pathogenesis has not been fully determined, AK originates from a disorder of the adaptive immune system in predisposed individuals, such as those with atopic dermatitis or asthma. Patients often present with ocular itching, mucoid discharge, tearing, periocular eczema, and lid manifestations. Development of corneal neovascularization, corneal ulcers and erosion, and posterior subcapsular cataracts may also occur. Treatment focuses on decreasing the inflammatory response and controlling symptoms, often under the guidance of an allergist and dermatologist (22).

References:
Axial length is the distance between the surface of the cornea and Bruch’s membrane underlying the retina. Usually measured using ultrasonography or partial coherence interferometry, the AL at birth is approximately 17mm, reaching approximately 24mm in adults. Longer axial eye lengths are typically present in myopes and shorter eye lengths in hyperopes (23). AL plays a crucial role in optics and choosing an intraocular lens for cataract surgery. In primary congenital glaucoma, axial myopia is common, and axial eye length should be measured serially to ensure the eye is growing at a normal rate.
Associated pathologies:
Argon laser trabeculoplasty is a laser technique used for the treatment of ocular hypertension, primary open angle glaucoma, and secondary open angle glaucomas. Trabeculoplasty increases outflow from and increases function of the trabecular meshwork, which decreases intraocular pressure. Laser trabeculoplasty is particularly effective in glaucomas with increased pigment in the trabecular meshwork (e.g., pigmentary glaucoma) but should be avoided in inflammatory states.
Associated pathologies:
References:
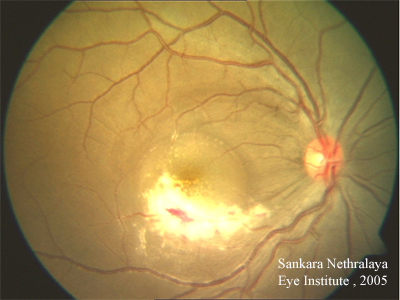
Age-related macular degeneration is a main cause of vision loss in patients over 60 years old. There are two forms of the disease: wet (neovascular or exudative) and dry (non-neovascular or non-exudative). The wet form is less common and occurs when networks of blood vessels called choroidal neovascular membranes (CNVM) gain access to and proliferate in or under the retina, leading to the extravasation of blood and fluid. Dry AMD results from the gradual break-down of light-sensitive cells (photoreceptors) in the macula, leading to outer retinal atrophy. The clinical hallmark of AMD is the presence of drusen, yellow deposits beneath the retina. The wet form of macular degeneration is treated with anti-vascular endothelial growth factor (VEGF) intravitreal injections to decrease the growth and leakage of a CNVM. Specific eye vitamins used in the Age-Related Eye Disease Study (AREDS vitamins) are recommended in most cases of AMD (intermediate and advanced unilateral disease) to slow progression of disease (24). At this time, there is no treatment to reverse the process of AMD. Patients should be advised to stop smoking as this is strongly related to an increased risk of developing AMD

References:
Anti-nuclear antibodies are autoantibodies that target the contents of the host cell nucleus. Generally, ANA testing is performed to diagnosis certain autoimmune diseases, such as juvenile idiopathic arthritis (JIA), systemic lupus erythematous (SLE), Sjögren's syndrome (SS), among others (26).
References:
Anti-neutrophil cytoplasmic antibodies may occur in patients with autoimmune vasculitis, such as granulomatosis with polyangiitis, Churg-Strauss syndrome, and microscopic polyangiitis. These and other ANCA-associated vasculitides may present with a number of ophthalmic manifestations, some of which may be the earliest indicators of systemic disease (27).
Associated pathologies:
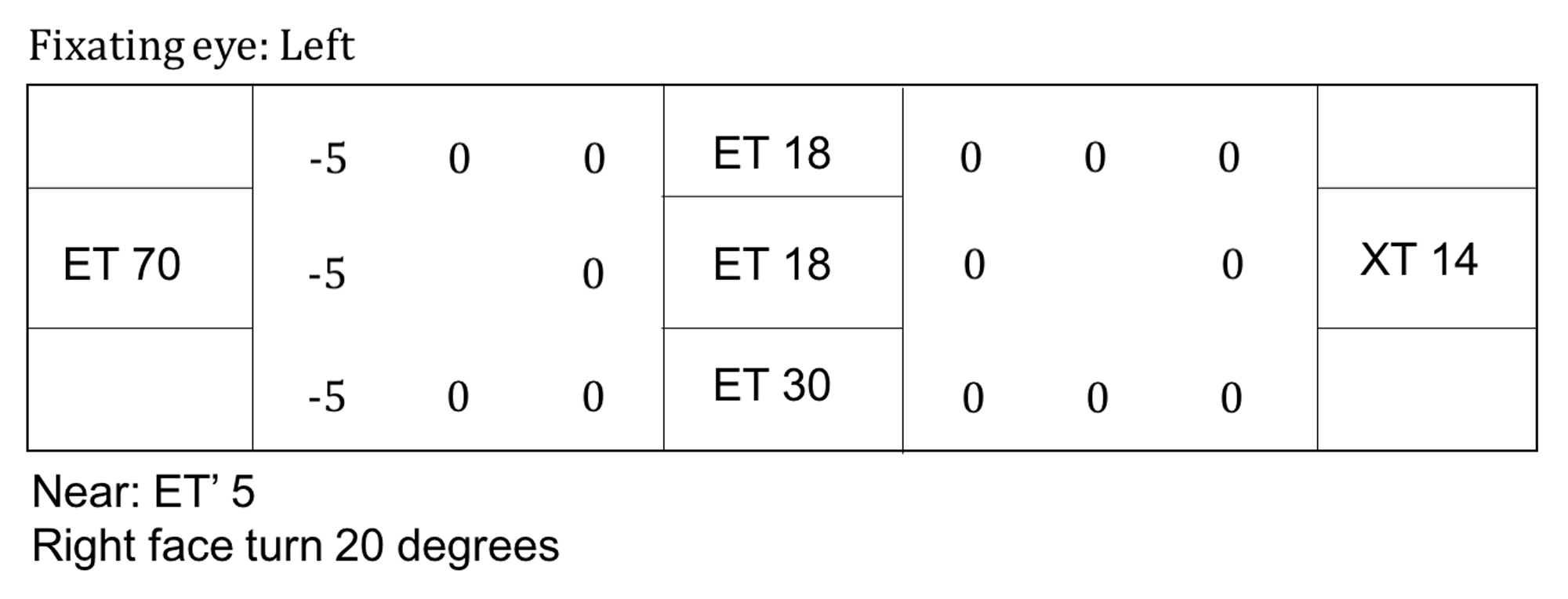
An alternate prism cover test is used to determine the full amount of ocular misalignment (strabismus) in a patient. To perform this test, one eye is occluded, and then the other, with a prism held over the non-fixating eye. The prism must be held in the appropriate direction for the deviation (e.g., base out prism for an esodeviation). While the patient is fixating on an object in the distance, various strengths of prisms are held over the eye until the deviation is corrected. The strength of the prism (in Prism Diopters) necessary to neutralize the deviation is used to quantify the degree of misalignment.
References:
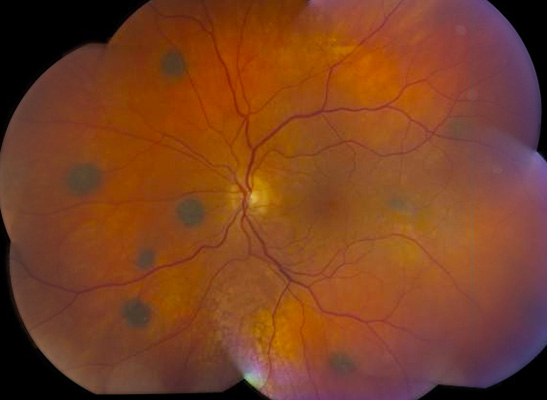
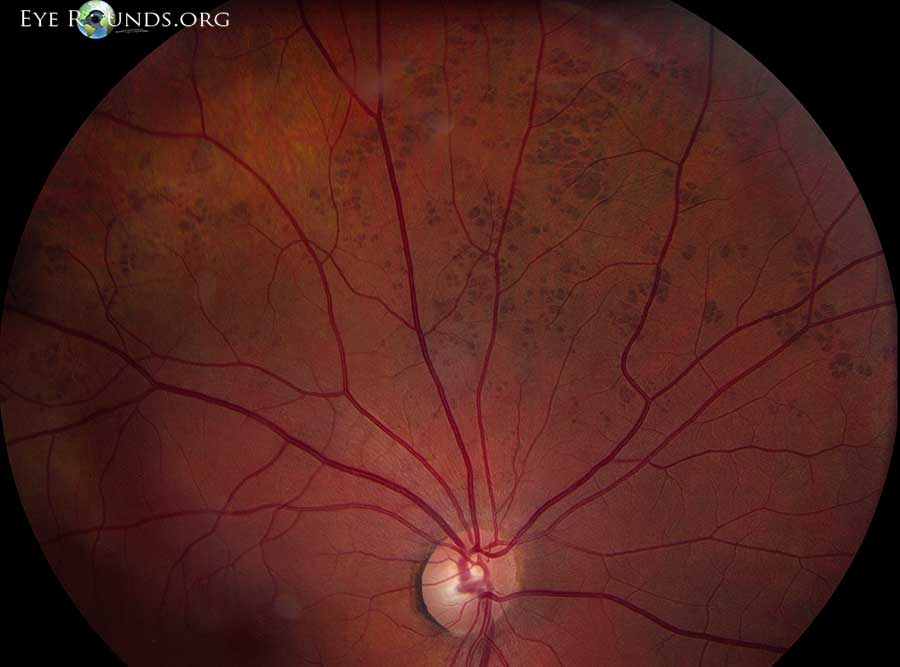
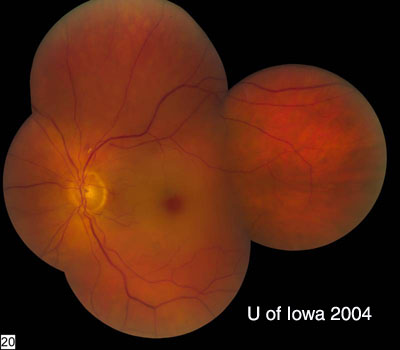
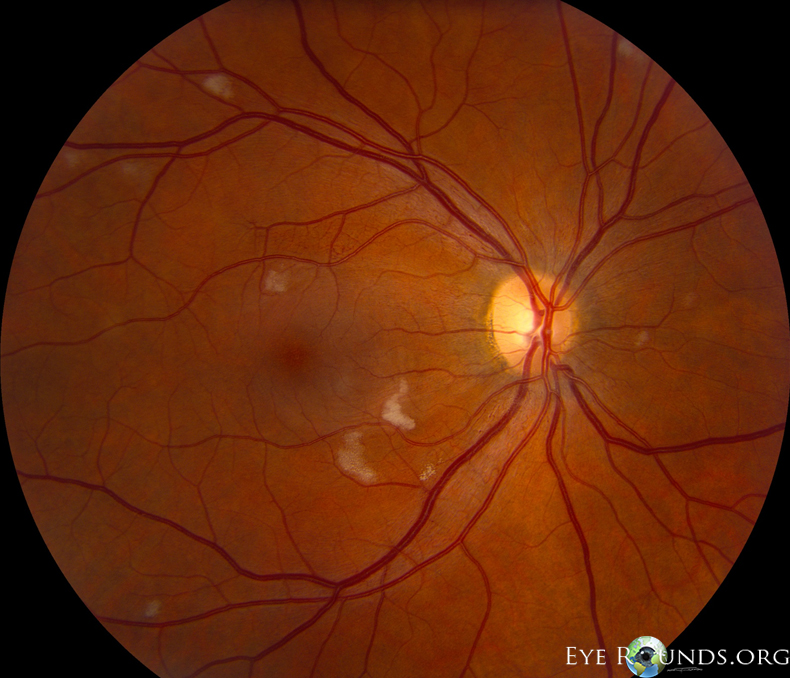
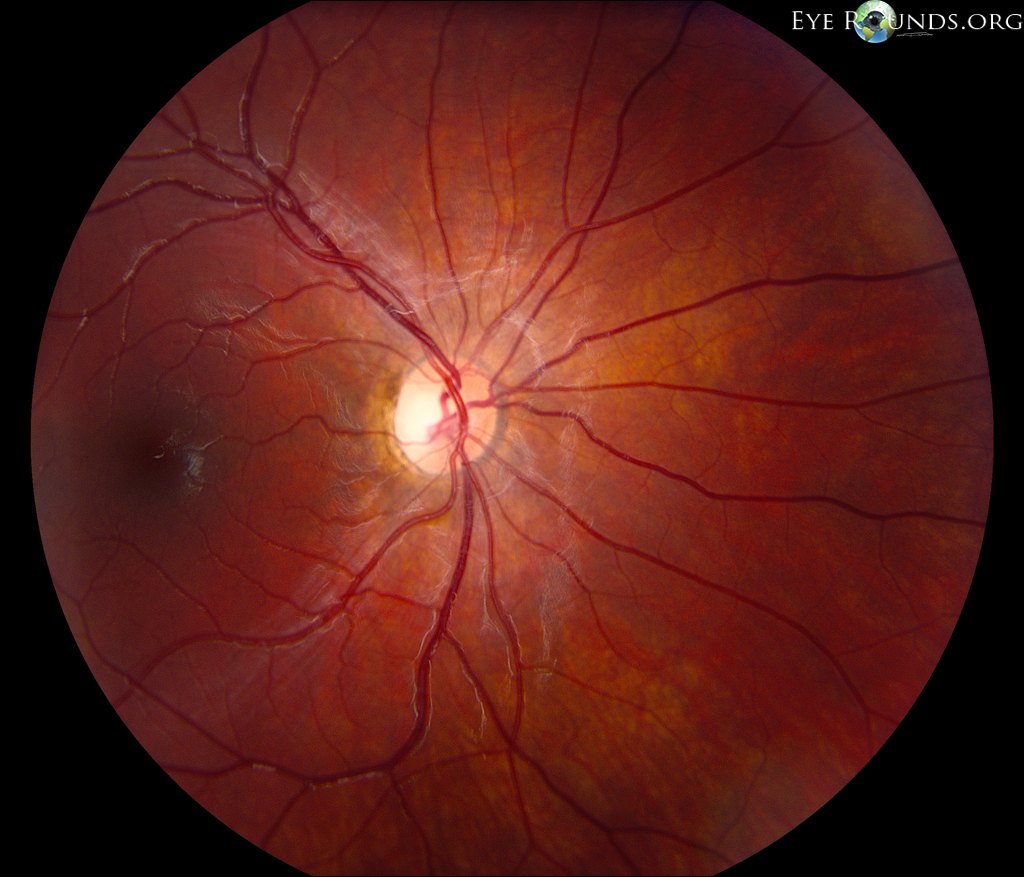
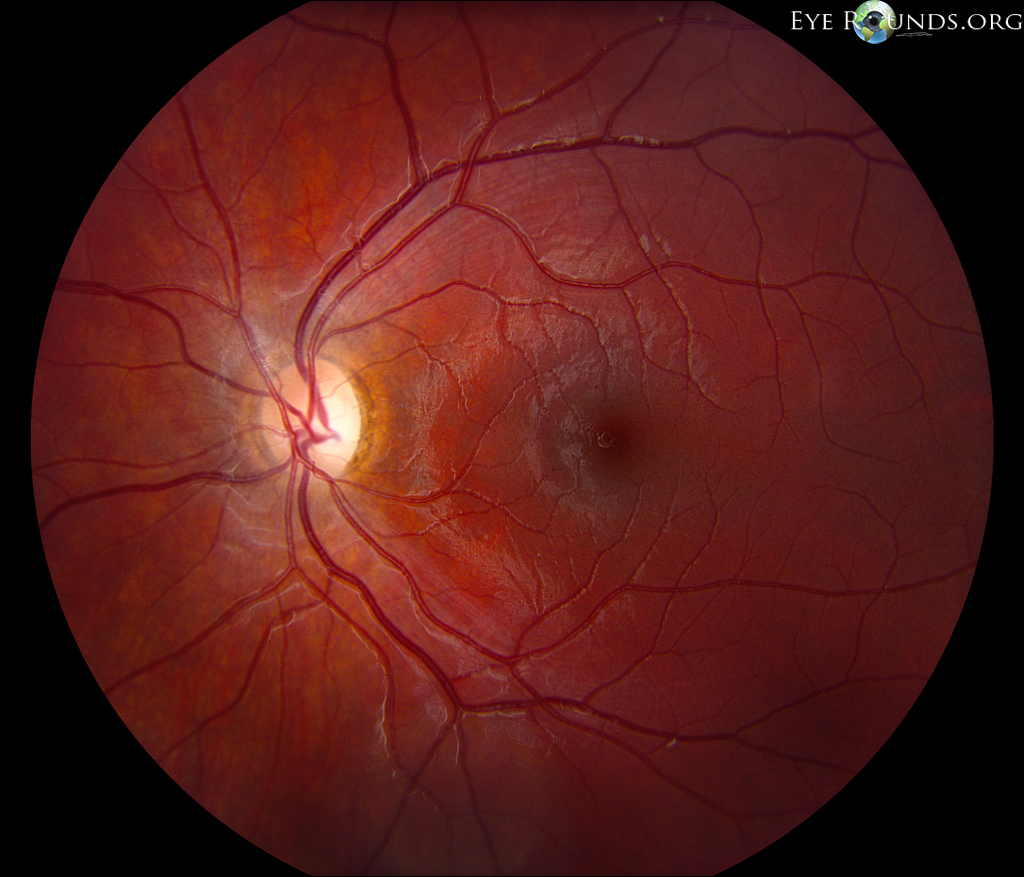
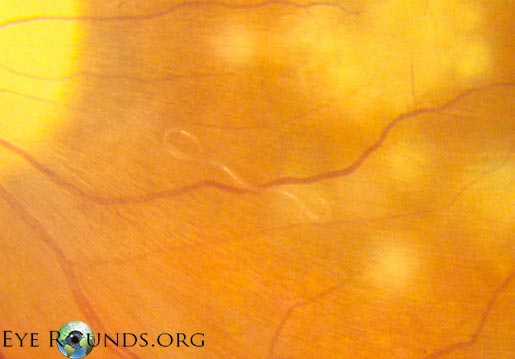
Acute posterior multifocal placoid pigment epitheliopathy is a granulomatous inflammation predominantly affecting the choroid and retinal pigment epithelium (RPE). APMPPE is classified as one of the white dot syndromes (WDS), and one third of patients experience a flu-like illness at or prior to onset. Occurring in young, healthy adults, it is usually bilateral with patients typically experiencing rapid onset of blurred vision, paracentral scotomas, and photopsias (perceived flashes of light). The condition is generally self-limited, requiring no treatment with vision often recovering in 4 weeks. In rare cases, APMPPE is associated with life-threatening cerebral vasculitis and other central nervous system manifestations that should not be missed (28).
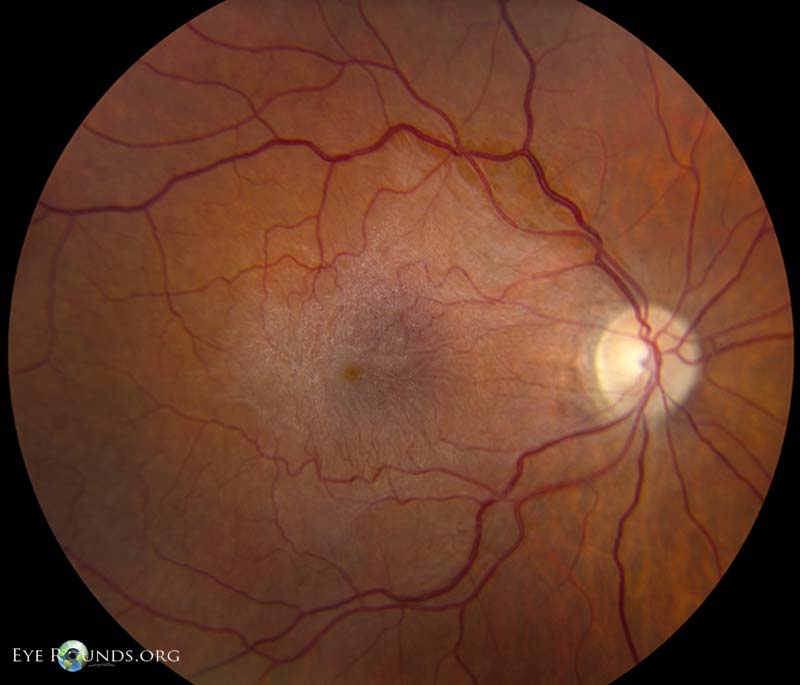
On fundoscopic exam, APMPPE presents as multiple bilateral yellow-white placoid lesions throughout the fundus. An anterior segment exam is usually normal, though anterior uveitis may be present. Diagnosis may be made with fundoscopy alone, though fluorescein angiogram, indocyanine green angiogram, fundus autofluorescence, and optical coherence tomography may be used to verify.

References:
Autosomal recessive refers to one of several patterns of genetic inheritance in which a trait or disorder is passed down through families. In AR inheritance, two mutated copies of a gene (one from each parent) are necessary for the person to be affected by the associated disorder or express the trait coded for by the recessive gene.
Autosomal recessive ocular disorders:
Anomalous or abnormal retinal correspondence occurs in cases of ocular misalignment (strabismus) in which non-corresponding retinal points in the right and left eye are linked in the visual cortex. This is a sensory adaptation allowing for binocular vision despite long-standing deviation of an eye. For instance, the fovea of the non-deviated eye would link to an extrafoveal retinal point in the deviated eye to provide binocular vision (30).
References:
The Age-Related Eye Disease Study is a large clinical trial put forth by the National Eye Institute (NEI) to investigate the natural history and risk factors of age-related macular degeneration (AMD) and cataracts. Specifically, the effects of high doses of vitamin C, vitamin, beta-carotene, and zinc on AMD and cataracts were studied, showing that elevated levels of antioxidants and zinc significantly reduce the risk of AMD. No effect was found in cataracts (31). A follow-up study, AREDS-2, investigated the effects of omega-3 fatty acids alongside the antioxidants, lutein and zeaxanthin, in AMD patients. Omega-3 fatty acids were found to have no effect, while lutein and zeaxanthin together were found to be an effective substitute for beta-carotene, which is known to increase the risk of lung cancer in smokers (32). Thus, the AREDS2 formulation is strongly preferred, especially for all current or prior smokers.
Further, AMD has been categorized by The Age-Related Eye Disease Study based on exam findings of hard drusen, soft drusen, RPE abnormalities, atrophy, and choroidal neovascularization (32). See below atlas link for descriptions of these categories.
Relevant link:
References:
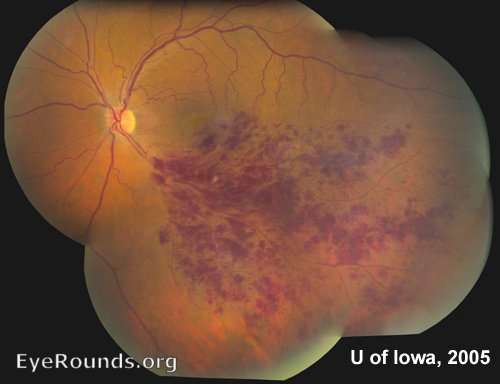
Acute retinal necrosis in an inflammatory condition caused primarily by the varicella zoster (VZV) and herpes simplex viruses (HSV). Most often affecting healthy, immunocompetent adults, patients present with acute onset vision loss in one eye, commonly with redness, photophobia, pain, floaters, and flashes. These symptoms occur when viral particles in the retina and vitreous provoke an inflammatory response that occludes the retinal arterioles and choroidal vasculature, causing necrotizing retinitis of the downstream tissue. Fundus examination will show discrete areas of peripheral retinal whitening and severe vitritis. There is rapid progression without treatment (33).
Approximately 50-70% of patients will develop retinal detachments in the affected eye within 3 months of onset. Treatment is individualized with administration of prompt intravitreal (e.g., foscarnet) and/or systemic antivirals (e.g., valacyclovir). In cases involving ischemic optic neuropathy, anti-inflammatory and antithrombotic therapy may also benefit. Laser photocoagulation may be used to prevent future retinal detachment, while surgery is used to treat existing detachments (33).
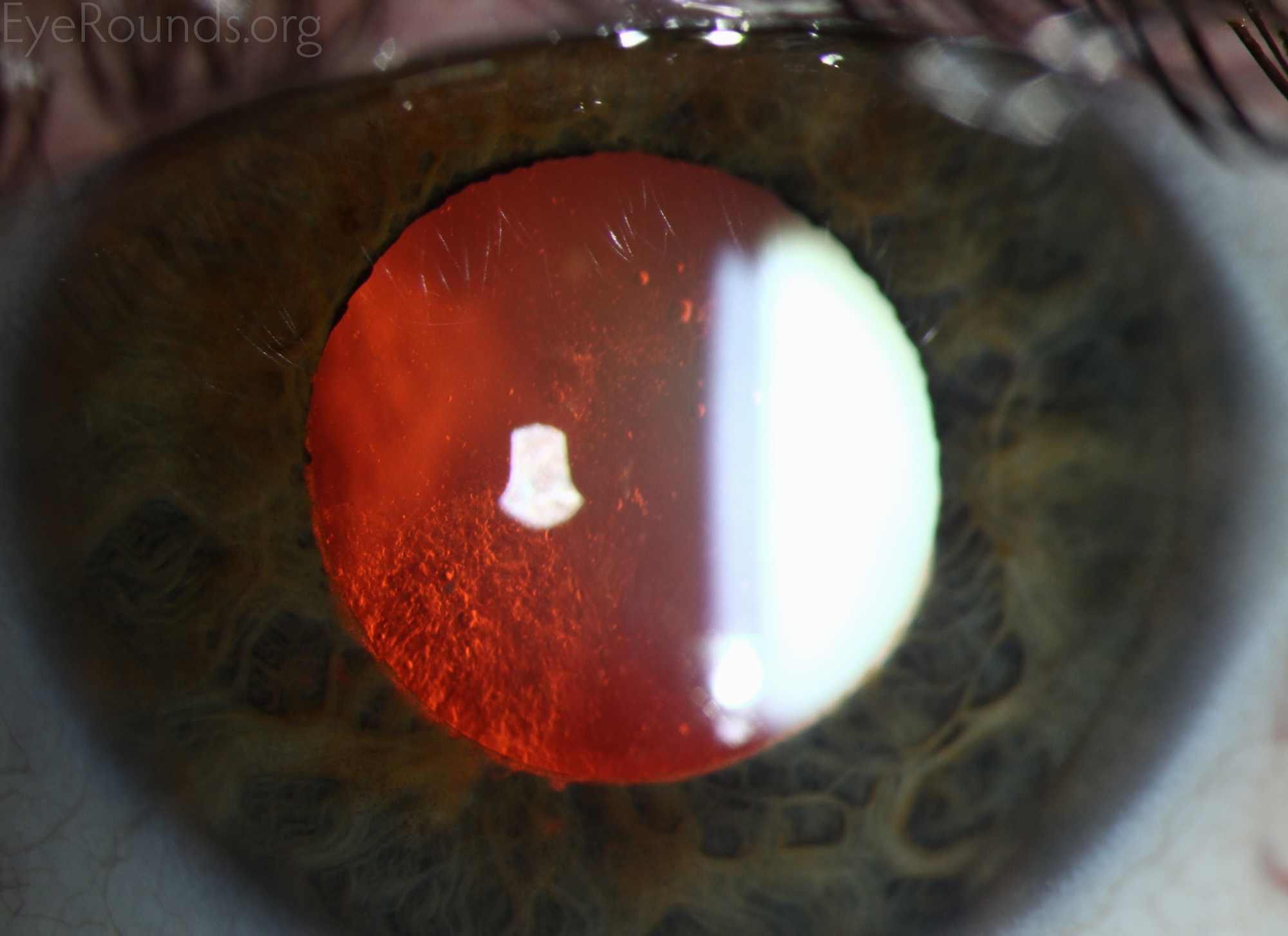
Anterior subcapsular cataracts form when anterior lens epithelial cells become necrotic, as may occur with iritis, keratitis, inflammation from atopic dermatitis, irradiation, or electrical burns. This ultimately causes an opacification of the lens as adjacent epithelial cells migrate to form a plaque of myofibroblasts over the damaged area. Eventually the myofibroblasts resolve, leaving behind a wrinkled appearing lens capsule (34).
References:
Aqueous tear deficiency is a form of dry eye due to impaired tear production resulting from lacrimal gland destruction or dysfunction. This ultimately causes hyperosmolarity of the tear film and ocular surface, which leads to inflammation with dryness, redness, irritation, light sensitivity and blurred vision. ATD can be further classified to Sjögren’s and non-Sjögren’s syndrome:
Treatment for ATD focuses not only on the underlying cause but also on increasing or supplementing tear production. Artificial tears may be useful (35).
References:
Artificial tears are lubricants that serve as first line treatment for ocular irritation, particularly in cases of dry eye. There are numerous ATs available, with some available as over the counter preparations (36).
General categories include demulcents, emollients, and homeopathic drops. Further detail may be found in the tutorial below.
References:
Arteriovenous refers to anything relating to or affecting an artery and a vein. Examination of the arteries and veins is an important part of the dilated examination. AV nicking may be seen in patients with hypertension, where the arteries or arterioles compress the underlying vein or venules; such impingement can lead to a branch retinal vein occlusion.
Arteriovenous malformations (AVM) and arteriovenous (AV) fistulas can affect the orbit and eye; additional information regarding these topics can be found at the links below.
References:
Anterior vitreous cell is a slit lamp finding that usually suggests the presence of ocular inflammation, especially if there are numerous small white cells (inflammatory cells). Patients who have retinal tears or retinal detachment will often present with anterior vitreous cells that appear pigmented; this is considered a positive Shafer sign.
The below links highlight significant anterior vitritis with numerous AVC in the setting of sympathetic ophthalmia and autoimmune retinopathy.
References:
Arteriovenous malformations are congenital, sometimes familial, abnormalities of the vascular architecture. In these cases, there is a direct connection between veins, which are low flow vessels, and high flow arteries. AVMs may affect retina vessels or may also occur in the orbit, facial bones, and brain. The latter may cause secondary neurologic symptoms; thus, head imaging is warranted in patients with retinal AVMs.

References:
An anterior vitrectomy is most often performed as part of a cataract surgery. Though this procedure may be anticipated as part of a traumatic cataract surgery, it is often an unplanned addition to cataract surgery used to correct vitreous prolapse following rupture of the posterior lens capsule. In this procedure, vitreous humor is removed from the anterior chamber using the vitrectomy cutter (39). The basic principles of anterior vitrectomy can be found in the anterior vitrectomy tutorial below.
References:
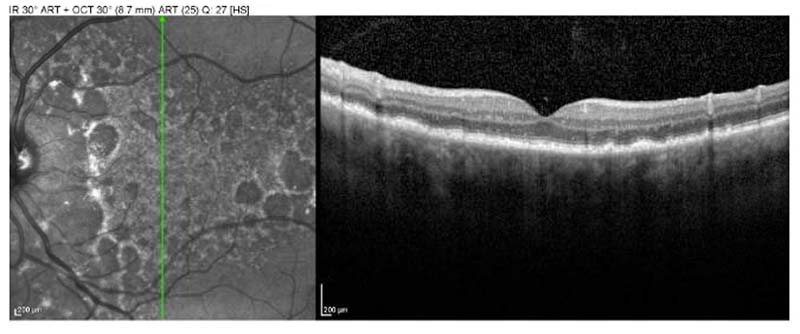
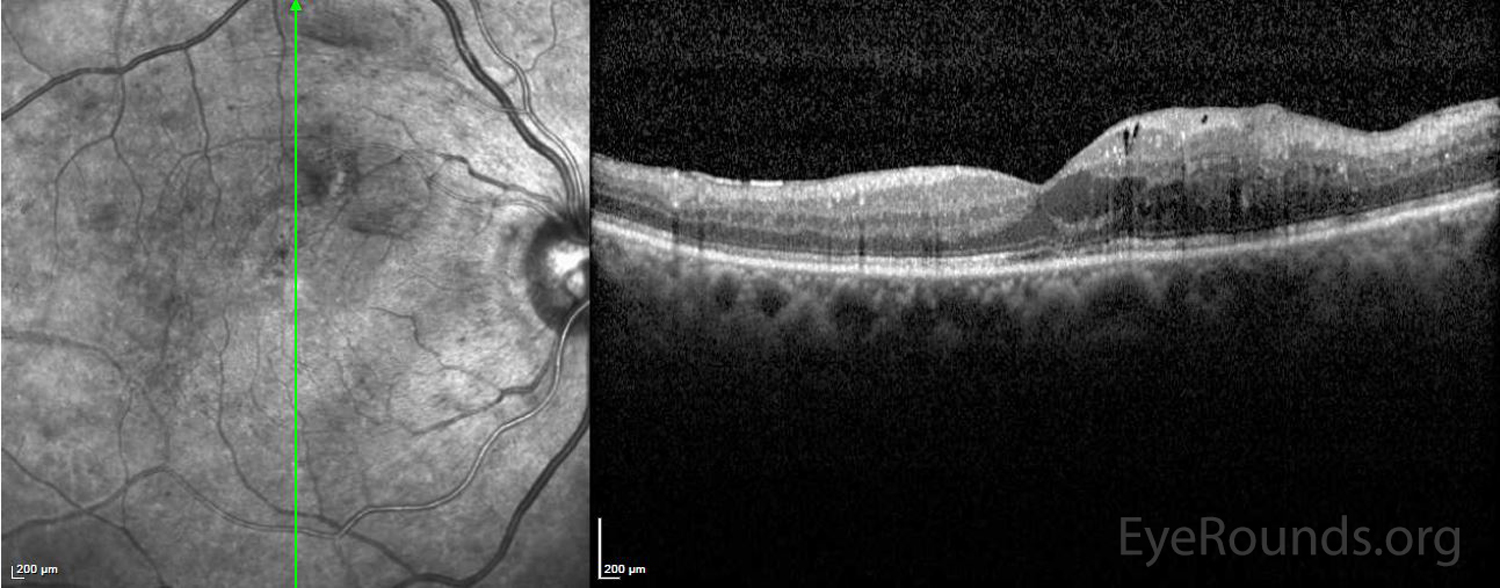
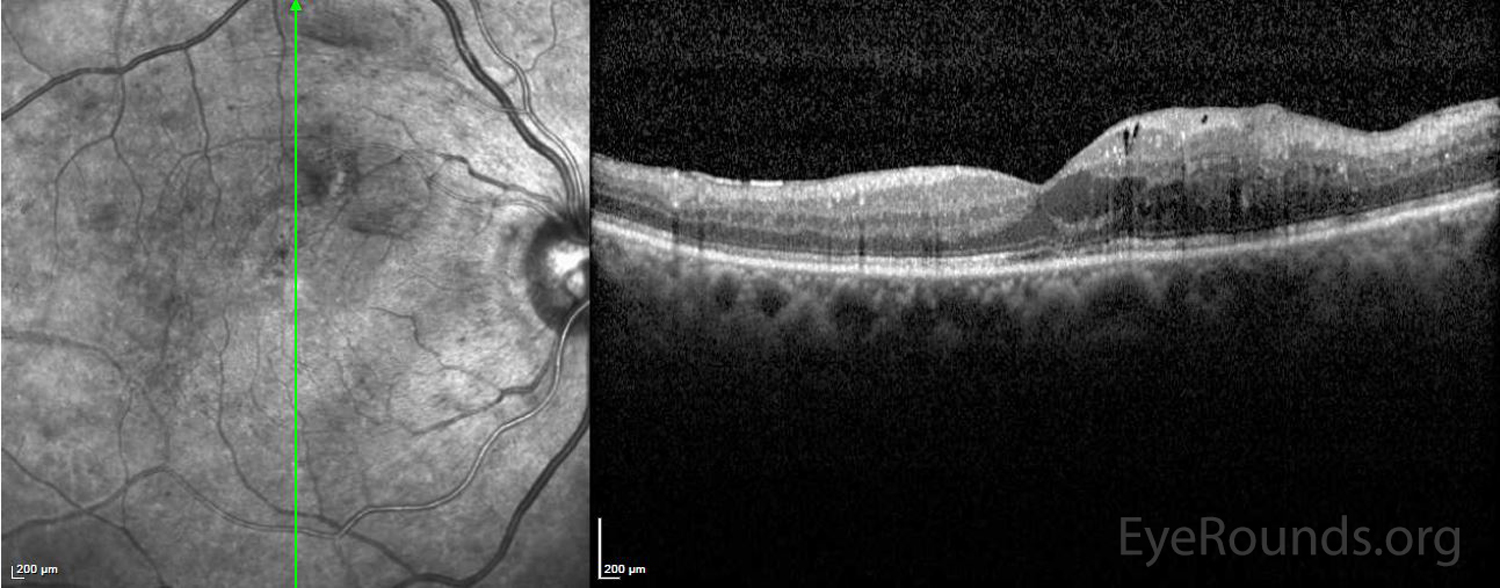
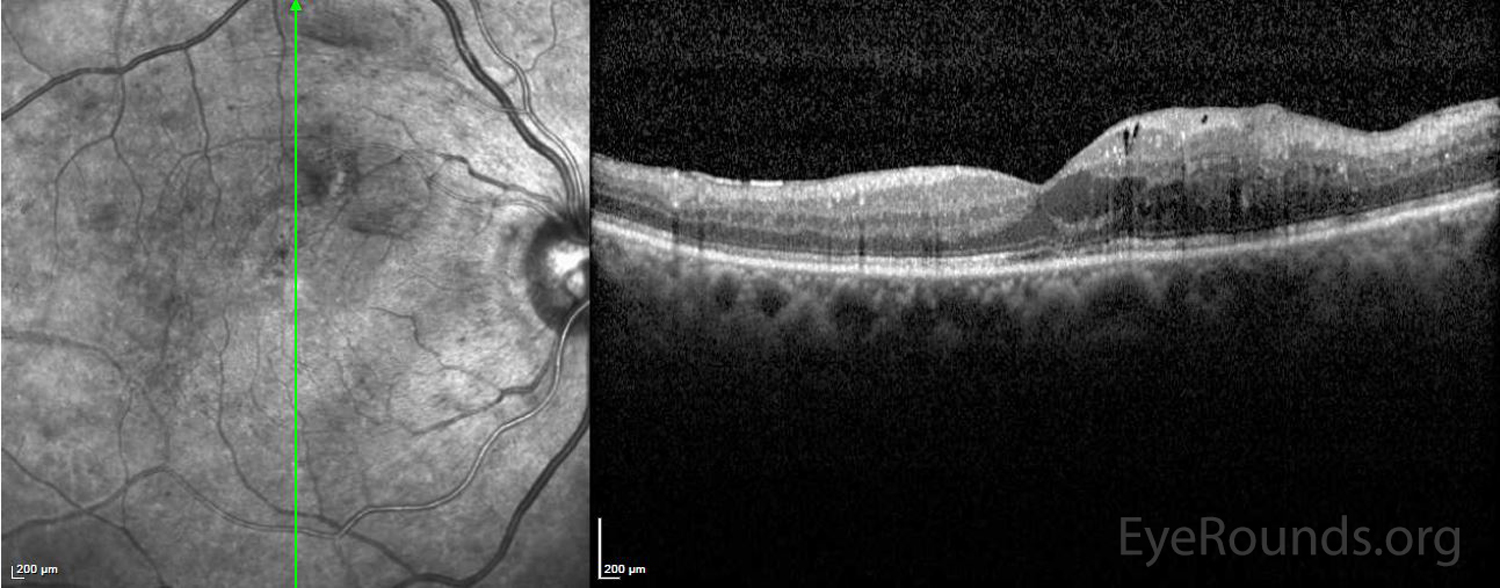
Acute zonal occult outer retinopathy is an inflammatory outer retinal disease characterized by rapid loss outer retinal function with minimal change to the fundus appearance initially. Patients typically are young myopic women and present with photopsias, visual field defects, and a relative afferent pupillary defect (RAPD). Optical coherence tomography (OCT) may show thinning of the outer retina, and fundus autofluorescence shows a characteristic pattern of hypoautofluorescence in the involved area with speckled hyperautofluorescence at the border. There are also mild electroretinographic abnormalities. Most patients recover vision within six months with most achieving good vision. Late fundus findings may include peripapillary retinal pigment epithelium (RPE) changes/depigmentation and/or areas that resemble sectoral retinitis pigmentosa (RP) (40). The mechanism of the disease is unknown, though it has been associated with autoimmune mediated disorders. No proven treatment exists (41).
References:
Basal cell carcinoma, a slow growing tumor of the deepest skin layer, is the most common malignancy of the eyelids often appearing as an elevated pearly lesion with rolled borders, ulceration, and madarosis (loss of eyelashes). The lower eyelid is most often affected, with risk factors including sun exposure and a history of other skin cancers. There are four main types, including nodular BCC (most common), morpheaform BCC (most aggressive), pigmented BCC, and multicentric BCC. Though growth is slow and malignancy is rare, treatment involves complete surgical resection and oculoplastic reconstruction in the most severe cases (42).


References:
The bandage contact lens is a soft contact lens used to protect damaged or irregular corneal surfaces. These non-refractive lenses are commonly used after refractive surgeries, such as LASIK, to reduce inflammatory cell infiltrate in the corneal stroma and associated scarring. They may also be used in treatment of cranial nerve V and cranial nerve VII palsies to protect from corneal exposure and ulceration (44). BCLs are used cautiously in the setting of recurrent erosions and/or corneal abrasions. It should be noted that patients wearing BCLs must also use frequent topical antibiotic drops to prevent corneal infection from developing. Close follow-up is warranted to prevent infectious complications.
References:
Best corrected visual acuity is a measurement of vision obtained when using the best possible lens correction for the patient. As measured by a Snellen chart, a person is considered legally blind in the United States if they have a BCVA of 20/200 or worse in their better eye (45).
References:
A base down prism has its thickest edge on the bottom. This serves to move an image upward when placed in front of the eye, making it instrumental in the measurement and treatment of upward deviations of the eye, such as in hypertropia and hyperphoria (45).
References:
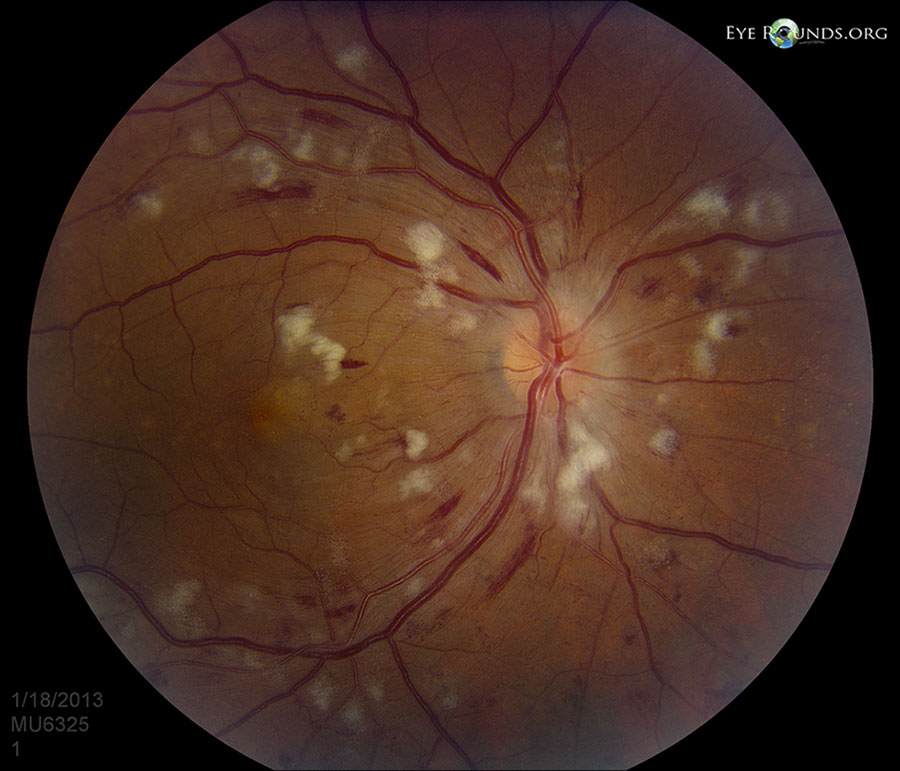
Background diabetic retinopathy, also known as non-proliferative diabetic retinopathy (NPDR), is a pathological condition associated with the initial stages of diabetic retinopathy. Hyperglycemia may result in damage to retinal capillaries, causing retinal changes, including microaneurysms, “dot-blot” hemorrhages (DBH), cotton wool spots (CWS, infarctions of the nerve fiber layer), and venous beading and dilation. BDR may progress to proliferative diabetic retinopathy (PDR), characterized by the formation of new and abnormal blood vessels (neovascularization) (46).
Review the following tutorial to learn about the classification of BDR, including the 4-2-1 rule for severe NPDR, screening recommendations, treatment options, and further resources.

References:
Bilateral diffuse uveal melanocytic proliferation is a rare paraneoplastic syndrome that results in bilateral vision loss followed by bilateral exudative retinal detachment and rapid cataract formation. Characterized by benign proliferation of choroidal melanocytes, BDUMP typically affects patients between 50-80 years with a co-occurring non-ocular malignancy, such as visceral cancer of the lung, colon, pancreas, gallbladder, ovary, uterus, or cervix. In approximately half of cases, non-ocular malignancies are found after diagnosis with BDUMP, while in the other half, malignancy has been previously diagnosed. An important aspect of management is evaluation for and treatment of the underlying non-ocular malignancy. Plasma exchange may also help to improve visual acuity and other symptoms (47).
References:
Blood glucose is an important metric in ophthalmology and medicine, in general, representing the amount of sugar in the blood at a given time. A high BG puts patients at risk of diabetes mellitus (DM), diabetic retinopathy (DR) with or without diabetic macular edema (DME), refractive changes (myopia or hyperopia), and cataracts (46).
References:
A base in prism has its thickest edge placed inward (nasally). This serves to move an image outward (temporally) when placed in front of the eye, making it instrumental in the measurement and treatment of outward deviations of the eye, such as in exotropia and exophoria (45).

References:
two times per day
An abbreviation for “bis in die," which in Latin means two times per day or twice daily; it is commonly used in prescriptions and clinical notes.
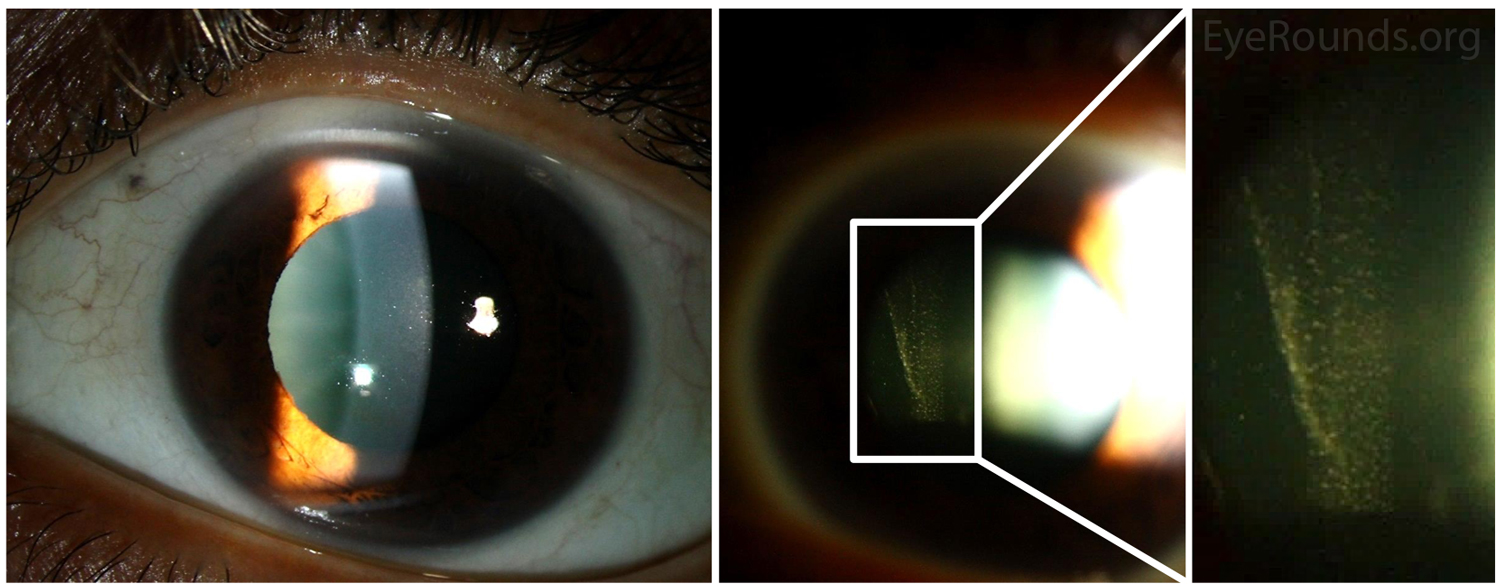
Band keratopathy is a form of corneal degeneration characterized by a band of horizontal calcium hydroxyapatite deposits in the superficial layers of the cornea, particularly Bowman’s layer. Band keratopathy first manifests as a fine, yellow-white deposit at the periphery of the cornea which may progress over a period of months to years to form the characteristic horizonal band across the cornea. Eventually, this band may impact vision as it covers the visual axis. Generally, this condition is associated with chronic ocular inflammation, hypercalcemia, hyperphosphatemia, certain hereditary disorders, or prolonged exposure to chemicals. Long-term intraocular silicone oil use for retinal surgery can lead to BK, especially when the anterior chamber (AC) is full of oil (49).
Treatment includes administration of lubricating drops, use of soft bandage contact lenses, and surgical intervention in the most advanced cases. Surgical options include manual superficial keratectomy to dissect and remove calcific deposits or excimer laser phototherapeutic keratectomy to precisely remove a desired thickness of anterior stroma (49).

References:
Blepharoplasty is a general term which refers to plastic surgery of the eyelids to remove excess skin and/or orbital fat for treatment of dermatochalasis. Blepharoplasties improve patient functionality by restoring a full visual field in patients whose lids obstruct the visual axis (45).
Videos: :
Bare light perception is a term used to describe severe visual impairment in which the patient is only capable of perceiving diffuse, indirect light. This is distinguished from light perception (LP) with projection, a term that indicates the patient sees where the light is coming from.
Bone marrow transplantation is a procedure which replaces diseased bone marrow cells with healthy donor marrow. This procedure is utilized in the treatment of leukemia, certain immune deficiencies, and other blood diseases.
References:
A base out prism has its thickest edge placed outward (temporally). This serves to move an image inward (nasally) when placed in front of the eye, making it instrumental in the measurement and treatment of inward deviations of the eye, such as in esotropia and esophoria (45).

References:
Blood pressure is measured in millimeters of mercury and is documented in two parts, diastolic BP and systolic BP. Diastolic BP is the lowest pressure in the cardiac cycle, corresponding to relaxation of the cardiac muscle. Systolic BP is the highest pressure in the cardiac cycle, corresponding to contraction of the cardiac muscle. According to the American Heart Association, high blood pressure is defined as a systolic BP higher than 130 or a diastolic BP higher than 80 (52).
High blood pressure (hypertension, HTN) may lead to cotton wool spots, hemorrhages, exudates; accelerated HTN may have several impacts on vision by causing swelling of the macula or optic nerve with acute vision loss. Additionally, HTN is a risk factor for eye diseases such as glaucoma, diabetic retinopathy, and macular degeneration.
References:
A branch retinal artery occlusion occurs when the flow of blood through any of the branches of the central retinal artery is blocked by an embolus (blood clot). This disruption of blood flow may cause ischemia and damage to the retina along with defects in the visual field corresponding to the blocked artery (45). Clinical signs include the presence of cotton wool spots (infarctions of the nerve fiber layer) and retinal whitening on funduscopic exam. Among the common sources of emboli are cholesterol (Hollenhorst plaque), platelet fibrin, or calcific emboli, among others. While BRAO often resolves on its own, assessment of stroke risk and referral to a stroke center are common aspects of management. In more severe/prolonged cases, antiplatelet therapy, anti-vascular endothelial growth factor (VEGF) agents, carotid endarterectomy or laser photocoagulation may be pursued (54).

References:
A branch retinal vein occlusion occurs when blood flow through a branch of the central retinal vein is blocked. This often results from compression from an overlying retinal artery that has been hardened, though may also result from vessel degeneration or coagulation (45). Blockage of the vein may cause hemorrhage, with flame hemorrhages, dot and blot hemorrhages (DBH), and cotton wool spots (CWS, infarctions of the nerve fiber layer) being typical findings on fundus exam. Macular edema may also cause deficits to the central vision. Patients typically present with acute, painless vision loss, while resulting neovascularization (NV) with subsequent vitreous hemorrhage (VH) may cause the patient to see floaters. Management may involve laser photocoagulation, steroid treatment, and/or administration of anti-vascular endothelial growth factor (VEGF) agents. Please see the BRVO case for further discussion of pathophysiology, diagnosis, management, and prevention.
References:
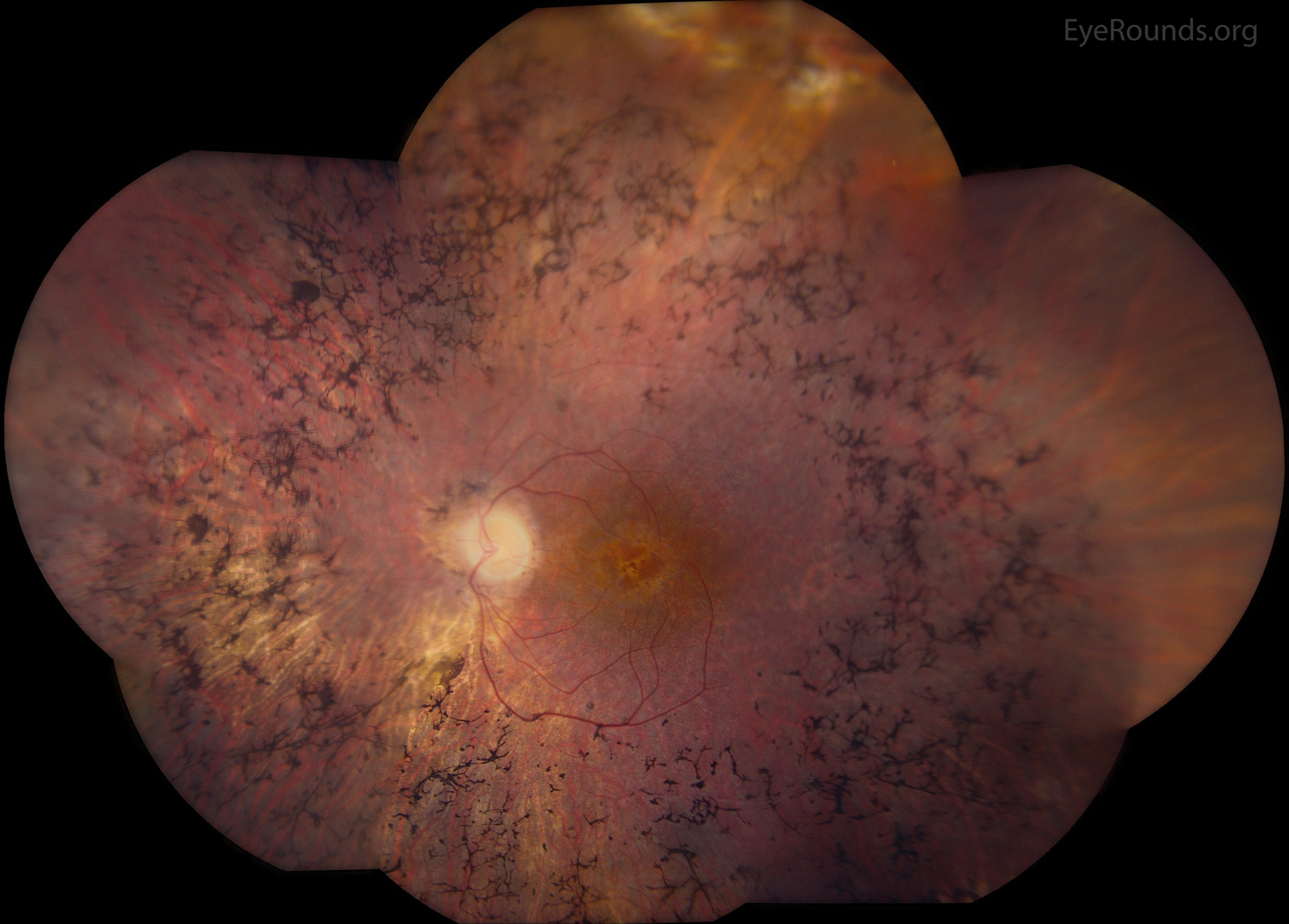
Bone-spicule-like pigmentation is a characteristic funduscopic finding in retinitis pigmentosa (RP), a family of inherited diseases causing progressive retinal degeneration and vision loss. Most prevalent in the mid-peripheral retina, these pigment clumps correspond to melanin-containing cells, which cluster around blood vessels in the inner retina. BSLP has been shown to be derived from cells in the retinal pigment epithelium (RPE) (57).
Please visit StoneRounds.org to learn more about inherited retinal diseases.
References:
A base up prism has its thickest edge placed upward. This serves to move an image down when placed in front of the eye, making it instrumental in the measurement and treatment of downward deviations of the eye, such as in hypotropia and hypophoria (45).
References:
Blood urea nitrogen is a test which measures the amount of urea in the blood, measured using the blood’s nitrogen content. This is an important indicator of kidney and liver function, as the liver produces ammonia (containing nitrogen), and the waste product, urea, is transported to and filtered from the blood in the kidneys. Generally, a BUN of 7-20 mg/dL is considered normal (45, 59).
See the below links to learn more about ocular diseases that often have abnormal BUN or creatinine levels due to kidney dysfunction.
Associated pathologies:
Cup-to-disc ratio refers to the area of the optic cup compared to the area of the entire optic disc/nerve. The optic cup is clinically seen as the white area in the center of the optic disc where the retinal ganglion cells exit the eye and through which the major blood vessels pass (45). C:D is an important tool for monitoring the progression of glaucoma, as loss of the retinal nerve fiber layer causes the cup to enlarge, leading to a higher C:D. Most normal individuals have a C:D of ~0.4, with ratios of 0.7 or greater occurring in only 2.5% of the population and raising suspicion for glaucoma (60).
Please see the Iowa Glaucoma Curriculum, a teaching site with 50 lectures covering topics related to glaucoma.
References:
Cell and flare is a clinical sign of white blood cells and protein, respectively, in the aqueous humor of the anterior chamber. Visualized by slit lamp examination, C/F indicates anterior uveitis, which is inflammation of the iris and/or ciliary body (45).
Please see the Iowa Glaucoma Curriculum, a teaching site with 50 lectures covering topics related to glaucoma.
Examples of anterior uveitis:
The conjunctiva is the clear mucous membrane lining the inner surface of the eyelids (palpebral conjunctiva) and anterior scleral surface (bulbar conjunctiva). These two segments of conjunctiva are continuous, functioning primarily to maintain hydration and lubrication of the ocular surface and eyelid. Additionally, this structure serves as a protective barrier against dust, debris, and infection (62).
Sclera is a layer of dense connective tissue that forms the white part of the eye. It forms the external protective coat of the eye and serves as an attachment for the extraocular muscles that control movement of the eyes (63)
Chronic angle closure glaucoma refers to slowly developing angle-closure glaucoma. This is a type of glaucoma which occurs when the iris blocks aqueous humor from exiting through the drainage angle in the eye. This ultimately leads to elevated ocular pressures, with risk of damage to the optic nerve. This disease is initially asymptomatic, often manifesting with severe damage only in the late stages of disease (64). Though the etiology is undefined, CACG is hypothesized to result from some combination of a large lens, thick iris, and/or a plateau iris (an iris with a configuration that blocks fluid drainage) (65). Treatment options include topical medications, laser procedures, and/or glaucoma surgeries (66).
For further information regarding medical management of glaucoma see: Medical management of glaucoma: a primer
References:
Carbonic anhydrase inhibitors are glaucoma medications that function as direct antagonists of carbonic anhydrase, a ciliary body enzyme that is responsible for production of aqueous humor. These medications work to decrease intraocular pressure. Systemic carbonic anhydrase inhibitors (e.g., acetazolamide, methazolamide) have limited use given their extensive side-effect profile, such as extremity numbness or tingling, nausea, metallic taste, anorexia, malaise, increased urination, among others. Topical carbonic anhydrase inhibitors (e.g., dorzolamide, brinzolamide) are better tolerated and more commonly used, often as part of a combination drop (67).
Topical CAIs are often used for treatment of cystoid macular edema (CME) for inherited retinal degenerations, such as retinitis pigmentosa (RP) or X-linked retinoschisis (XLRS) (68). Systemic acetazolamide is commonly used as a treatment for idiopathic intracranial hypertension to reduce cerebral spinal fluid (CSF) production (and, thus, intracranial pressure). Patients with renal dysfunction or a history of kidney stones should avoid taking systemic CAIs, if possible.

For further information see : Medical management of glaucoma: a primer
For further information see : Medical management of glaucoma: a primer
Complexion-associated melanosis a benign, hyperpigmented lesion of the conjunctival epithelium. Complexion-associated melanosis occurs in darker skinned individuals and has no reported risk of progressing to conjunctival melanoma. Important clinical characteristics that differentiate complexion-associated melanosis from other pigmented lesions of the conjunctiva include bilateral occurrence, often perilimbal location, flat, non-cystic and dark skin pigmentation (69). CAM is confined to the conjunctiva and is now associated with feeder vessels that may be seen surrounding conjunctival melanomas.
Tutorial: Ocular surface tumors
Cancer-associated retinopathy is a rare retinal degenerative disease in which auto-antibodies cross react with tumor-tissue and retinal-tissue antigens. Recoverin and alpha-enolase are the most common retinal antigens to which autoantibodies develop. Oftentimes this autoimmune mediated retinal damage and associated visual loss occurs prior to the patient’s cancer diagnosis. Some of the most common presenting symptoms include photopsias, photophobia, scotomas, and/or loss of color contrast sensitivity. The most common cancers associated with cancer-associated retinopathy include small cell lung carcinoma, breast cancer, and gynecologic cancer. Treatment consists primarily of long-term immunosuppression (70).
The ciliary body is a uveal structure composed of muscle, vessels, epithelium and autonomic neural tissue (71). This structure serves several functions, including production of aqueous humor and suspension of the lens via the ciliary zonules. Additionally, it contains the ciliary muscle responsible for accommodation, changing the shape of the lens to allow the eye to focus on near objects (72)
Endocyclophotocoagulation (ECP) involves cyclodestruction of the ciliary body epithelium to reduce aqueous production and therefore IOP. Review this tutorial on minimally invasive glaucoma surgery for more information.
Case: Ciliary body melanoma
A complete blood count is a blood test that measures several components of the blood. This includes red blood cells (responsible for carrying oxygen), white blood cells (fight infection and mediate the immune response), hemoglobin (protein in red blood cells that carries oxygen), hematocrit (ratio of red blood cell volume to total blood volume), and platelets (involved in clotting).
CBC should be checked in any case of suspected non-accidental trauma of a child to rule out blood dyscrasias. Anemia (low hemoglobin) should be ruled out in cases of presumed normal tension glaucoma or posterior ischemic optic neuropathy. CBC is commonly checked in uveitis or orbital inflammation cases to rule out lymphoma, systemic infection/inflammation, severe anemias, or an associated thrombocytopenia.
“With correction” refers to a measurement of visual acuity taken with refractive correction (i.e., glasses or contacts).
Video: Visual acuity testing
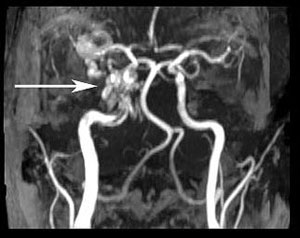
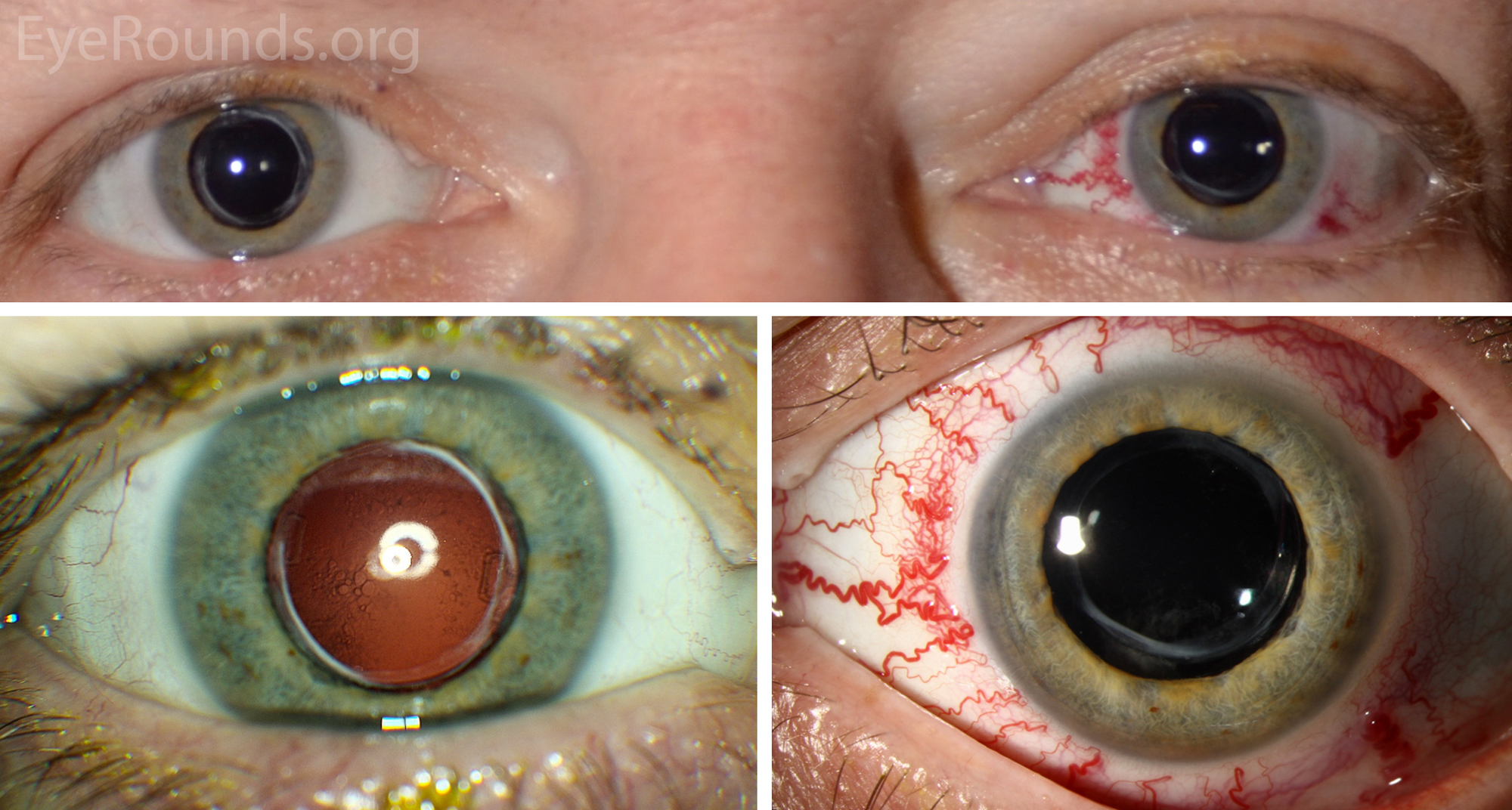
A carotid cavernous sinus fistula is an abnormal communication between the venous cavernous sinus and the internal carotid artery (ICA). This fistula often results in the triad of exophthalmos, epibulbar arterialized loops (“corkscrew” conjunctival vessels), and glaucoma. Examination may also find proptosis, orbital bruit, blood in Schlemm’s canal on gonioscopy, and/or retinopathy from venous congestion. Diagnosis is by clinical examination, computed tomography or magnetic resonance angiography, and/or catheter angiography.
There are two main types (73):
References:
Central corneal thickness refers to the thickness of the cornea at its center, measured by pachymetry. A normal central corneal thickness is considered to be 450 to 650 μm. The central corneal thickness may be decreased after surgical tissue ablation and in ectatic corneal diseases, such as keratoconus, pellucid marginal degeneration, or iatrogenic keratectasia. Lamellar or penetrating keratoplasty, corneal edema, cornea plana and other corneal dystrophies can cause increased central corneal thickness (75).
Cataract extraction is the removal of the opacified lens (cataract) from the eye and is generally divided into three overarching techniques: phacoemulsification, extracapsular cataract extraction (ECCE) and intracapsular cataract extraction (ICCA).
There are numerous cataract and intraocular lens videos on EyeRounds.org: Cataract procedures.
References:
Cataract extraction with implantation of intraocular lens refers to the entire cataract procedure with removal of the opacified lens (cataract) from the eye and subsequent replacement with a synthetic lens. Cataract surgery is the most common procedure in the United States (76).
There are numerous cataract and intraocular lens videos on EyeRounds.org: Cataract procedures.
References:
Count fingers is a measure of visual acuity (VA) used when a patient is unable to use or read a Snellen chart to test vision, usually due to profound vision loss. Notation demonstrates the distance from which the patient can accurately count the number of figures on the examiner’s hand. For example, “CF 4” indicates the patient’s ability to count fingers on the examiner’s hand at four feet (77).
References:
Congenital hereditary endothelial dystrophy is an autosomal dominant (CHED 1) or recessive (CHED 2) condition characterized by bilateral corneal clouding. Present at birth or developing in infancy, this condition is the result of endothelial dystrophy with subsequent corneal edema and visual disturbance. Treatment is often surgical, though mild corneal edema may be managed with hypertonic sodium chloride drops.
Like Fuchs endothelial dystrophy and posterior polymorphous dystrophy (PPMD), CHED is thought to result from a defect in terminal differentiation of neural crest with altered morphology or endothelial cells (78).
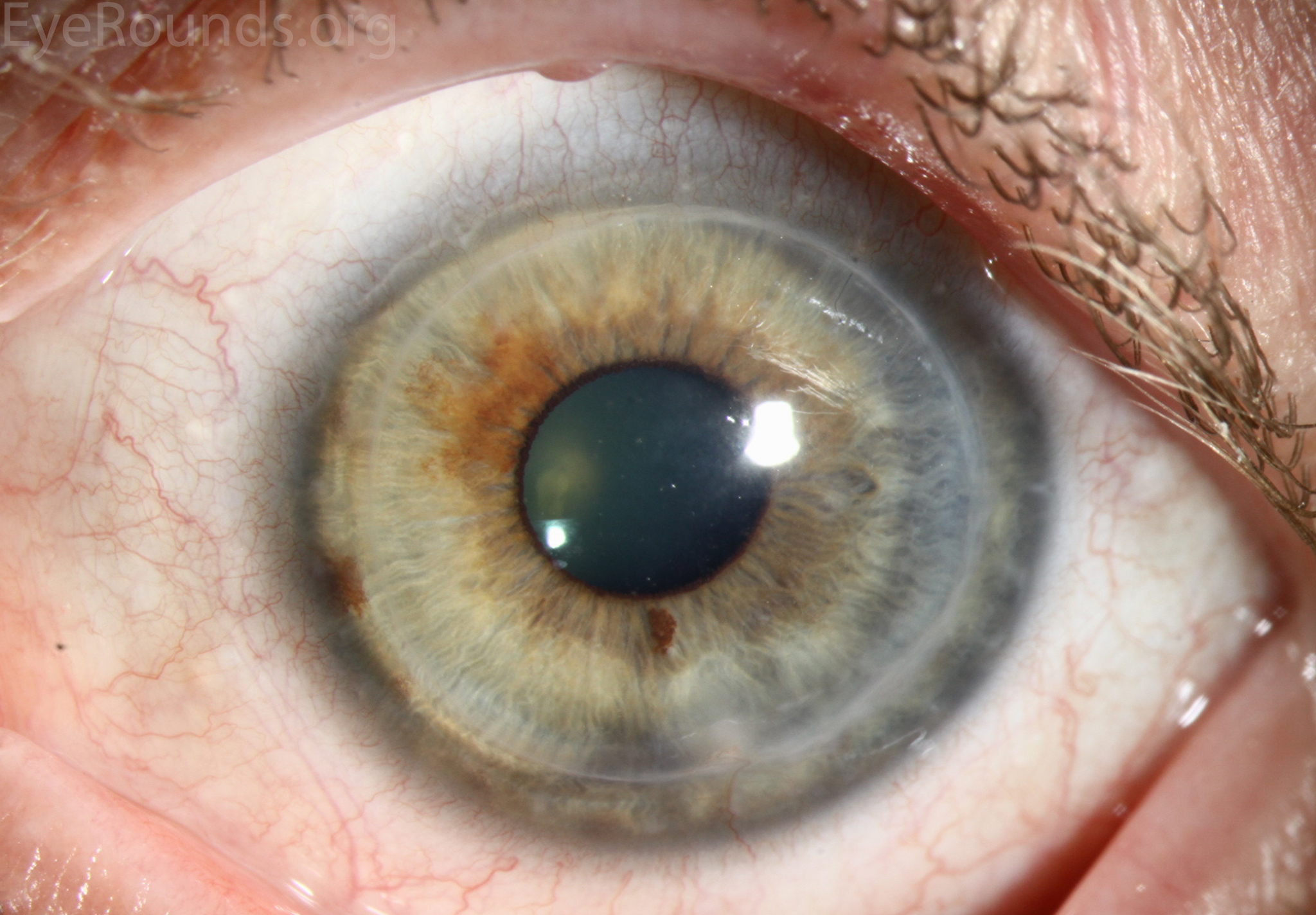
Congenital hypertrophy of the retinal pigment epithelium (RPE) are benign, solitary, flat, well-demarcated, hyperpigmented lesions of the retina (79). These lesions are composed of hypertrophied RPE and are lined by degenerated photoreceptors. Generally, this is an asymptomatic finding on exam. Bilateral CHRPE lesions should raise suspicion for Gardner’s syndrome, which is an autosomal dominant condition that is associated with colon cancer.
References:
Congenital hereditary stromal dystrophy is an autosomal dominant disease resulting in central corneal clouding without corneal edema, yet the peripheral cornea remains clear. This disease presents at birth with bilateral clouding resulting in moderate to severe vision loss. Treatment generally involves penetrating keratoplasty (80).
Corneal clouding has a long differential diagnosis that can be remembered as “STUMPED.” Review the case on Peters anomaly to explore these other diagnoses.
Chlorhexidine is an antiseptic medication with several uses in ophthalmology, including as a disinfectant for soft contact lenses and as treatment for Acanthamoeba keratitis (AK). It is a biguanide that may be prescribed at a concentration of 0.02% for use every hour in the early treatment course for amoeba eradication. Though it is generally well tolerated, ocular toxicity has limited its use in the United States (81).
Conductive keratoplasty is a refractive procedure used to correct moderate hyperopia (farsightedness). In this procedure areas of the cornea are heated to induce collagen shrinkage and change in corneal shape (82).
References:
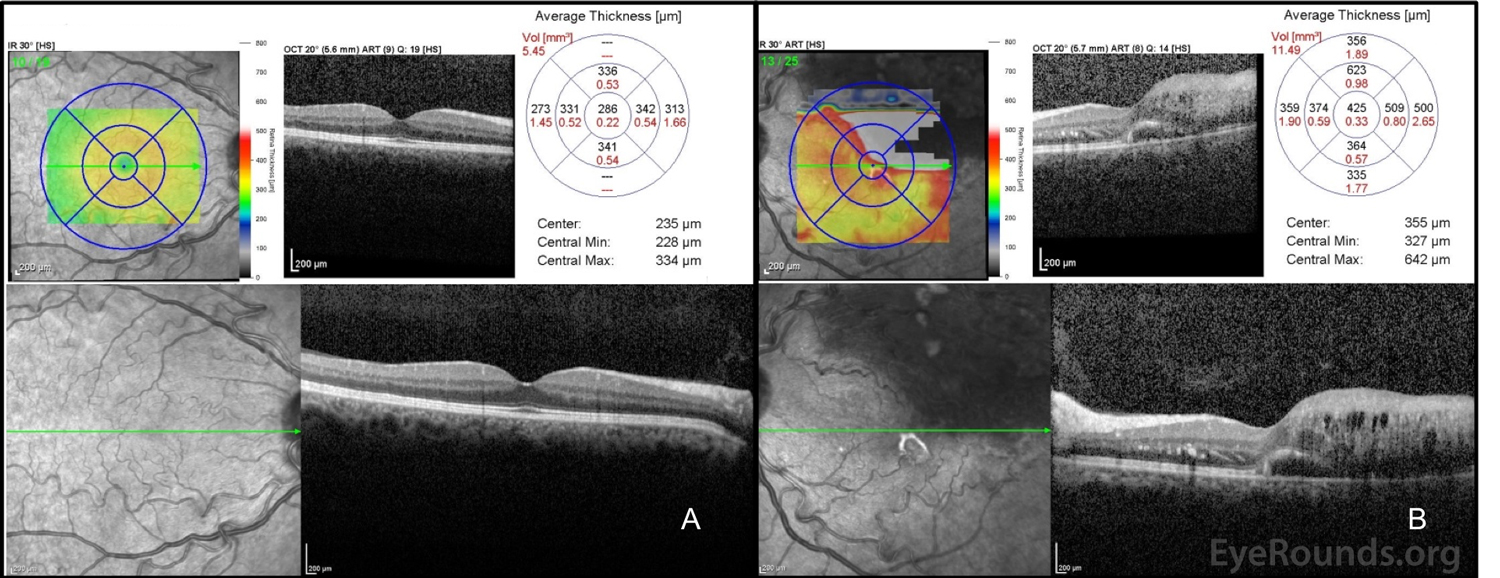
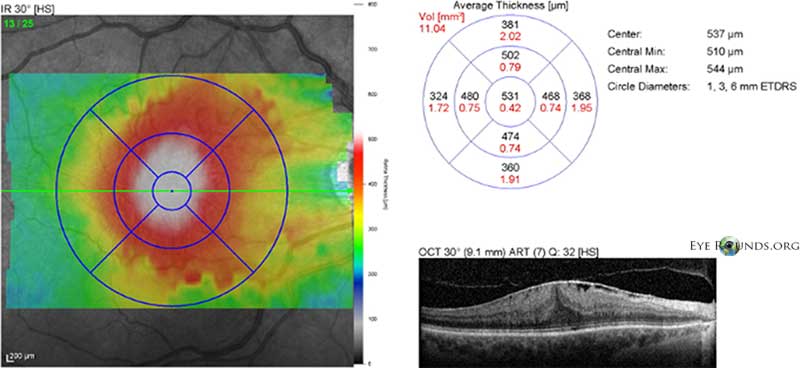
Central macular thickness is a measure of the thickness of the retina at the center of the macula or fovea. This metric is determined with optical coherence tomography (OCT) mapping software.
Cytomegalovirus is an opportunistic infection that can affect the eye, particularly in AIDS patients (usually when CD4 lymphocyte count is < 50) and others with profound immunosuppression. CMV retinitis is the most common ocular manifestation, beginning as white, perivascular retinal infiltrates or dot-blot hemorrhages (DBH) that may progress to full thickness retinal necrosis that follows the retinal vasculature. Less common findings include vitritis, anterior segment cell and flare (C/F), or fine keratic precipitate (KP). Retinal detachments are common in these patients. Treatment may include ganciclovir, foscarnet, valganciclovir, and/or cidofovir (intravenous or intravitreal) (84). In active ocular disease, intravitreal injections are recommended every 72 hours (at least twice weekly). Systemic therapy using involves an induction phase followed by maintenance dose of anti-viral therapy.
References:
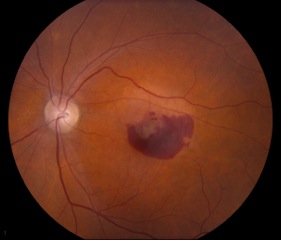
A choroidal neovascular membrane is the result of blood vessel growth beneath the retina as a result of a break in Bruchs membrane. These new vessels can extend into the retina or in the subretinal space, causing leakage, subretinal hemorrhage, and/or vision loss. Choroidal neovascular membranes can be secondary to neovascular (or wet) age-related macular degeneration, presumed ocular histoplasmosis syndrome (POHS), pseudoxanthoma elasticum (PXE), choroidal rupture from trauma,

References:
Cyclophotocoagulation is a class of laser procedures utilized to lower the pressure in the eyes in certain glaucoma patients. There are several such procedures currently in use, including transpupillary CPC, transvitreal endophotocoagulation, transscleral CPC, and endoscopic CPC. Each of these procedures induce damage to the ciliary body (CB), reducing aqueous humor production and subsequently reducing intraocular pressure (86).
References:
Chronic progressive external progressive ophthalmoplegia is a hereditary weakness of the extraocular muscles that causes progressive ptosis and ophthalmoplegia. Most often caused by a single deletion in mitochondrial DNA, this disease is often diagnosed in the fourth or fifth decade, though may manifest in early childhood and infancy as well. Biopsy of the affected muscles yields ragged red fibers. Treatment is surgical (e.g., ptosis repair), though not curative (87).
Kearns-Sayre syndrome is characterized by the clinical features of CPEO combined with pigmentary retinopathy, complete heart block, and cerebellar ataxia. Thus, all patients with CPEO should be evaluated with an EKG and additional cardiac work-up.
References:
Continue present management is an acronym commonly used in the “plan” section of a clinic note, indicating that no changes to the patient’s treatment or follow-up plan were made from the prior visit.
Creatinine is a natural breakdown product of muscle that is filtered from the blood by the kidneys. As such, serum and urine creatinine tests are commonly used to evaluate kidney function. An elevated serum creatinine level may be indicative of poor kidney function, as the kidneys are unable to adequately remove the waste product from the blood (89).
See the below links to learn more about ocular diseases that often have abnormal blood urea nitrogen (BUN) or creatinine levels due to kidney dysfunction.
Associated pathologies:
Central retinal artery occlusion occurs when blood flow within the central retinal artery is blocked. The central retinal artery is a branch of the ophthalmic artery and supplies blood flow to the inner retina. As such, disruption of this blood supply typically results in profound, painless vision loss. A cherry red spot over the fovea is a classic exam finding and is often accompanied by vascular attenuation and occasionally visualization of an embolus. Common risk factors include hypertension, hypercholesterolemia, diabetes, vascular disease, prior myocardial infarction, cardiac stenting, transient ischemic attacks, and stroke (90). Giant cell arteritis (GCA) should be ruled out, and work-up includes neurology consult and carotid imaging. Further work-up and management of CRAOs are discussed here.
Kearns-Sayre syndrome is characterized by the clinical features of CPEO combined with pigmentary retinopathy, complete heart block, and cerebellar ataxia. Thus, all patients with CPEO should be evaluated with an EKG and additional cardiac work-up.
References:
C-reactive protein is an inflammatory marker, commonly measured as part of a blood test. Elevated C-reactive protein (usually greater than 2.0 milligrams per liter; the exact value is lab dependent) may be indicative of an infection, such as orbital cellulitis, or inflammatory diseases, such as giant cell arteritis (GCA), orbital myositis, lupus, or rheumatoid arthritis (91).
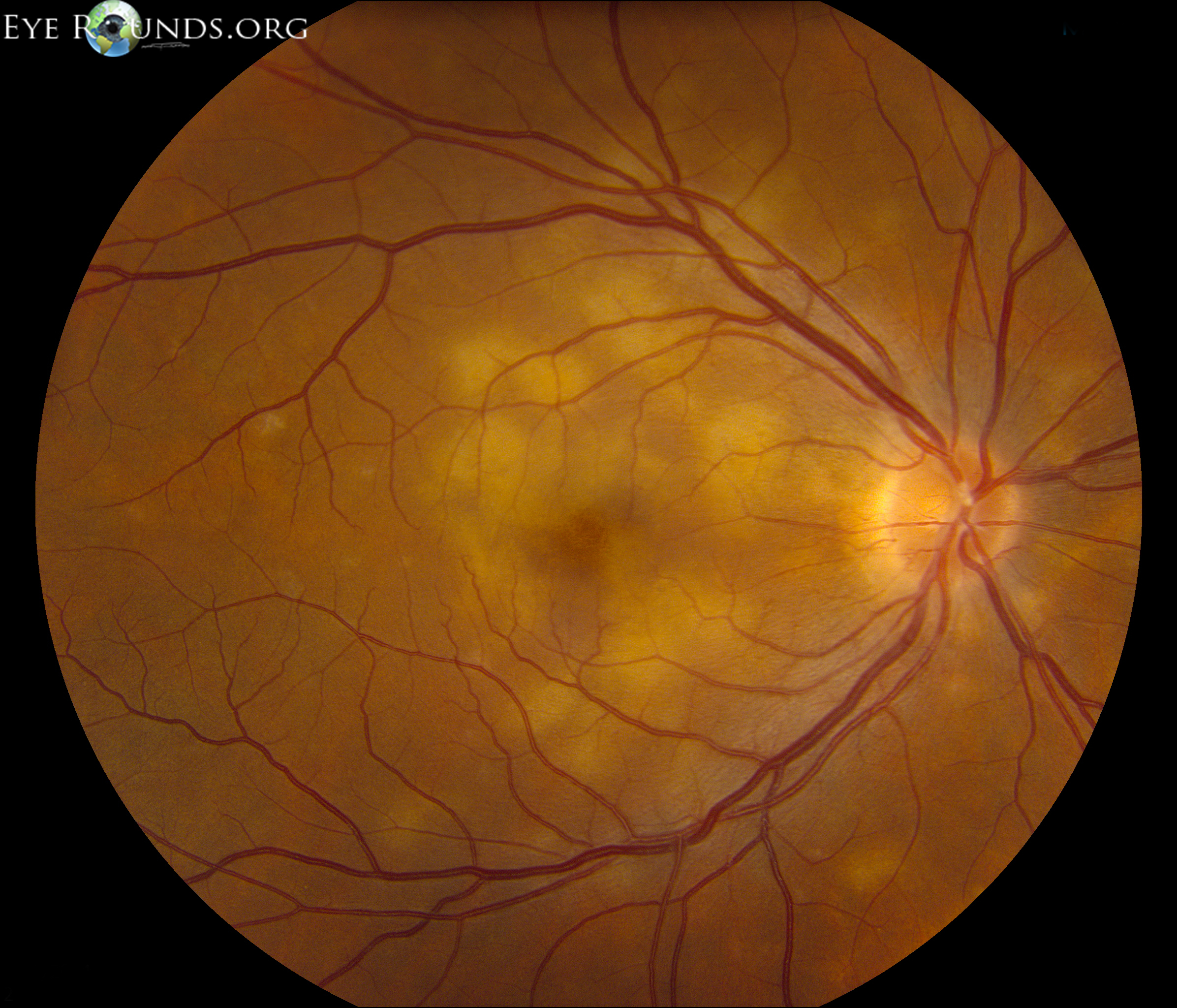
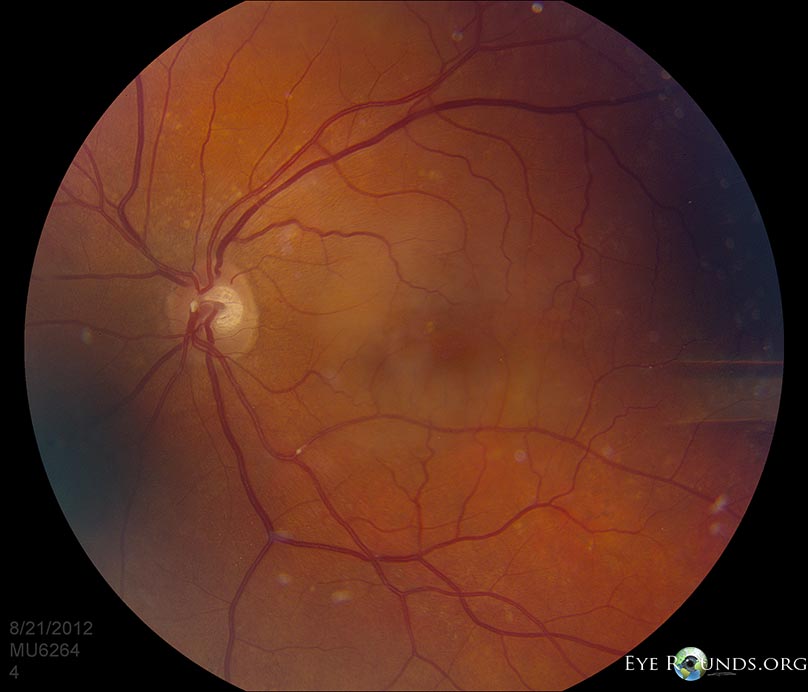
Central retinal vein occlusion is blockage of blood flow through the central retinal vein, the main vein draining the retina vessels. Occlusion may result in macular edema, retinal ischemia, and/or ocular neovascularization (NV). Patients typically present with unilateral, sudden, painless vision loss. Findings on exam include engorgement and tortuosity of the retinal veins with intraretinal and superficial nerve fiber layer hemorrhages, often described as a “blood and thunder” appearance of the fundus. The etiology is most likely related to stagnant flow and formation of a thrombus in the central retinal vein lumen (92).

References:
Cycloplegic refraction is a technique used to measure the complete refractive error of the eye. This is done with the use of cycloplegic drops, which relax the ciliary muscle, thereby inhibiting accommodation by the lens. Though there are numerous reasons to utilize cycloplegic refraction, the technique is most routinely used in children due to their inherently large amplitude of accommodation (94).
References:
Cryotherapy is a freezing procedure used to treat a number of eye conditions. This is done by placing a probe with cold gases (such as nitrous oxide) on the intended surface to induce freezing and cellular destruction. Examples of uses include treatment for retinal tears and detachments as well as for eyelash follicle destruction (95). Techniques for using a cryoprobe can be found at the below links.

References:
Cortical spoking (also known as cuneiform opacities) is an exam finding commonly associated with cortical cataracts. These are wedge-shaped opacities which form at the periphery of the lens as the cortical lamellae become separated with fluid. When viewed directly with a slit lamp, the cortical spokes appear as white opacities, but appear as dark shadows upon retroillumination (97).

References:
Central serous chorioretinopathy (also known as central serous chorioretinopathy, CSCR) leads to serous detachment of retina and often affects the macula and posterior pole. Mostly affecting young adult and middle age men, this process presents with a “smokestack” or “ink blot” pattern of choroidal leak on fundus fluorescein angiography (FFA). Ninety percent of patients experience spontaneous recovery without significant vision loss, though some patients may require treatment with laser photocoagulation or photodynamic therapy (PDT). Anti-VEGF injections may be offered in the event of an associated choroidal neovascular membrane (CNVM) (99). Patients should be instructed to avoid steroids, when possible, as steroid use (topical/creams, injections, inhalers, etc.) are associated with increased CSR activity. Further, CSR patients should minimize stress, treat sleep apnea, and avoid testosterone use.

References:
Clinically significant diabetic macular edema is defined by the Early Treatment Diabetic Retinopathy Study (ETDRS) as: “retinal thickening within 500 µm of the macular center; hard exudates within 500 µm of the macular center with adjacent retinal thickening; and/or one or more disc diameters of retinal thickening, part of which is within one disc diameter of the macular center.” Macular edema may cause decreased visual acuity (VA) and metamorphopsia. The presence of clinically significant diabetic macular edema is the accepted prerequisite to initiate treatment with focal laser photocoagulation and/or anti-VEGF therapy in patients with diabetic retinopathy (101).
References:
Central, steady, maintain is an approach to measuring visual acuity in children too young to use Allen pictures (103).
Clinically significant macular edema is defined by the Early Treatment Diabetic Retinopathy Study (ETDRS) as: “retinal thickening within 500 µm of the macular center; hard exudates within 500 µm of the macular center with adjacent retinal thickening; and/or one or more disc diameters of retinal thickening, part of which is within one disc diameter of the macular center.” Although commonly associated with diabetes, macular edema may also be related to a branch retinal vein occlusion, age-related macular degeneration, etc. The presence of clinically significant macular edema is the accepted prerequisite to initiate treatment with focal laser photocoagulation and/or anti-VEGF therapy (101).
References:
Congenital stationary night blindness is a collection of non-progressive genetic diseases that affect the photoreceptors (PR), retinal pigment epithelium (RPE), or bipolar cells. This cluster of diseases generally results in difficulties with vision in dark or dim-lit settings since birth. CSNB patients may inherit this disorder in an X-linked, autosomal dominant, or autosomal recessive fashion. There are two main categories, Riggs-type and Schubert-Bornstein. Diagnosis relies primarily of electroretinography (ERG), classically with an electronegative ERG (i.e., reduced b wave). While there is no current treatment, gene therapy and photoreceptor replacement are currently under investigation (104).
Associated conditions: Oguchi disease and fundus albipunctatus
References:
Confrontation visual field testing is utilized in clinic or bedside to assess the patient’s visual fields. This is done by having the patient look directly at the examiner’s nose while asking them to count the number of fingers presented in each of the primary visual fields. This is done with one eye at a time, with the other eye covered (105).
References:
Cotton wool spots are a classic exam finding in patients with diabetic retinopathy and hypertensive retinopathy, though may also occur in other ischemic, inflammatory, neoplastic and iatrogenic causes. These lesions are infarctions of the retinal nerve fiber layer and manifest as fluffy, white lesions (46).
References:
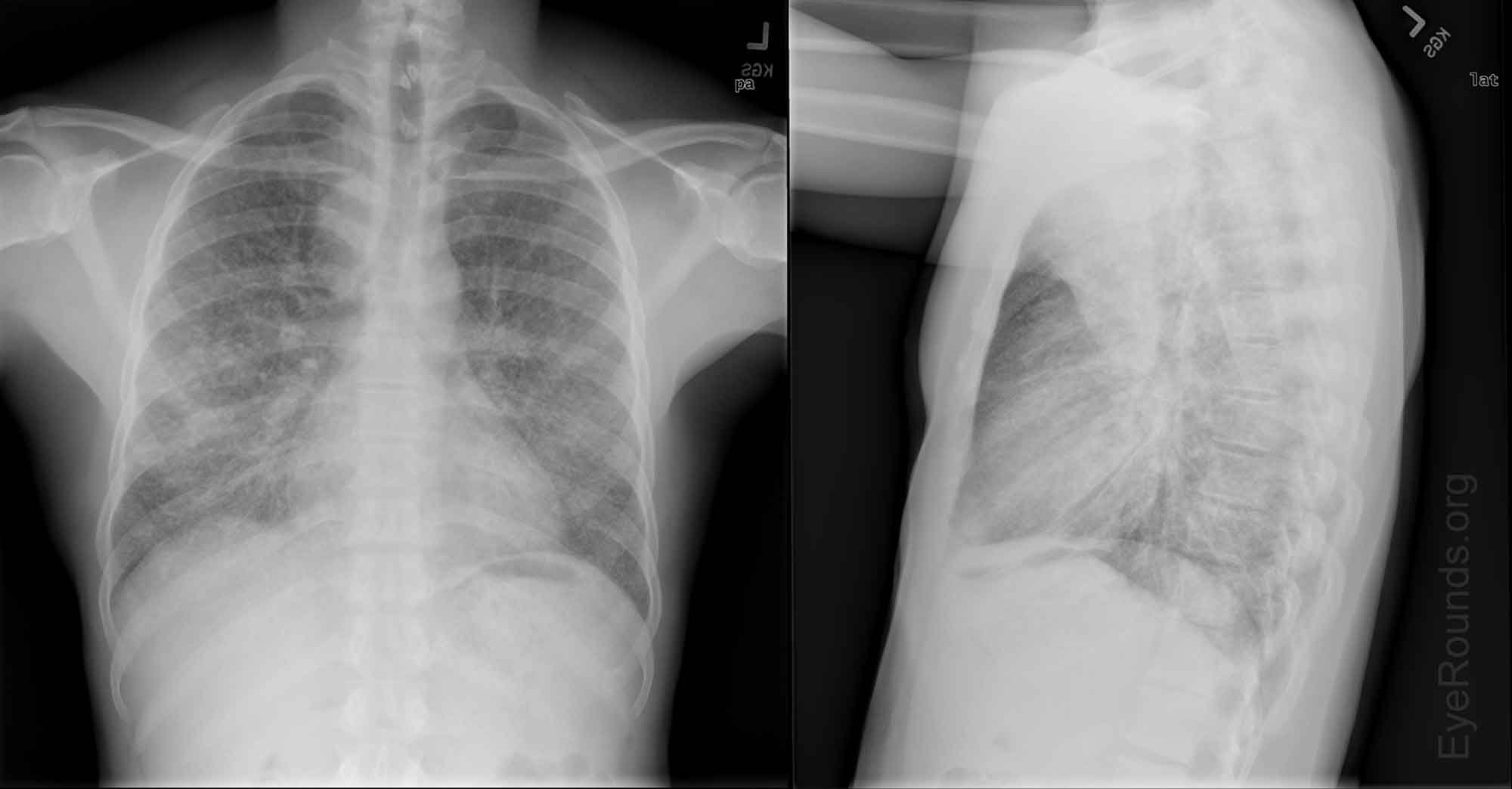
A chest x-ray is used to image the heart, lungs, blood vessels, airways, and bones of the chest. CXR is commonly ordered in the work-up of uveitis to rule out hilar lymphadenopathy associated with sarcoidosis.
References:
The cylinder component of an eyeglass prescription refers to the cylindrical or toric lens used to correct astigmatism. This is conventionally the second number in the glasses prescription. There are two different notations for indicating the cylinder strength: plus cylinder notation and minus cylinder notation (108).
References:
Diopter (D) is a unit of measure used to describe the refractive error of the eye as well as the power of ophthalmic lenses. A diopter is defined as a unit of lens power equal to 1/focal length of the lens in meters, 100/focal length of the lens in centimeters, or 40/focal length of the lens in inches. In eye care, quarter diopter units of power is used by convention (109).
References:
D/C refers to the discontinuation of a medication. For example, ophthalmologists are commonly consulted to determine if patients on hydroxychloroquine (plaquenil) have developed hydroxychloroquine toxicity. Discontinuing this medication may be warranted if there is decreased vision, visual field changes, or clinical changes, such as RPE or outer retinal loss.
Deep and quiet is used to describe a normal anterior chamber that appears deep, with no evidence of angle closure, and quiet, with no evidence of inflammation (e.g., cell or flare).
Gonioscopy.org is a wonderful resource to review videos of normal and abnormal angles.
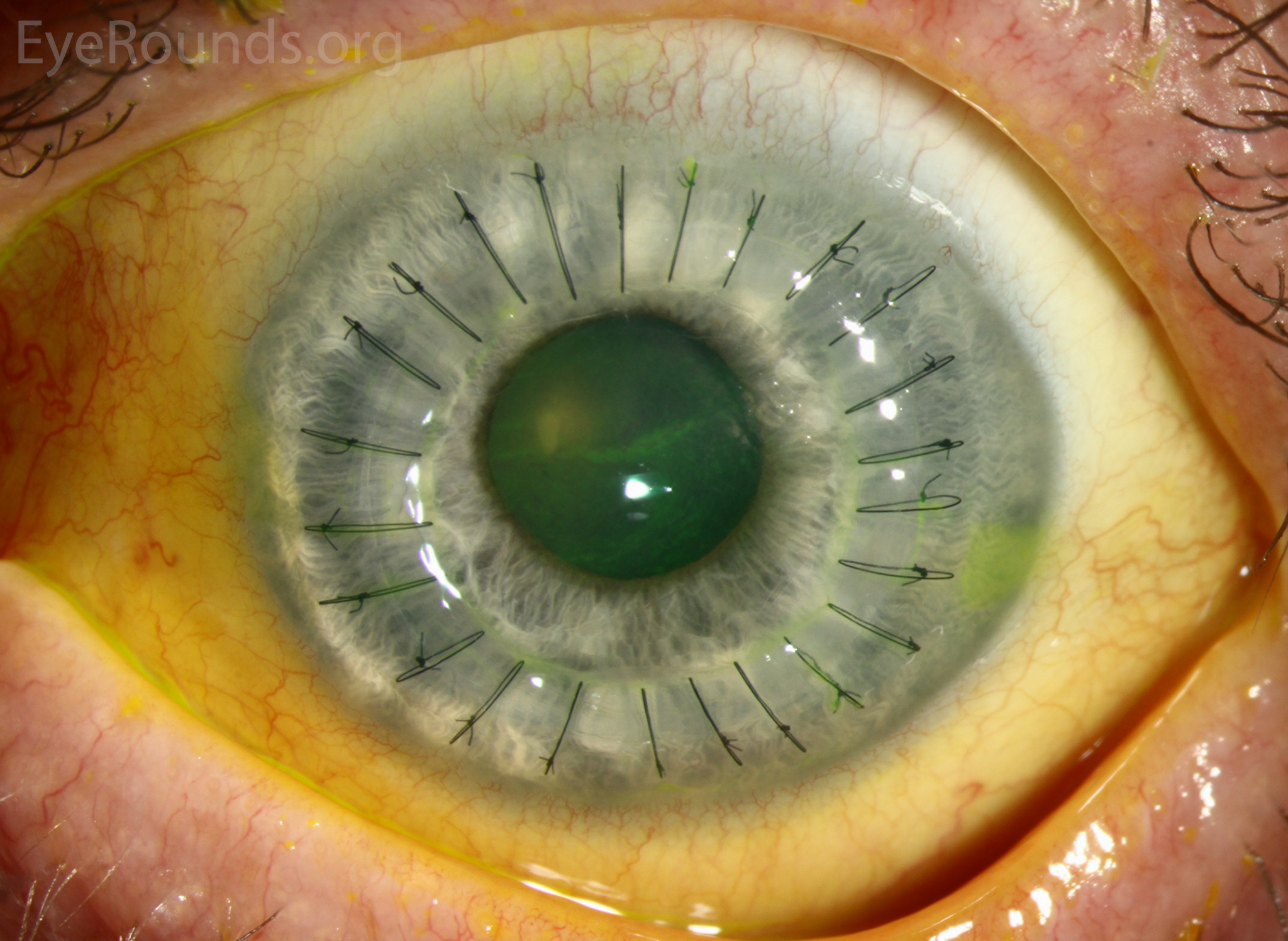
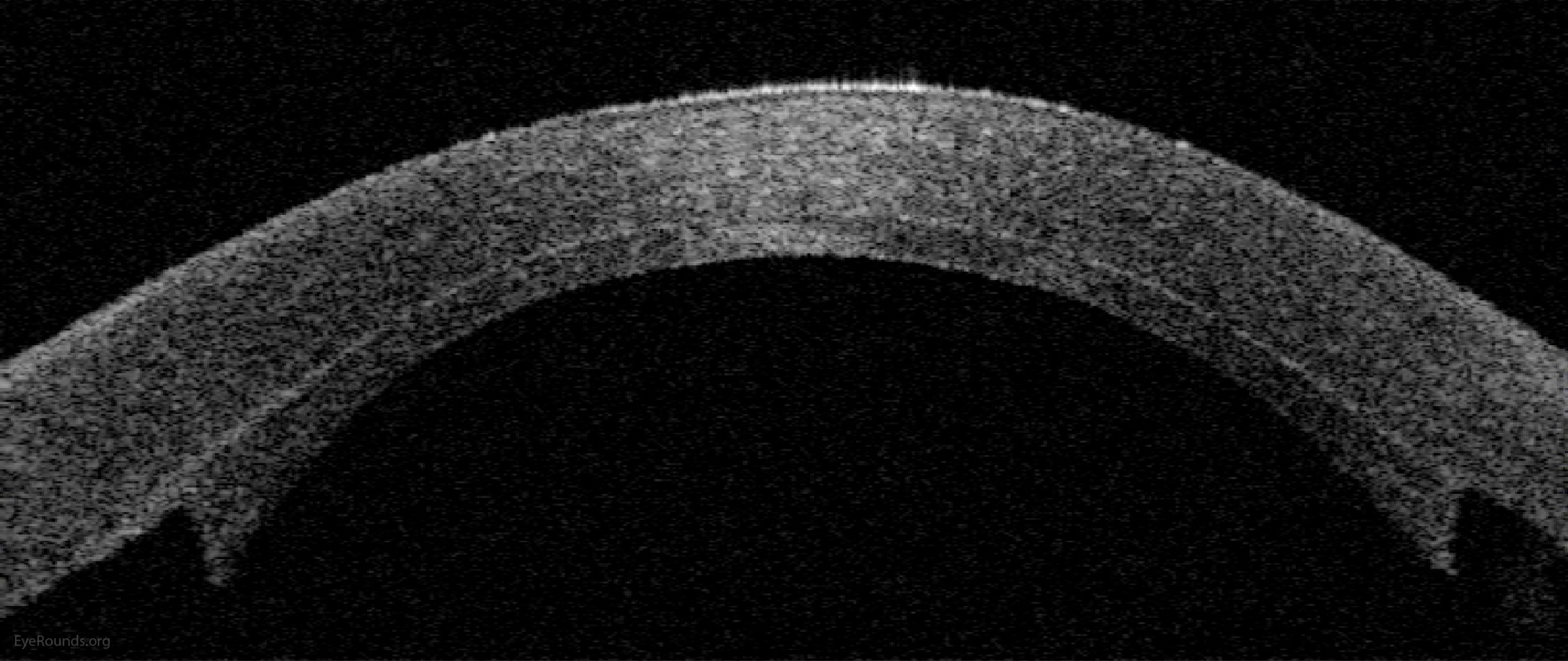
Deep anterior lamellar keratoplasty is a partial-thickness cornea transplant procedure that involves selective transplantation of the corneal stroma, leaving the descemet membrane and endothelium in place. A trephine with an appropriate diameter is used to make a partial-thickness incision into the patient’s cornea, followed by pneumodissection or manual dissection of the anterior stroma. The dissection step is followed by placement of a graft prepared from a full-thickness punch in which the donor endothelium-Descemet membrane complex has been removed. The graft is secured with interrupted and/or running sutures, and these are then selectively removed post-operatively.
DALK is useful for processes involving the corneal stroma in the presence of healthy endothelium. Examples of ocular disease states that may require DALK include corneal ectasia, corneal scars that are not full-thickness, and corneal stromal dystrophies.
References:
Dot-and-blot hemorrhages occur when blood accumulates in the outer plexiform and/or inner nuclear layers, and have a dot-like appearance. Hyperglycemia and hypertension result in weakened retinal capillary walls and microaneurysms that can rupture to form these hemorrhages deep within the retina. Thus, DBHs are more commonly seen in association with hypertension (HTN) or diabetic retinopathy (DR).
Review the diabetic retinopathy tutorial to determine the “4-2-1 rule” for classification of severe non-proliferative diabetic retinopathy and how this relates to the location and number of DBHs.

References:
Dacryocystorhinostomy is a procedure for nasolacrimal duct obstruction (NLDO) that creates an anastomosis between the lacrimal sac and the nasal mucosa via a bony ostium in the nose (112, 113).
Review this case of sarcoidosis causing NLDO for an overview of the many diagnoses that can lead to acquired NLDO.
References:
A disc diameter refers to the mean diameter of the optic disc, as evaluated from fundus photographs and examination. A normal disc diameter is approximately 1.5mm to 2mm (114). It is common in ophthalmology to describe a choroidal or retinal lesion or finding by the size in “disc diameters.” For instance, a choroidal nevus may be two disc diameters (or 2dd), indicating the nevus appears twice the size of the optic nerve.
Review this case of sarcoidosis causing NLDO for an overview of the many diagnoses that can lead to acquired NLDO.
Dry eye syndrome, or keratoconjunctivitis sicca (KCS), is a condition where A) the aqueous component of tears is inadequate; B) there is excessive tear evaporation; or C) there is a combination of A and B. DES is often due to meibomian gland dysfunction and associated blepharitis.
Please review this comprehensive evaporative dry eye tutorial to learn more about dry eye diagnosis and management.
References:
Dilated fundus examination is a procedure that employs the use of eye drops (e.g. tropicamide and phenylephrine) to dilate the pupil to obtain a better view of the fundus of the eye. The fundus may be examined by indirect or direct ophthalmoscopy. Indirect ophthalmoscopy is performed using non-contact fundus lenses. The specific lens is chosen based on the need for a specific magnification and/or field of view.
References:
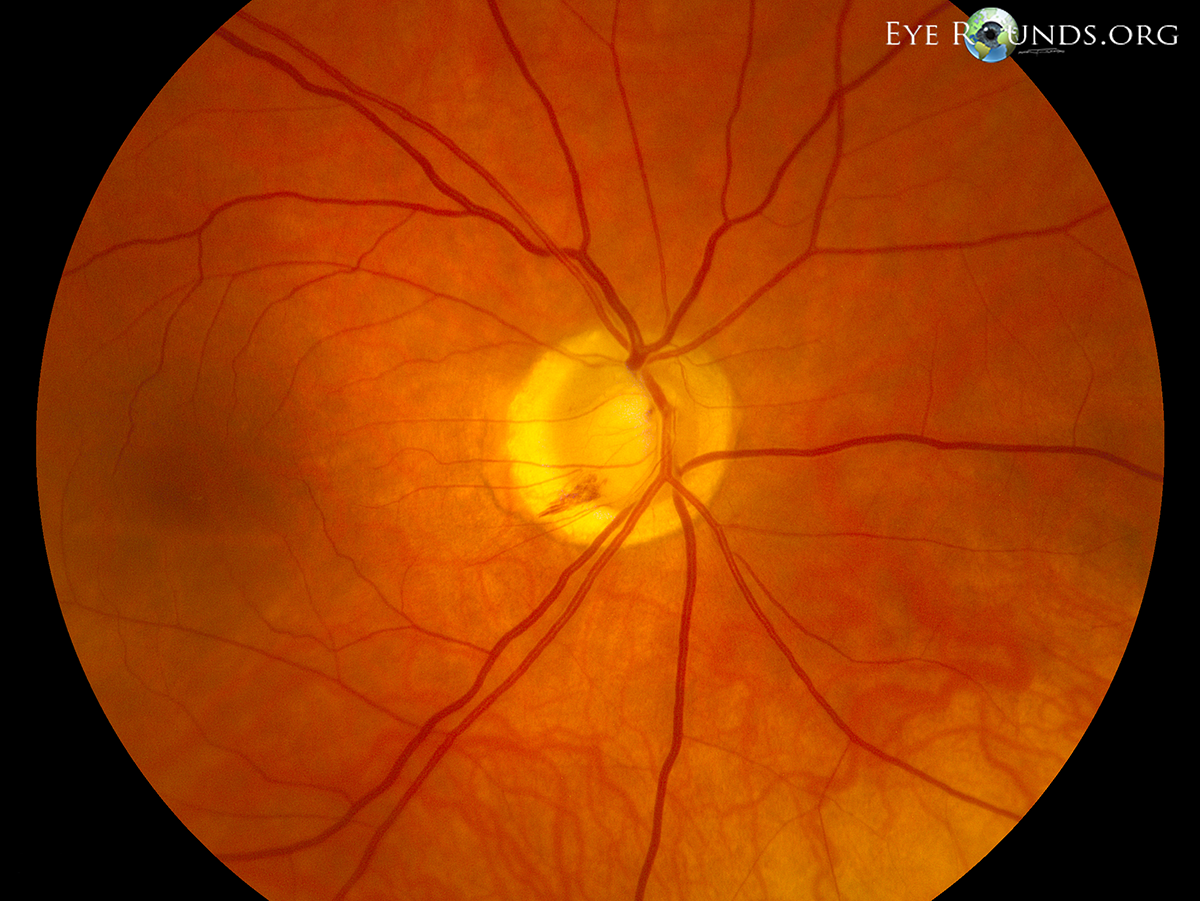
Disc hemorrhages usually occur at the border of the optic disc in the retinal nerve fiber layer (RNFL). DHs are often seen in glaucoma indicating that the disease is active and possibly progressing. There is some evidence that DH is a prognostic factor for the onset and progression of visual field loss. Fundus examination, as well as optic disc photography, should be done regularly to reliably detect DHs. A typical DH in an eye with glaucoma appears as a splinter-like or flame-shaped hemorrhage (115).
Intrapapillary hemorrhages may be related to disc edema, myopia, valsalva, or vitreopapillary traction.
References:
Deep lamellar endothelial keratoplasty is a surgical method of endothelial replacement that is performed through a limbal scleral incision that leaves the surface of the recipient cornea untouched to preserve normal topography with the result of minimal refractive astigmatism (117).
However, DLEK is technically difficult to perform, requires extensive manual lamellar dissection, and has not been adopted widely. Review this corneal transplantation tutorial for an overview of all types of keratoplasties.
References:
Diffuse lamellar keratitis is a type of inflammation that can occur in the first few days after LASIK surgery and requires prompt treatment with topical steroid drops and possibly re-lifting the LASIK flap, depending on the degree of inflammation (118).
References:
Diabetes mellitus is a group of metabolic disorders characterized by elevated blood glucose levels over a prolonged period. Hemoglobin A1C provides an important measure for diagnosis and monitoring of diabetes and may be an important predictor of retinopathy. A1C values above 6.5% are often considered abnormal, suggesting chronic hyperglycemia (4). Increased hemoglobin A1C levels are associated with increased microvascular complications of diabetes, including neuropathy, nephropathy, and retinopathy (5). Intensive glycemic control should be encouraged since lower A1C levels decrease the progression of diabetic retinopathy (6).
References:
Diabetic macular edema is the most frequent cause of vision loss related to diabetes (119, 120). DME can result in diffuse or focal areas of swelling and retinal thickening, and may be associated with hard exudates (102). Clinically significant diabetic macular edema is defined by the Early Treatment Diabetic Retinopathy Study (ETDRS) as: “retinal thickening within 500 µm of the macular center; hard exudates within 500 µm of the macular center with adjacent retinal thickening; and/or one or more disc diameters of retinal thickening, part of which is within one disc diameter of the macular center.” Macular edema may cause decreased visual acuity (VA) and metamorphopsia. The presence of clinically significant diabetic macular edema is the accepted prerequisite to initiate treatment with anti-VEGF drugs, as well as focal or grid pattern laser photocoagulation.
References:
The double Maddox rod test is used to determine cyclodeviations in which the eye is abnormally rotated by incyclotorsion or excyclotorsion (121). A Maddox rod is placed in a trial frame or phoropter and positioned in front of each eye with the rods aligned vertically so that the patient sees horizontal line images. The patient or examiner rotates the axes of the rods until the lines are perceived to be parallel. To facilitate the patient’s recognition of the two lines, it is often helpful to dissociate the lines by placing a small prism base-up or base-down in front of 1 eye. The degrees of deviation and the direction (incyclo or excyclotorsion) can be determined by the angle of rotation that causes the line images to appear horizontal and parallel.
Abnormal cyclotorsion is common in cranial nerve IV palsies, dorsal midbrain syndrome, cavernous sinus syndrome, among others.
Dorsal midbrain syndrome, also known as Parinaud syndrome, is a usually sporadic condition that presents with a collection of signs and symptoms, including limited conjugate upgaze and convergence-retraction nystagmus, which is characterized by an irregular, jerky nystagmus with convergence and retraction of both eyes on attempted upgaze. There is commonly pupillary hyporeflexia or poor pupillary constriction to light but preserved constriction with convergence (i.e., light near dissociation) (122, 123). Patients may also present with lid retraction in the primary position (Collier’s sign).
The causes of Parinaud syndrome include pineal gland tumors, midbrain infarctions, multiple sclerosis (MS), midbrain hemorrhage, encephalitis, arteriovenous malformations (AVM), infections (e.g., toxoplasmosis), trauma, obstructive hydrocephalus, and, sometimes, tonic-clonic seizures. Treatment is primarily directed towards the etiology of dorsal midbrain syndrome. A thorough work-up including neuroimaging is essential to rule out the various causes of dorsal midbrain syndrome.
References:
Acetazolamide, or diamox, is a carbonic anhydrase inhibitor (CAI) that is commonly used in clinical practice as an immediate and readily available option for acute reduction of intraocular pressure (IOP) (124). Carbonic anhydrase inhibitors are glaucoma medications that function as direct antagonists of carbonic anhydrase, a ciliary body enzyme that is responsible for production of aqueous humor. The most common side effects associated with the use of oral acetazolamide include fatigue, paresthesias of the face and extremities, metallic taste in the mouth, and nausea and/or vomiting, which are related to drug-induced metabolic acidosis. Other complaints may include dizziness, increased urination, weight loss, depression, and/or intestinal colic.
Systemic acetazolamide is also commonly used as a treatment for idiopathic intracranial hypertension to reduce cerebral spinal fluid (CSF) production (and, thus, intracranial pressure). Patients with renal dysfunction or a history of kidney stones should avoid taking systemic CAIs, if possible.

For further information see Medical management of glaucoma: a primer
Autosomal dominant optic atrophy (Kjer syndrome) is the most common inherited optic neuropathy. This autosomal dominant condition is the result of a mutation in the OPA1 gene, leading to mild to moderate bilateral vision loss with typical onset in childhood. Most patients maintain vision better than 20/200, while some patients may also present with color vision deficits (125, 126).
References:
Doxycycline (or doxy), similar to other tetracycline medications, is commonly used for eye diseases, including blepharitis, ocular rosacea, corneal inflammatory diseases, corneal infections, adult chlamydial conjunctivitis, ocular bartonellosis, and meibomian gland dysfunction (MGD) not controlled with eyelid hygiene (127-129).
Doxy is usually started at 100 milligrams twice daily (BID) and gradually reduced or stopped over time. The most common side effects of doxy are upset stomach and increased sensitivity to sunlight. Less frequently, skin rashes and hypersensitivity reactions have been reported. Doxy should not be used in the last half of pregnancy, in infants, or in children under the age of 8 because it may cause permanent discoloration of the teeth. Nursing mothers should not take doxy as it may be transmitted to the infant in human milk. The safety of doxy in early pregnancy has not been established and should, therefore, not be used.
References:
Diabetic retinopathy is a vascular disease of the retina that affects patients with diabetes mellitus (DM). It is the number one cause of blindness in people between the ages of 20-64 in the United States (130). Nearly one-fourth of patients with DR have vision-threatening disease.
Hemoglobin A1C values above 6.5% are often considered abnormal, suggesting chronic hyperglycemia (4). Increased hemoglobin A1C levels are associated with increased microvascular complications of diabetes, including retinopathy (5). Intensive glycemic control should be encouraged since lower A1C levels decrease the progression of diabetic retinopathy (6).
References:
Descemet Stripping Automated Endothelial Keratoplasty is a partial thickness cornea transplant procedure that involves selective removal of the patient's descemet’s membrane and endothelium, followed by transplantation of donor corneal endothelium in addition to donor corneal stroma (110).
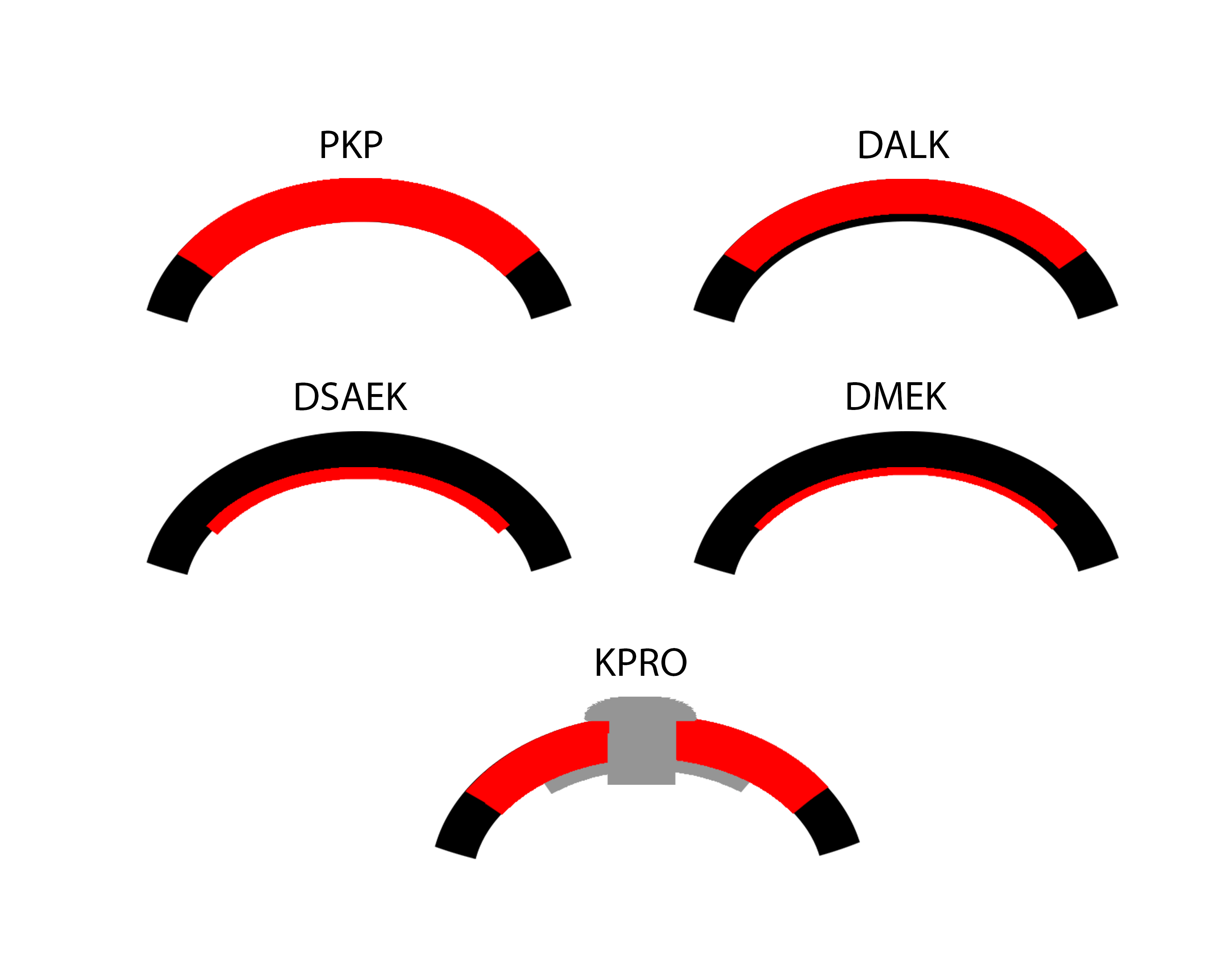
References:
Descemet's stripping endothelial keratoplasty is a procedure that involves replacing only the innermost layer of the cornea, rather than the entire thickness of the cornea, as is performed in standard full-thickness corneal transplantation (131). In DSEK, the patient’s descemet’s membrane is removed and replaced with a partial thickness graft that includes donor posterior Stroma, descemet’s membrane and endothelium (~20-30% of the inner donor cornea). Both donor and host cornea are manually dissected using the instruments seen here.
References:
Diffuse unilateral subacute neuroretinitis is a multifocal chorioretinitis caused by a nematode (132, 133). Recommendations usually include starting albendazole systemically and undergoing laser photocoagulation therapy to kill the nematode.

References:
Dissociated vertical divergence is an ocular motor disorder characterized by a slow, upward drift of one eye, either frequently or infrequently, when the other eye is fixating on a target (134). DVD may be present in one or both eyes, and the amount of drifting may vary during the course of the day.
DVD occurs in more than half of patients with congenital esotropia.
Esophoria is a condition involving inward deviation of the eye often due to extra-ocular muscle imbalance.
References:
Esophoria at near is a condition involving inward deviation of the eye when an individual is viewing an object at near.
References:
Accommodative esotropia is the most common cause of childhood esotropia. At the onset, the deviation is usually intermittent, but usually becomes constant in the following weeks to months.
Intermittent esotropia is a condition where either one or both eyes turn inward occasionally and not all the time when an individual is viewing an object at near.
References:
Accommodative esotropia is the most common cause of childhood esotropia. At the onset, the deviation is usually intermittent, but usually becomes constant in the following weeks to months.
Intermittent esotropia is a condition where either one or both eyes turn inward occasionally and not all the time when an individual is viewing an object at near.
References:
Also called anterior basement membrane dystrophy (ABMD) or map-dot-fingerprint dystrophy, epithelial basement membrane dystrophy is the most common type of corneal dystrophy. The clinical course has two phases: an early phase characterized by recurrent epithelial erosions and a second phase with visual disturbances. This occurs as a result of abnormalities in the formation and maintenance of the epithelial basement membrane adhesion complex of the corneal epithelium. Though the majority of patients remain asymptomatic or experience only minor episodic discomfort, some will complain of recurrent corneal erosions and/or visual disturbances. Management focuses on improving vision and reducing the rate of recurrence of recurrent corneal erosions with application of nighttime lubricating or hyperosmotic ointments, use of bandage soft contact lenses, or, in more severe cases (see below links), treatment with surgical interventions, such as superficial keratectomy (SK).

References:
Epstein-Barr virus, also known as human herpesvirus 4, is one of the most common viruses in humans. EBV may be suspected in cases of interstitial keratitis, iridocorneal endothelial (ICE) syndrome, among others.
Extracapsular cataract extraction is usually performed in the setting of a dense cataract that may be difficult to remove using more modern techniques, such as phacoemulsification. Althgouth there are various techniques, the videos below demonstrate the technique of creating a 12mm limbal incision with subsequent expression of the cataract using counter pressure and a muscle hook.
In some cataract extraction cases, there is a need to convert to an unplanned ECCE in the event the lens is too dense to continue phacoemulsification safely or there is concern for an impending dropped lens with continued surgery, such as with a radialized capsular tear.
Review this ECCE tutorial to better understand factors that would increase CE difficulty, indications for conversion, and the steps needed to efficiently and safely carry out this surgical technique.
References:
Endothelial keratoplasty is a partial-thickness cornea transplant technique to restore vision when the endothelium, or the inner cell layer of the cornea, is dysfunctional. This most commonly occurs in the setting of Fuchs dystrophy, bullous keratopathy, iridocorneal endothelial syndrome, or other endothelial disorders. EK selectively replaces only the endothelium and Descemet’s membrane, leaving healthy stroma and epithelium intact. The main types of EK are Descemet stripping automated endothelial keratoplasty (DSAEK), Descemet's stripping endothelial keratoplasty (DSEK) and Descemet's membrane endothelial keratoplasty (DMEK).
References:
Epidemic keratoconjunctivitis is a highly contagious viral conjunctivitis. It is caused by adenoviruses; specifically, serotypes 8, 19, and 37 are often associated with EKC (135, 136). Adenovirus most commonly manifests as a follicular conjunctivitis. When adenoviral eye infections further involve the cornea, the term epidemic keratoconjunctivitis (EKC) is used. These patients may develop pseudomembranes, subepithelial corneal infiltrates, and/or corneal erosions (137).
References:
Endolaser is an important component of vitreoretinal surgery and is commonly used to create a laser barricade around retinal tears, surround retinectomy edges or giant retinal tear margins, and delivery scatter panretinal photocoagulation (139).
References:
The external limiting membrane, also called the outer limiting membrane, is seen as a distinct, hyper-reflective line in the outer retina on optical coherence tomography (OCT). Although not a true basement membrane, the ELM is comprised of zonulae adherentes connecting the photoreceptor cell bodies (inner segments) and the apical processes supporting Müller cells (140).
Numerous retinal diseases can cause ELM disruption, including acute macular neuroretinopathy, hydroxychloroquine toxicity, macular holes, retinal detachments, among others
Electroocoulogram is an elecrophysiologic test that measures the existing resting electrical potential between the cornea and Bruch's membrane.
The defective chloride channels in Best vitelliform macular dystrophy result in an abnormal electrooculogram with a low Arden ratio (light peak/dark trough).
Extraocular muscle motility refers to examination and testing the function of the extraocular muscles. Below is an example of EOM documentation in a patient with localized orbital amyloidosis presenting as new-onset diplopia.
Electroretinography measures the electrical activity of the retina when exposed to flashes of light of varying intensity. Abnormalities in the ERG typically occur in conditions that affect the bipolar cells or the photoreceptor cells (142).
Multifocal Electroretinogram (mf-ERG) allows the detection of localized parafoveal or extramacular depression in early retinopathy, such as in hydroxychloroquine toxicity.
Ocular diseases diagnosed or serially followed with ERG include Central retinal vein occlusion, Retinitis pigmentosa, Vitamin A deficiency, among others.
Epiretinal membrane, also known as cellophane maculopathy or macular pucker, is an avascular fibrocellular membrane that clinically appears as a sheen on the inner surface of the retina. ERMs most commonly cause minimal symptoms, but in some cases, they can result in painless loss of vision and metamorphopsia. ERMs become symptomatic when affecting the macula. Pars plana vitrectomy (PPV) with membrane peel (MP) with or without internal limiting membrane (ILM) peel is the surgical treatment of choice for patients who want definitive treatment for their symptomatic ERM.
References:
An erythrocyte sedimentation rate is a type of blood test that measures how quickly erythrocytes (red blood cells) settle at the bottom of a test tube that contains a blood sample. Elevated ESR (usually greater than 20 mm/hour; the exact value is patient/age dependent) suggests there is a faster than normal rate of erythrocyte settling and may be indicative of an infection, such as orbital cellulitis, or inflammatory diseases, such as giant cell arteritis (GCA), orbital myositis, lupus, or rheumatoid arthritis (91).
Episcleral venous pressure is an important determinant of intraocular pressure (IOP) and can be measured by using various techniques, including non-invasively by estimating the pressure required to compress an episcleral vein to a predetermined endpoint (144, 145). ESVP is relatively stable but varies with alterations in body position and with certain diseases of the orbit, the head, and the neck that obstruct venous return to the heart or shunt blood from the arterial to the venous system. The usual range of ESVP is 8–10 mm Hg. Elevated ESVP may be associated with blood in Schlemm’s canal on gonioscopy.
In some ocular diseases, resistance to aqueous outflow may be due to elevated episcleral venous pressure based on the Goldmann Equation: Po=(F/C) + Pv
Ocular diseases that may have increased ESVP include Carotid cavernous fistula, Sturge-Weber syndrome, Thyroid eye disease, among others.
References:
Exam under anesthesia refers to examination of a patient while he or she is under anesthesia. Pediatric ophthalmologists often schedule EUAs for infants or children who need accurate intraocular pressure checks, retinoscopy, corneal examination, evaluation for uveitis, and/or retinal laser procedures. EUAs may also be performed for a patient who has had eye or eyelid trauma.
Children with infantile glaucoma often have serial EUAs with IOP checks, axial eye length checks, corneal diameter measurements, and evaluation for optic nerve changes. Some advantages of EUAs include the accuracy of the measurements obtained compared to a clinic setting and the ability to intervene with surgery at the time of examination.
Floaters are tiny clumps of collagen or cells inside the vitreous cavity. These specks often appear to the patient as small circles or lines when the shadow is cast on the retina. In contrast, flashes happen when there is vitreoretinal traction that leads to pulling on the retina. This traction appears as flashing lights or lightning streaks to the patient. Complaints of sudden onset of flashes or floaters should be evaluated promptly be an ophthalmologist with a dilated fundus examination (DFE) as these symptoms may be related to a posterior vitreous detachment (PVD), retinal tear, retinal detachment, and/or vitreous hemorrhage.
Review this tutorial on photopsias to learn more about the differential diagnosis and management of flashes.
Follow-up refers to further action, such as contact with a health care agency, after a hospital or clinic visit.
In ophthalmology, f/u should not be confused with 5-FU, which refers to 5-fluorouracil. 5-FU is used as an anti-fibrotic agent in the post-operative period of trabeculectomy surgeries and does increase the risk of post-operative bleb-associated endophthalmitis.
Fix and follow refers to the ability of a person to fix and follow a light or an object. This is commonly documented for pre-verbal children. Further information on vision screening for children can be found here.
Fundus autofluorescence (FAF) is a rapid non-contact, non-invasive way to evaluate retinal pigment epithelium (RPE) function (146). Autofluorescence is the intrinsic fluorescence emitted by a substance after being stimulated by excitation energy. Ocular structures that autofluorescence include the corneal epithelium and endothelium, lens, macular and RPE pigments, optic nerve drusen. The clinical use of fundus AF relies on the fact that the predominant source of autofluorescence in the macula is lipofuscin.
Abnormal fundus autofluorescence can be seen in hydroxychloroquine toxicity, macular telangiectasia, disc drusen and PXE, pattern dystrophy, and many others.
A foreign body is an object or piece of extraneous matter that has entered the body, usually as a result of trauma. A common consult for ophthalmologists is the removal of foreign bodies embedded in the cornea; see below links. Care should be taken to ensure the globe is not ruptured and/or the FB does not traverse full-thickness through the cornea.
Intraocular foreign bodies (IOFBs) are emergencies and require prompt surgical removal of the foreign body from the eye. Please see the tutorial on ocular trauma to learn more about examination and management of ocular and adnexal injuries.
References:
Familial exudative vitreoretinopathy defines a group of inherited diseases with abnormal retinal angiogenesis leading to incomplete vascularization of the peripheral retina. It can be inherited in an autosomal dominant (most common), autosomal recessive, or X-linked recessive fashion (called Norrie’s disease).
FEVR patients often develop neovascularization (NV) and develop tractional and exudative retinal detachments. Temporal dragging of the macula and vessels is commonly seen.
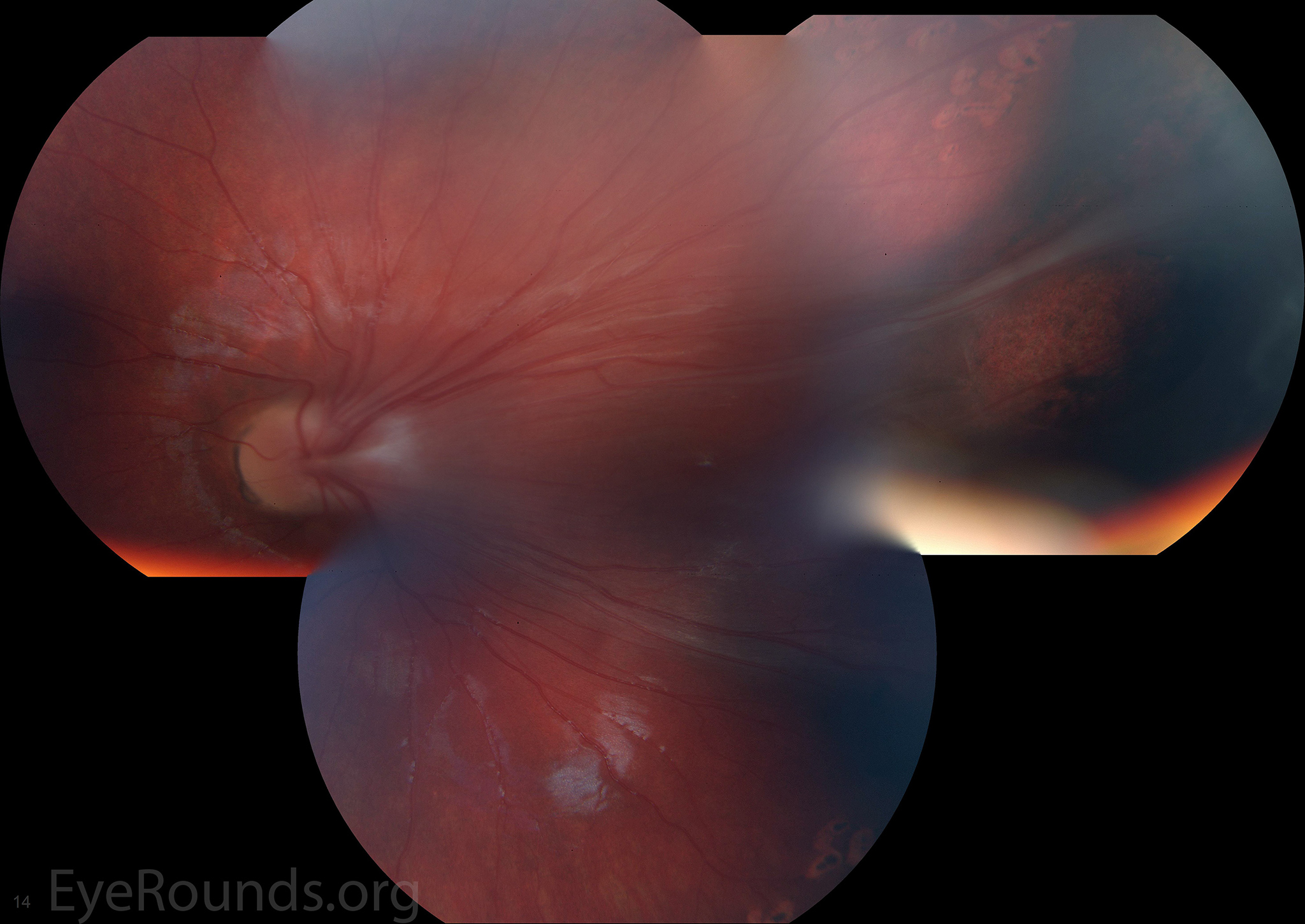
References:
Fundus fluorescein angiography is a diagnostic procedure where a fluorescein dye is injected into a vein in the arm/hand. As dye passes through the retinal vessels, multiple photographs are taken to record the blood flow throughout the retina. The photographs can reveal the presence of abnormal blood vessels or damage to the existing vessels with leakage of the dye.
FFA is an image modality commonly utilized in the diagnosis and management of diabetic retinopathy, neovascular age-related macular degeneration, anterior ischemic optic neuropathy, central serous retinopathy, central retinal vein occlusion, among others.
Review normal and abnormal FFA images here.
Family history refers to information about medical conditions of the direct blood relatives of the patient. A pedigree is an important part of the family history when an inherited eye disease is suspected or known. Review the pedigrees in the following cases: Malattia leventinese and dominant optic atrophy. In patients with retinal detachments (RDs), a strong family history of RDs would increase suspicion of Stickler’s syndrome or other inherited retinal degenerations. Similarly, a family history often helps make the diagnosis for corneal dystrophies, juvenile glaucoma, Best disease, neurofibromatosis (NF), among many others, and such knowledge further helps gauge prognosis.
Fluorescent treponemal antibody absorption test is a confirmatory test for syphilis designed to detect the presence or absence of specific antibodies directed against the spirochete bacterium Treponema pallidum.
Laboratory testing for syphilis involves two types of assays: non-treponemal and treponemal. The non-treponemal tests, such as rapid plasma regain (RPR) and Venereal Disease Research Laboratory (VDRL), are less specific, and they become negative after treatment. The treponemal tests, such as Treponema pallidum particle agglutination assay (TPPA) and FTA-ABS, are more sensitive and more specific, but they remain positive for life (148).
References:
Full-thickness macular holes are foveal defects involving full-thickness retina from the internal limiting membrane (ILM) to the outer segment of the photoreceptor layer (149).
Treatment includes pars plana vitrectomy (PPV) with epiretinal membrane (ERM) peel (MP), internal limiting membrane (ILM) peel, and gas. The patient are often required to do facedown positioning for several days to weeks to ensure adequate gas tamponade and closure of the macular hole.
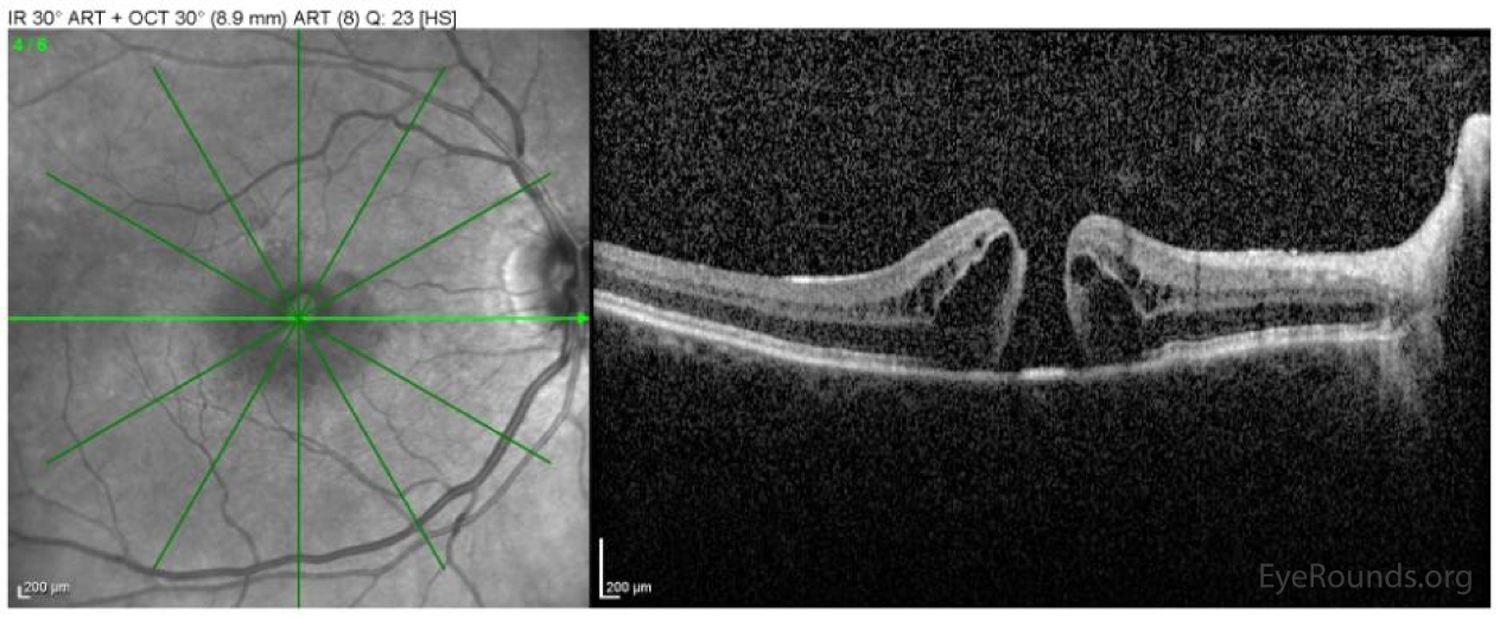
References:
Fracture is a break in bone or cartilage, usually resulting from trauma. Orbital fractures are common ophthalmic consults; please review orbital fracture repair videos here to learn more about these surgeries.
Fifteen percent of orbital floor fractures in female patients are secondary to assault, with over half of these being intimate partner violence (IPV). This IPV tutorial reviews the screening tools and intervention steps for these difficult cases.
References:
Geographic atrophy is a chronic progressive degeneration of the macula, as part of late-stage age-related macular degeneration (AMD) (150). The disease is characterized by localized sharply demarcated atrophy of outer retinal tissue, retinal pigment epithelium and choriocapillaris. It is bilateral in most cases, and starts typically in the perifoveal region and expands to involve the fovea with time, leading to central scotomas and permanent loss of visual acuity.
Giant cell arteritis, or temporal arteritis, is an inflammatory disease affecting the large blood vessels of the scalp, neck, and arms. Inflammation causes a narrowing or blockage of the blood vessels, which interrupts blood flow, and can cause arteritic anterior ischemic optic neuropathy with profound blindness in one or both eyes if untreated.
GCA is an ophthalmic emergency. Please review this GCA tutorial by Dr. Sohan Singh Hayreh to learn more about the diagnosis and management of this blinding disease. ESR and CRP are common blood tests used in the diagnosis and monitoring of this disease state. It should be noted that any patient with suspected GCA should be promptly started on high dose systemic steroids prior to obtaining a confirmatory temporal artery biopsy.
References:
The ganglion cell layer is the retinal layer containing the ganglion cell nuclei and amacrine cells. There are 1.2 million axons in the optic nerve with the cell bodies in the GCL. The synapses of these axons are in the lateral geniculate body.
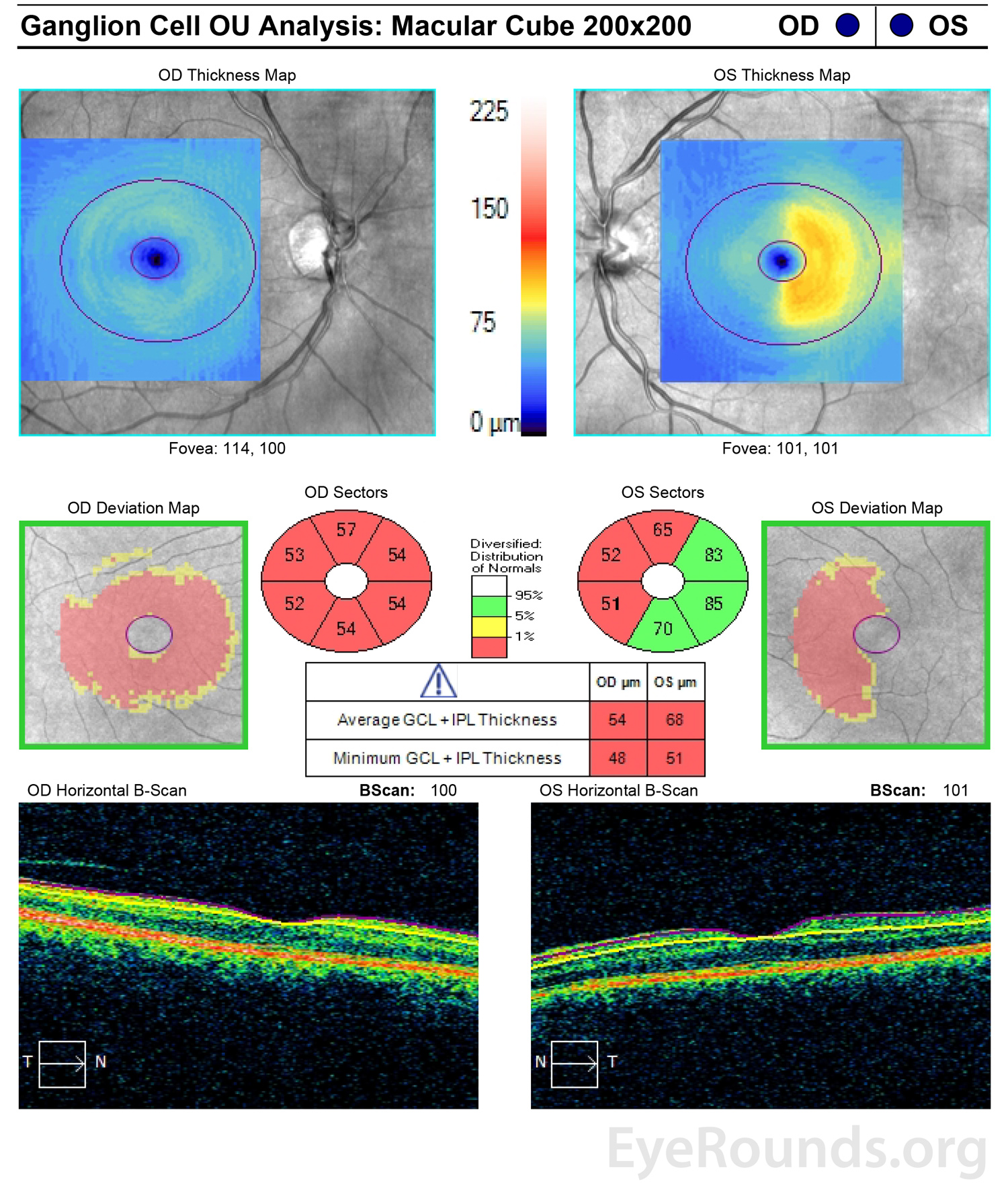
References:
Gastrointestinal refers collectively to the digestive system, including the stomach, small and large intestine, and the digestive tract.
Pseudoxanthoma elasticum (PXE) patients may also have gastrointestinal findings. Gardner’s syndrome, which is associated with colon cancer, presents with bilateral “bear tracks” of congenital hypertrophy of the retinal pigmented epithelium (CHRPE) lesions. Behcet’s disease causes recurrent ocular inflammation and often is associated with genital and oral aphthosis.
Gonioscopy is an examination technique used to evaluate the internal drainage system (anterior chamber angle) of the eye and to determine whether the angle is open or closed, which has implications for intraocular pressure (IOP) and glaucoma diagnosis.
Gonioscopy.org includes numerous examples of gonioscopy performed on patients with various glaucoma diagnoses.
There are several gonioscopy-assisted surgeries performed to lower IOP; these include gonioscopy-assisted transluminal trabeculotomy (GATT) and other minimally invasive glaucoma surgeries (MIGS)
References:
Giant papillary conjunctivitis is a condition when the palpebral conjunctiva becomes hyperemic, swollen, and irritated with large papillae, usually due to long-term contact lens or prosthetic use (153).
References:
A drop (Gtt) is a unit of volume approximated by the amount of fluid dispensed from a dropper or drip chamber.
Goldmann visual field is a type of kinetic visual field test in which progressively dimmer lights of varying sizes against a white background are moved from the peripheral vision into the central vision. The point at which the target is first seen within bowl-shaped perimeter is accurately mapped, often by a perimetrist who is monitoring the patient’s eyes and responses.
References:
Graft-versus-host disease is a life-threatening complication of allogeneic stem cell transplantation and develops when a donor transplant's immune cells attack the recipient's tissues. GVHD symptoms include skin rash, nausea, vomiting, diarrhea, abdominal cramping, dryness, and irritation of the eyes. Ocular involvement occurs in 90% of all GVHD cases.
Please review this chronic ocular GVHD case to better understand the pathophysiology, ophthalmic symptoms, testing, and management of these difficult cases.
Hand motions refers to one’s ability to see hand movement. Notation demonstrates the distance from which the patient can detct motion of the examiner’s hand. For example, “HM 4” indicates the patient’s ability to see motion on the examiner’s hand at four feet.
Human papillomavirus is the most common sexually transmitted infection. It can lead to cancer or genital warts.
There is a strong association of conjunctival papilloma with HPV, most notably strains 6 and 11 (low-risk) and 16 and 33 (high-risk). Treatment consists of surgical excision with free margins, followed by cryotherapy (155).
References:
Hemiretinal vein occlusion is an occlusion at the disc, involving either the superior or inferior hemiretina.
This branch retinal vein occlusion case and central retinal vein occlusion tutorial have detailed information on the pathophysiology, diagnosis, testing, and management of RVOs.
Horseshoe tears, also referred to as flap or U-shaped tears, are full thickness breaks in the retina that occur secondary to vitreous traction to an area of preexisting vitreoretinal adhesion (156). The retina frequently appears completely normal before the acute event. Horseshoe tears are more common in middle age and appear most often near the equator of the eye. It is important to perform scleral depression on any patient with acute onset of flashes and/or floaters if a retinal tear is suspected. Treatment includes laser retinopexy using photocoagulation to barricade the retina surrounding the tear. Failure to identify or treat retinal breaks can put the patient at risk of developing a rhegmatogenous retinal detachment (RRD).
This branch retinal vein occlusion case and central retinal vein occlusion tutorial have detailed information on the pathophysiology, diagnosis, testing, and management of RVOs.
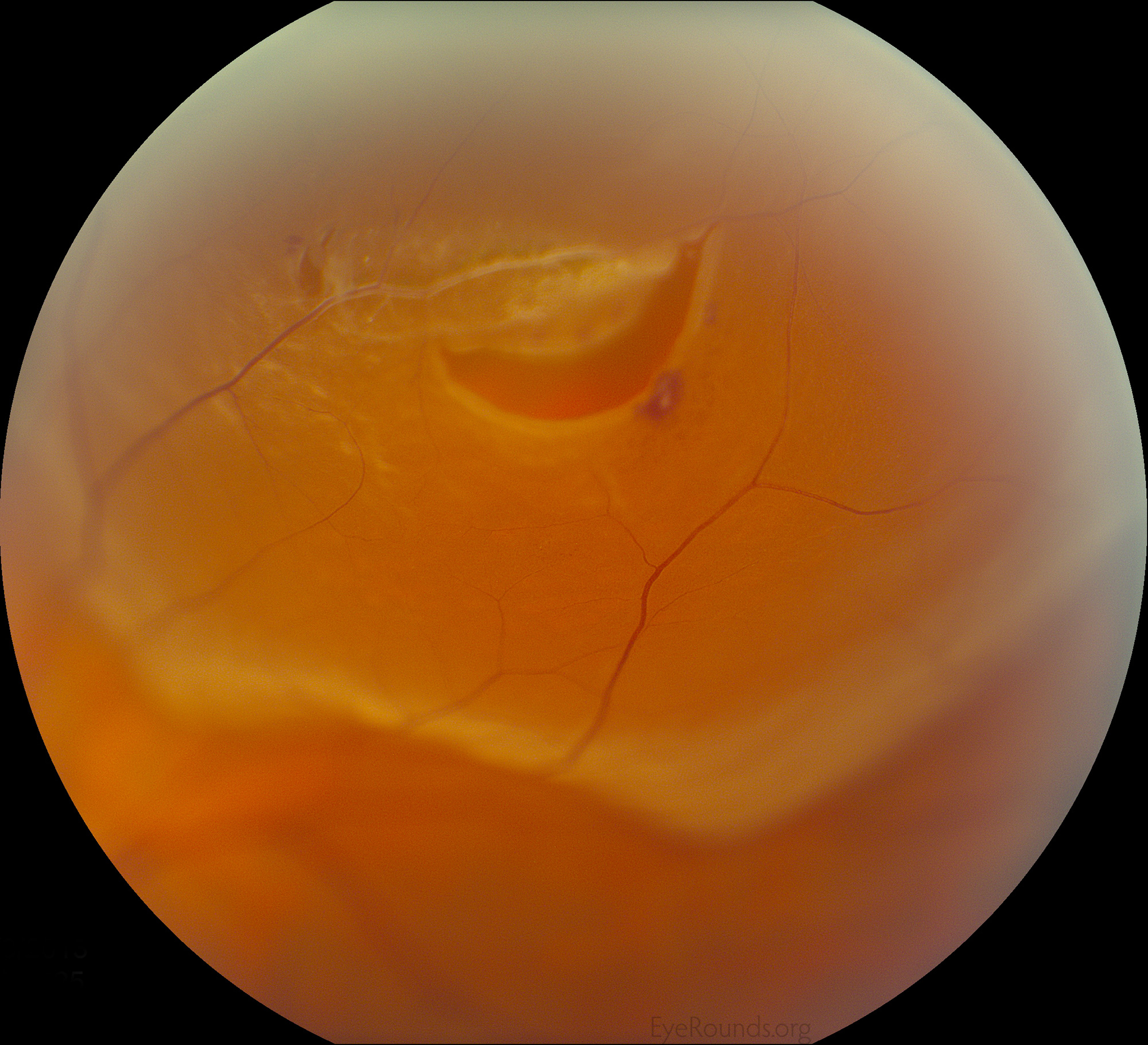
References:
The herpes simplex virus is an infection that can cause recurrent infection of the skin, mouth, lips, eyes, and genitals. Ocular HSV can present as HSV keratitis with classic epithelial dendrites, HSV stromal or disciform keratitis forms, or HSV keratouveitis with elevated intraocular pressure, anterior chamber (AC) cell, and keratic precipitates (KP). Herpetic ocular disease may cause neurotrophic keratopathy, which predisposes the patient to superinfections.
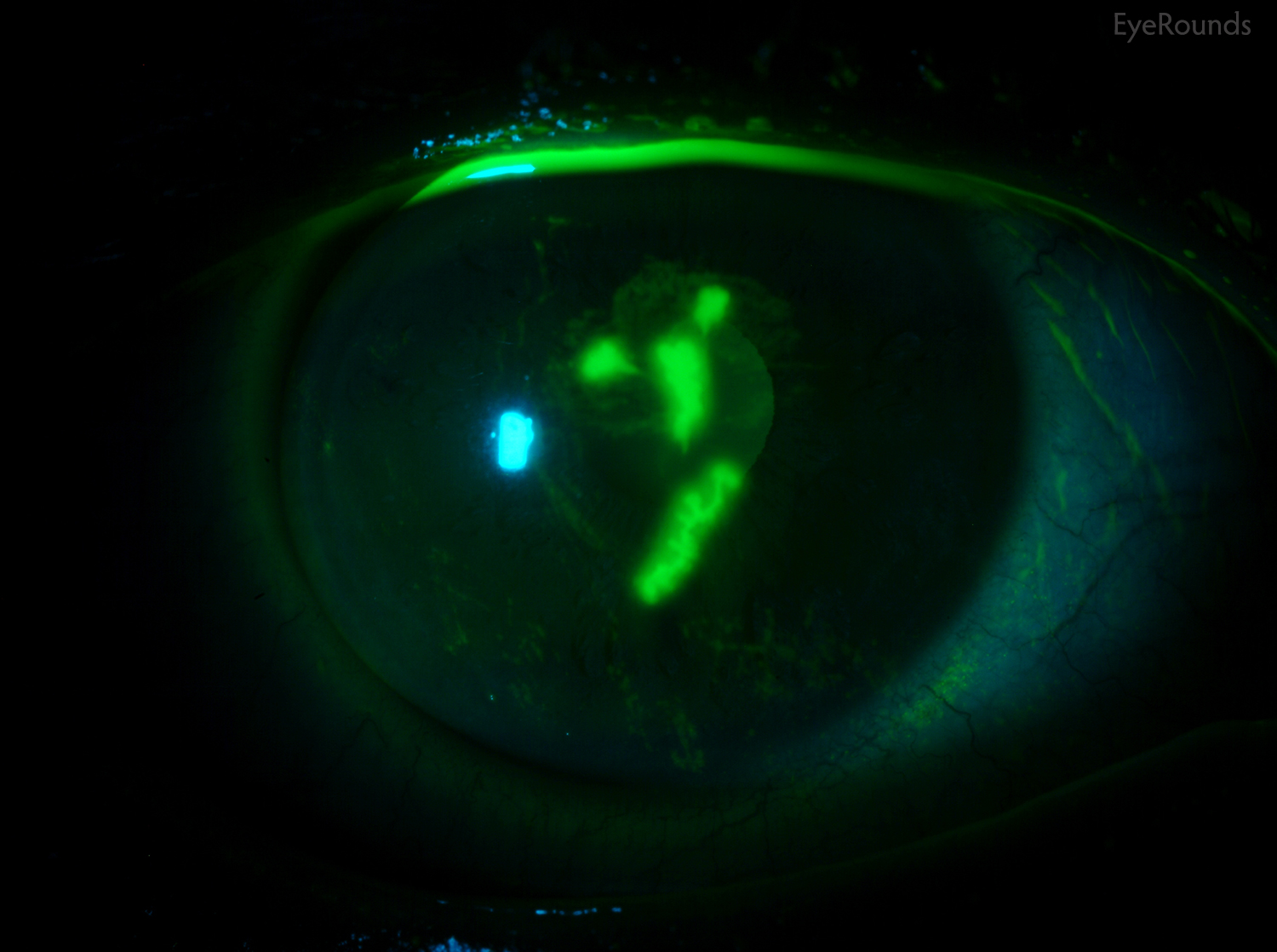
References:
Hypertropia is a condition of misalignment of the eyes where the visual axis of one eye is higher than the fellow fixating eye.
References:
Humphrey visual field testing is an automated, static perimetry tool for measuring the visual field. During HVF testing, the patient fixes his gaze toward a central fixation point. The HVF test assesses the ability to see a non-mobile stimulus which remains for a brief moment (around 200 ms) in the visual field. Different locations within a given region of the visual field are tested until the threshold, or the stimulus intensity seen 50% of the time, is seen at each test location (159).
HVF is commonly used in the glaucoma clinic to assess glaucomatous progression. The following Iowa Glaucoma Curriculum Videos are helpful to better understand HVF principles and interpretations:
References:
Hypotropia is a condition of misalignment of the eyes where the visual axis of one eye is lower than the fellow fixating eye.
References:
Herpes zoster ophthalmicus is a condition that usually manifests as a unilateral, painful skin rash in a dermatomal distribution of the trigeminal nerve shared by the eye and ocular adnexa (160, 161). HZO occurs typically in older adults but can present at any age and occurs after reactivation of latent varicella-zoster virus (VZV) present within the sensory spinal or cerebral ganglia.

References:
Intracapsular cataract extraction involves the removal of the lens and the surrounding lens capsule through one large limbal incision (162). The major drawbacks of ICCE include potentially blinding complications, such as retinal detachment, macular edema, and corneal decompensation, which are more likely to occur when the lens capsule is not in place to prevent the vitreous from prolapsing forward. Further, there is no capsular support for a posterior chamber intraocular lens (IOL), and anterior chamber IOLs are commonly used instead.
ICCE requires larger incisions to remove a cataract, leading to slow healing and a greater amount of surgically induced astigmatism. Despite its drawbacks, ICCE remained the primary approach for cataract extraction in the United States well into the 1970s, and modern ICCE is still in practice in developing countries.
References:
Indocyanine green angiography is a procedure used to acquire an angiogram of the choroid (163). ICG is similar to fluorescein angiography, but instead uses Indocyanine green dye, which fluoresces in the infra-red, non-visible light range. The infra-red wavelenths can penetrate the retinal layers making the circulation in deeper layers visible when photographed with an infra-red sensitive camera. ICG is injected intravenously and flows through the body to reach the choroidal and retinal circulation.
ICG allows the distinct outlines of the vessels of the choroid to be seen and identified. ICG is sometimes used to complement fundus fluorescein angiography (FFA). FFA is often referred to retinal angiography while ICG angiography is referred to choroidal angiography.
Polypoidal choroidal vasculopathy (PCV) can be diagnosed with ICG angiography by detection of choroidal polyps.
Diluted ICG dye is also commonly implemented surgically for identification of the internal limiting membrane prior to peeling this layer; this staining technique is often used for macular hole repairs.
Infectious crystalline keratopathy was first described as a unique and distinctive clinical entity characterized by white, branching, crystalline, opacities within the corneal stroma and little or no associated inflammatory response (164). A sharply demarcated, snowflake-like stromal opacity on a background of clear corneal graft is the classic presentation. ICK is most commonly associated with Streptococcus species (specifically α-hemolytic Streptococcus), but may be caused by a variety of organisms.
The most common risk factors for infectious crystalline keratopathy include history of penetrating keratoplasty, corticosteroid use, and contact lens wear.
Treatment initially consists of cessation or strict minimization of topical steroids and prolonged use of topical bactericidal antibiotics. ICK is difficult to treat, demonstrating poor and slow response to medications. Debilitating stromal scars or recurrence of infection are common.
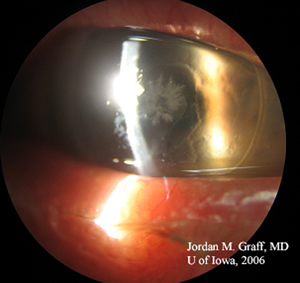
References:
Idiopathic intracranial hypertension is a condition in which the cerebrospinal fluid (CSF) is under high pressure in the absence of an intracranial mass, venous sinus thrombosis, or other primary cause (165). It is also known as pseudotumor cerebri because patients present with signs and symptoms of a brain tumor without a brain tumor being present. Patients may complain of headaches, double vision, pulse-synchronous tinnitus (PSTs), transient visual obscurations (TVOs). The below IIH case describes the differential diagnosis, work-up, and treatment options (165).
Please note that one of the main treatments for IIH is weight reduction. This tutorial is helpful as an overview of weight management in IIH.
References:
Interstitial keratitis is a chronic, non-ulcerative inflammation of the corneal stroma that may be seen in isolation or may be associated with uveitis or episcleritis (166). Symptoms include pain, tearing, photophobia, and/or gradual blurring of vision. The differential diagnosis for IK includes infections, such as syphilis, tuberculosis, mumps, Lyme disease, Chlamydia, leprosy, brucellosis, Epstein-Barr virus, Rubeola, parasitic infection, or herpes zoster and simplex. Interstitial keratitis may rarely be seen in association with systemic and autoimmune diseases, such as associated granulomatous vasculitis, polyarteritis nodosa, rheumatoid arthritis, relapsing polychondritis, lymphoma, sarcoidosis, and Cogan’s syndrome.
References:
The internal limiting membrane is the basal lamina of the inner retina that is formed by the footplates of Müller cells. It is the structural interface between the retina and the vitreous and is composed of collagen fibers, glycosaminoglycans, laminin, and fibronectin.
Patients with an epiretinal membrane and/or macular hole may undergo pars plana vitrectomy with ILM peeling. ICG or brilliant blue are dyes used in these cases to staining the ILM. However, ILM peeling has been rarely associated with ganglion cell layer loss and dissociation of the nerve fiber layer.
References:
The inner nuclear layer consists of the cell bodies of horizontal cells, bipolar cells, amacrine cells, interplexiform neurons, Müller cells, and sometimes displaced ganglion cells (168). The nuclei of the horizontal cells are located next to the outer plexiform layer, where their processes synapse. The nuclei of the amacrine cells are located next to the inner plexiform layer, where their processes terminate.
Paracentral Acute Middle Maculopathy is a disease state sometimes seen in isolation or with vein or artery occlusions. In these cases, the patients present with paracentral scotoma due to occlusion of the superficial plexus and resultant ischemia of the INL.
References:
The inferior oblique is one of the six extra-ocular muscles that control eye movements. The inferior oblique moves the eye up and out. Although rare, IO palsy may lead to diplopia with an elevation deficit. In cases of fourth nerve palsy, there is often an IO overaction (IOOA). Weakening of the IO muscle by recession or myectomy are commonly performed for superior oblique palsy cases associated with a V-pattern strabismus.
References:
Intraocular foreign bodies are seen in 18%-40% of penetrating ocular injuries that most frequently occur at workplaces where tools involving metal striking metals are used (169).
IOFBs are emergencies and require prompt surgical removal of the foreign body from the eye. Please see the tutorial on ocular trauma to learn more about examination and management of ocular and adnexal injuries.
References:
Intraocular lens is a lens implanted in the eye as part of a treatment for cataracts or myopia. The most common type of IOL is the pseudophakic IOL which is implanted immediately after cataract extraction.
There are numerous videos here to review the surgical steps of cataract extraction with intraocular lens placement (CEIOL). A thorough “time out” should be performed accurately to ensure safety of every IOL placement surgery and to minimize wrong site or wrong implant mistakes.
IOLs can also be placed in the anterior chamber (ACIOL); additionally, IOLs can be sutured or externalized through the sclera when there is no capsular support.
References:
In primary inferior oblique muscle overaction, an upshoot of the adducting eye occurs when gaze is directed into the field of action of the inferior oblique muscle, producing a greater upward excursion of the adducted eye than of the abducted eye (170).
In cases of fourth nerve palsy, there is often an IO overaction. Weakening of the IO muscle by recession or myectomy are commonly performed for superior oblique palsy cases associated with a V-pattern strabismus.
References:
Intraocular pressure is the pressure in mmHg (mm of Mercury) inside the eye measured by tonometry.
The Iowa Glaucoma Curriculum is a resource for learning more about glaucoma, including how to measure IOP, the classifications of glaucoma, and numerous videos on the medical and surgical management of elevated or low IOP.
Pupillary Distance (PD) or interpupillary distance (IPD) is the distance, often measured in millimeters, between the centers of the pupils of each eye. This measurement is used when preparing to make prescription eyeglasses.
Convergence (in prism diopters) is defined as 100/working distance (cm) x Pupillary Distance (cm). Further description can be found in this optics review.
References:
The inner plexiform layer consists of synaptic connections between the axons of bipolar cells and dendrites of ganglion cells.
The inferior rectus is one of the six extra-ocular muscles that controls eye movements. The IR moves the eye down and in.
Thyroid eye disease (TED) is the most common cause of proptosis in adults. The muscle most commonly enlarged in TED is the inferior rectus, followed by the medial rectus. It can contribute to vision loss by causing a compressive optic neuropathy.
Orbital floor fractures are common consults for ophthalmologists, and entrapment of the inferior rectus muscle should be ruled out both clinically and radiologically. Muscle entrapment should be promptly addressed surgically to avoid compartment syndrome around the muscle.
Intraretinal microvascular abnormalities are shunt vessels that appear as abnormal branching or dilation of existing blood vessels within the retina. These vessels act to supply areas of non-perfusion in diabetic retinopathy (171). These vessels represent either new vessel growth within the retina or remodeling of pre-existing vessels through endothelial cell proliferation stimulated by hypoxia bordering areas of capillary non-perfusion.
IRMA is one of the defining features of severe non-proliferative diabetic retinopathy (NPDR) based on the "4-2-1" criteria from the Early Treatment Diabetic Retinopathy Study (ETDRS). Please review the below diabetic retinopathy tutorial to better understand this classification system.
IRMAs are slightly larger in caliber than neovascularization (NV) with broader arrangement and are always contained to the intraretinal layers. Neovascularization will show late leakage on fluorescein angiography whereas IRMAs traditionally do not leak.
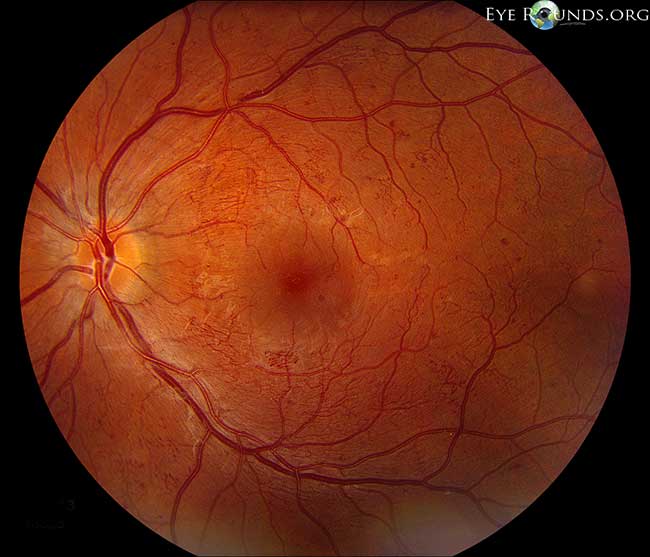
References:
Intravitreal triesence is injected into the eye in a similar fashion to anti-VEGF agents. Triesence contains preservative-free triamcinolone acetonide, a corticosteroid, and is often given in pseudophakic patients with chronic macular edema, such as in diabetic retinopathy or vein occlusions, after failing monthly anti-VEGF agents. IVT is also used with patients with ocular inflammatory conditions unresponsive to topical corticosteroid agents.
As when other intraocular steroid injections, IVT should not be given to patients with glaucoma or a history of elevated intraocular pressures. The dose for intraocular use varies; however, 2 mg (or 0.05cc) and 4 mg ( or 0.10cc) are commonly used, studied, and well tolerated.
References:
Jaeger notation for near vision assigns each line on the near vision card a single arbitrary numeric value corresponding to a Snellen value. For example, Jaeger 2, abbreviated J2, is equivalent to the 20/30 Snellen distance-equivalent line. The near card should be read with correction and at a normal reading distance, approximately 14 inches from the eyes.
References:
Juvenile open-angle glaucoma is a subset of primary open-angle glaucoma (POAG) (173). The two conditions are classified by age, with JOAG affecting those who are between three and 40 years old and adult-onset POAG affecting those older than 40 years. JOAG is a rare condition and is estimated to affect 1 in 50,000 individuals. JOAG is frequently passed down through families, and many cases of JOAG are caused by mutations in the myocilin gene, especially subjects that have early-onset of disease, high IOP, and a strong family history of glaucoma (174).

References:
Juvenile idiopathic arthritis is the most common type of arthritis in children under the age of 16 (176). JIA can cause persistent joint pain, swelling, and stiffness. Some children may experience symptoms for only a few months, while others have symptoms for the rest of their lives. JIA can cause complications including growth problems, joint damage, and uveitis.
Uveitis associated with JIA is most commonly seen in patients with the oligoarticular type (i.e., 2-4 joints are involved). Additional risk factors, screening recommendations, and management can be reviewed in the discussion of the below JIA case.
References:
Juvenile xanthogranuloma is a benign and typically self-limited skin disorder that is not commonly associated with systemic manifestations. The skin lesions of JXG usually present as reddened, yellowish-tan, slightly raised bumps.
Juxtafoveal telangiectasia, now called macular telangiectasia (or mac tel), is a condition that leads to abnormalities of capillaries of the fovea or perifoveal region associated with loss of the outer nuclear layers and ellipsoid zone. This ocular disease can progress to cystic cavitation-like changes in all retinal layers or development of full-thickness macular hole or subretinal neovascularization in advanced stages (179, 180).
Learn about the diagnosis and management of the three types of macular telangiectasia by reading this case.
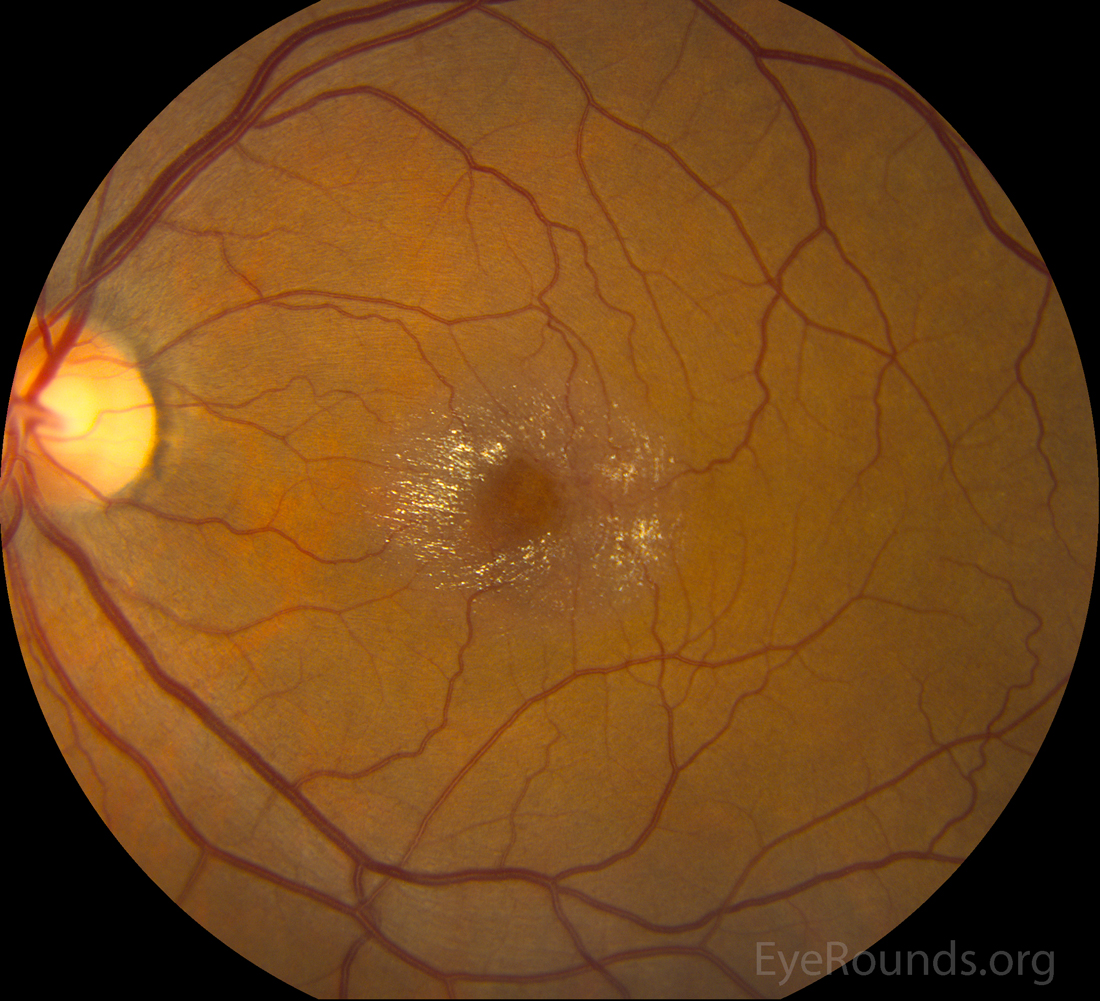
References:
The cornea is the clear, multilayered structure that is serves as the front part of the eye. It serves as a barrier and focuses light. Corneal procedures can be reviewed here. Corneal imaging can be reviewed here.
References:
Keratoconus is a progressive eye disease in which the cornea thins and begins to bulge into a cone-like shape. This causes light to be deflected as it enters the eye and leads to distorted vision (183).
Keratoconus, the most common corneal ectasia, is a progressive corneal condition characterized by central thinning and steepening of the cornea. Early keratoconus often looks normal on slit lamp examination. Topography has become the gold standard for screening patients for keratoconus and other corneal ectasias. Review the corneal imaging tutorial for excellent KCN examples.
Surgical management of KCN can be reviewed here.
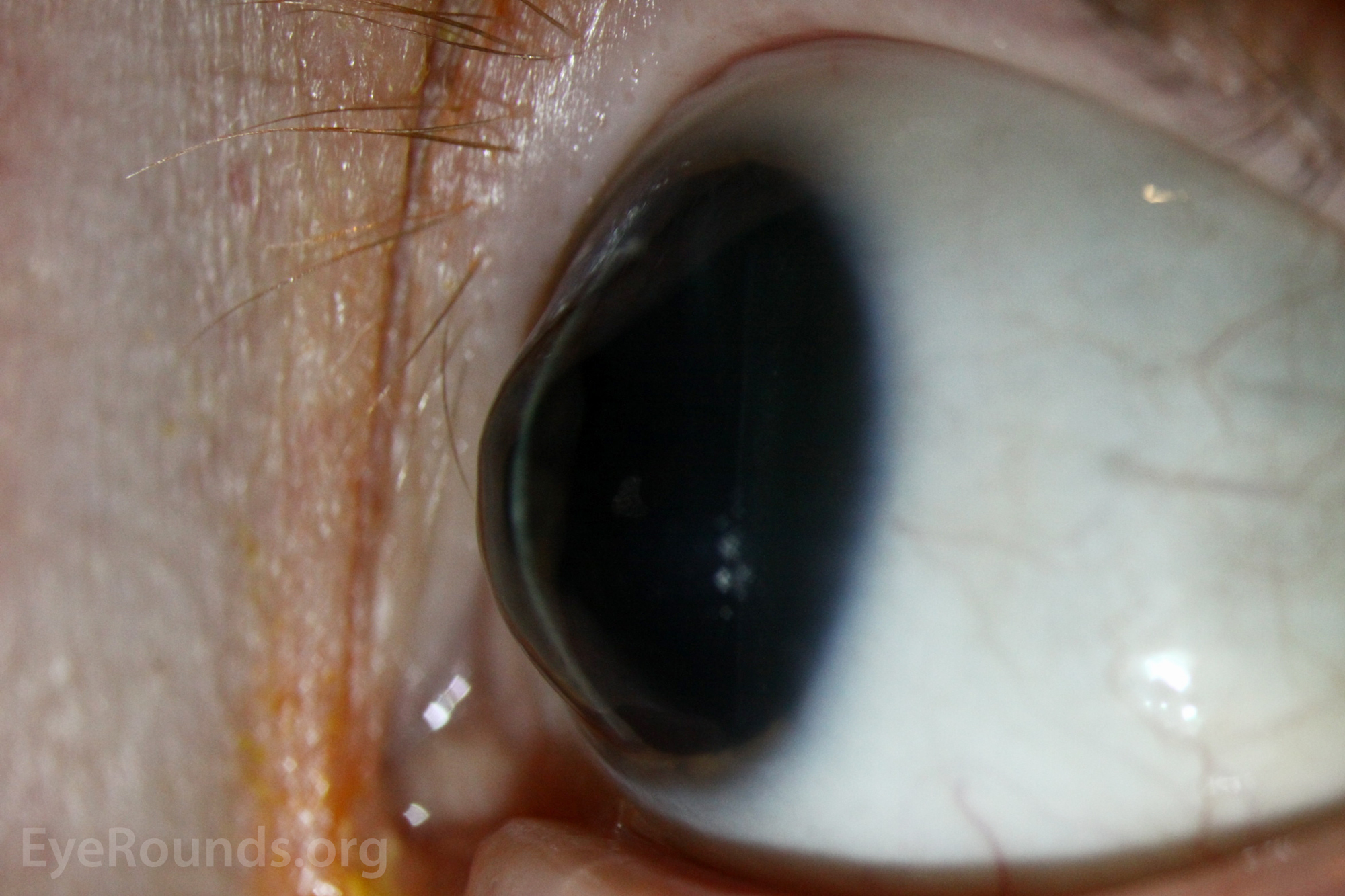
References:
Keratoconjunctivitis sicca, or dry eye syndrome, is a condition where A) the aqueous component of tears is inadequate; B) there is excessive tear evaporation; or C) there is a combination of A and B. DES is often due to meibomian gland dysfunction and associated blepharitis.
Please review this comprehensive evaporative dry eye tutorial to learn more about dry eye diagnosis and management.
References:
Keratic precipitates are inflammatory cellular deposits seen on corneal endothelium. When these coalesce and become large with a yellowish color, they are described as mutton-fat KP, which are associated with granulomatous inflammation (e.g., sarcoidosis, VKH, TB, syphilis, etc.). Non-granulomatous ocular inflammations (e.g., HLA-B27-associated uveitis) may present with fine KP.
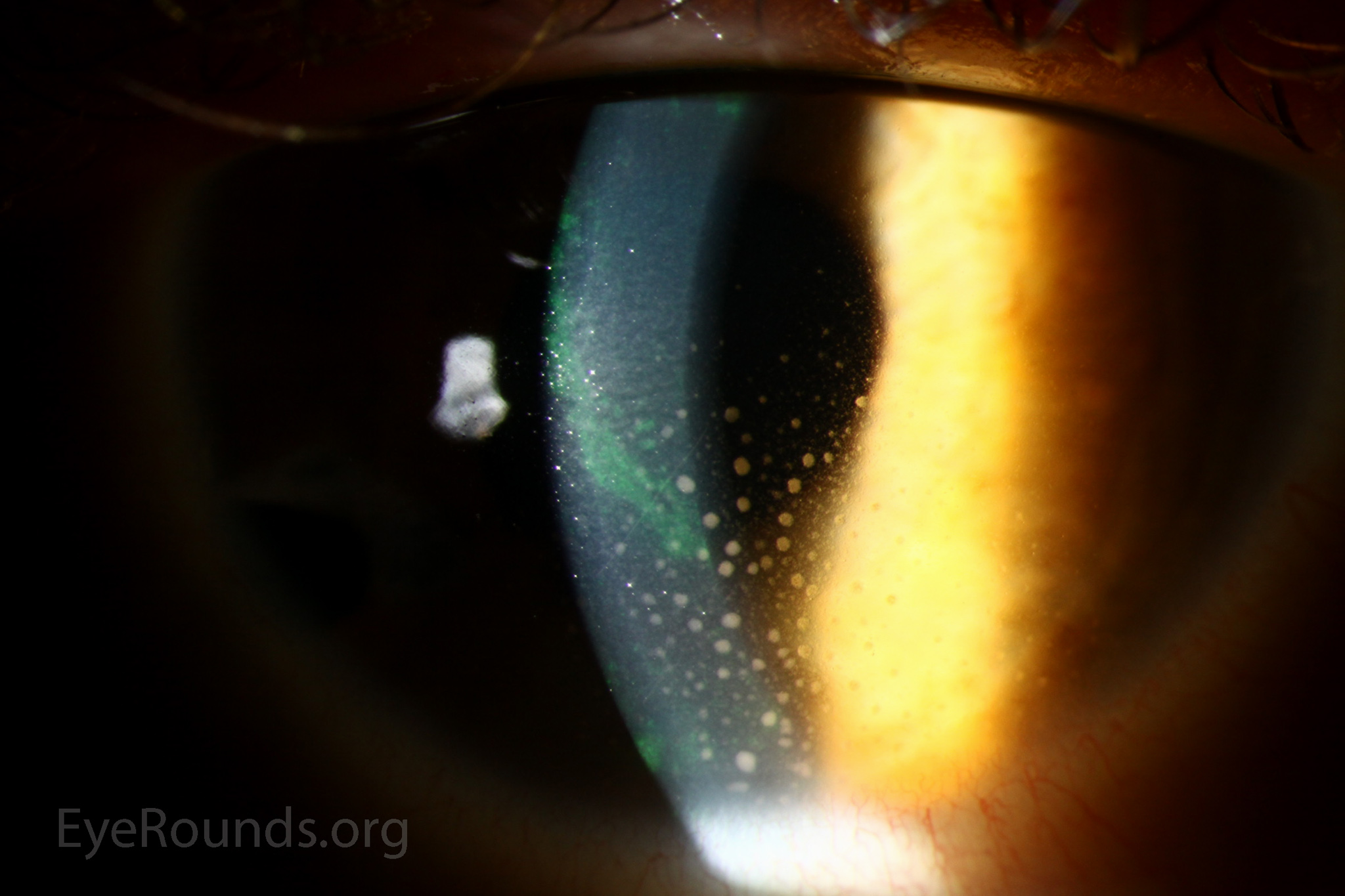
References:
Keratoprosthesis (KPro) implantation is a procedure that involves full-thickness removal of the cornea and replacement by an artificial cornea. The keratoprosthesis is then secured to host tissue using interrupted or running sutures (110).
Review this KPro tutorial with images and videos relevant to this keratoprosthesis.
Krukenberg spindle refers to pigment along the corneal endothelium. This is a common sign in pigmentary dispersion syndrome due to circulating pigment in the anterior chamber. Pigment dispersion occurs due to rubbing of the iris pigment epithelium against the lens zonules, typically because of a back-bowed iris. This pigment can clog the trabecular meshwork and lead to pigmentary glaucoma.
References:
Lids and lashes refer to eyelids and eyelashes. Lids and lashes should be examined at every slit lamp examination.
Please see the oculoplastics surgery page for numerous videos related to procedures on lids and lashes.
Associated pathology: Floppy eyelid syndrome, distichiasis, benign lesions, blepharitis, meibomian gland dysfunction
A laceration is a deep cut or tear through the skin that creates a wound, usually requiring a procedure for closure. In ophthalmology, eyelid lacerations are common consults. When the laceration is close to the lid margin medial to the puncta of the eyelids, the canaliculus likely has been injured and requires surgical repair. Dog bites are common causes of eyelid trauma.
Please review this tutorial on emergent evaluation of eyelid lacerations.
References:
Laser-assisted subepithelial keratectomy (LASEK) is a procedure used for correction of a broad range of refractive abnormalities. Like Laser in situ keratomileusis (LASIK), LASEK create flaps preceding the laser treatment of corneal stromal tissue. The flap in LASEK is more superficial (i.e., only epithelium) compared to that of LASIK. LASEK is considered a surface ablation procedure, much like photorefractive keratectomy (PRK). LASEK was developed as an alternative to PRK to address the issue of pain associated with epithelial debridement used for PRK (187).
LASEK instruments can be reviewed here.
Laser in situ keratomileusis (LASIK) is a procedure used for correction of a broad range of refractive abnormalities. The safety and efficacy of the procedure, combined with the quick visual recovery and minimal patient discomfort, have made LASIK the most popular refractive procedure for the treatment of all, but the highest levels, of myopia, hyperopia, and astigmatism.
This tutorial provides a good summary of laser refractive surgery.
Pre-op assessment should be carefully performed to rule out underlying corneal dystrophy, keratoconus, autoimmune disorders, history of herpetic eye disease, among others.
LASIK complications include post-LASIK ectasia, epithelial ingrowth, dislocation of flap, and diffuse lamellar keratitis
Leber congenital amaurosis is a family of congenital retinal dystrophies that results in severe vision loss at an early age (188). Patients present usually with nystagmus, sluggish or near-absent pupillary responses, severely decreased visual acuity, photophobia and high hyperopia. It is the most severe retinal dystrophy, causing blindness by the age of 1 year. Although RPE65 mutations account for only 8% of all LCA cases, the first FDA approved gene therapy, Voretigene Neparvovec-rzyl (Luxturna), was developed for RPE65-associated LCA (189).
References:
The muscles responsible for eyelid retraction are the levator palpebrae superioris, Müller's muscle, and the frontalis muscle. Of these three, the levator muscle is the predominant muscle of eyelid retraction.
Levator function is the distance the upper eyelid travels from downgaze to upgaze while the frontalis muscle is held inactive at the brow. A LF measurement of 13 - 17 mm is considered normal.
Other pre-op testing techniques and etiologies for ptosis can be reviewed in this tutorial: A primer on ptosis.
Lid hygiene refers to promoting and maintaining the health of the eyelids and ocular surface. Poor lid hygiene can lead to blepharitis, meibomian gland dysfunction, and chalazion formation.
Associated pathology: Blepharitis, meibomian gland dysfunction, ocular rosacea, chalazion
Leber hereditary optic neuropathy is the most common inherited mitochondrial disorder (190). It typically begins as a unilateral progressive optic neuropathy, with sequential involvement of the fellow eye months to years later. Treatment options are limited but include the use of antioxidant supplements, including idebenone, and gene therapy trials are currently underway. Please see below LHON case for overview of differential diagnosis and management.
References:
Laser indirect ophthalmoscopy is a tool that enables ophthalmologists to treat retinal pathology while the patient is in a supine position. This allows the physician to perform maneuvers, such as scleral depression, which allows visualization of peripheral lesions that would be otherwise hidden from the field of view using slit lamp biomicroscopy.
Other advantages of LIO include a wider field of view, better image resolution, and less irritation to the ocular surface. It is also useful in patients with small pupils and decreased media clarity.
LIO is performed in progressing retinopathy of prematurity (ROP) cases to ablate the peripheral non-perfused retina. This technique is also commonly utilized to laser around retinal tears or localized retinal detachments. It can also be used to perform panretinal photocoagulation (PRP) in the setting of proliferative diabetic retinopathy (DR).
Lamellar keratoplasty is a surgical procedure for removal of only the damaged or diseased epithelium and stroma, leaving the endothelium intact, in cases where only the more superficial layers are damaged. Examples include deep anterior lamellar keratoplasty (DALK).
A trephine with an appropriate diameter is used to make a partial-thickness incision into the patient’s cornea, followed by pneumodissection or manual dissection of the anterior stroma. The dissection step is followed by placement of a graft prepared from a full-thickness punch in which the donor endothelium-Descemet membrane complex has been removed. The graft is secured with interrupted and/or running sutures, and these are then selectively removed post-operatively.
DALK is useful for processes involving the corneal stroma in the presence of healthy endothelium. Examples of ocular disease states that may require DALK include corneal ectasia, corneal scars that are not full-thickness, and corneal stromal dystrophies.
LLL refers to the lower eyelid of the left eye.
Review the difference between festoons and lower eyelid dermatochalasis here.
Light perception refers to the ability to detect the presence of a direct light source (on or off). Light perception with projection indicates the patient sees where the light is coming from. In contrast, bare light perception (BLP) is a term used to describe severe visual impairment in which the patient is only capable of perceiving diffuse, indirect light.
Laser peripheral iridotomy is a procedure to treat angle-closure glaucoma caused by relative or absolute pupillary block. LPI eliminates pupillary block by allowing the aqueous fluid to pass directly from the posterior chamber into the anterior chamber, bypassing the pupil. Review the Iowa glaucoma curriculum here to learn more about LPI technique and indications.
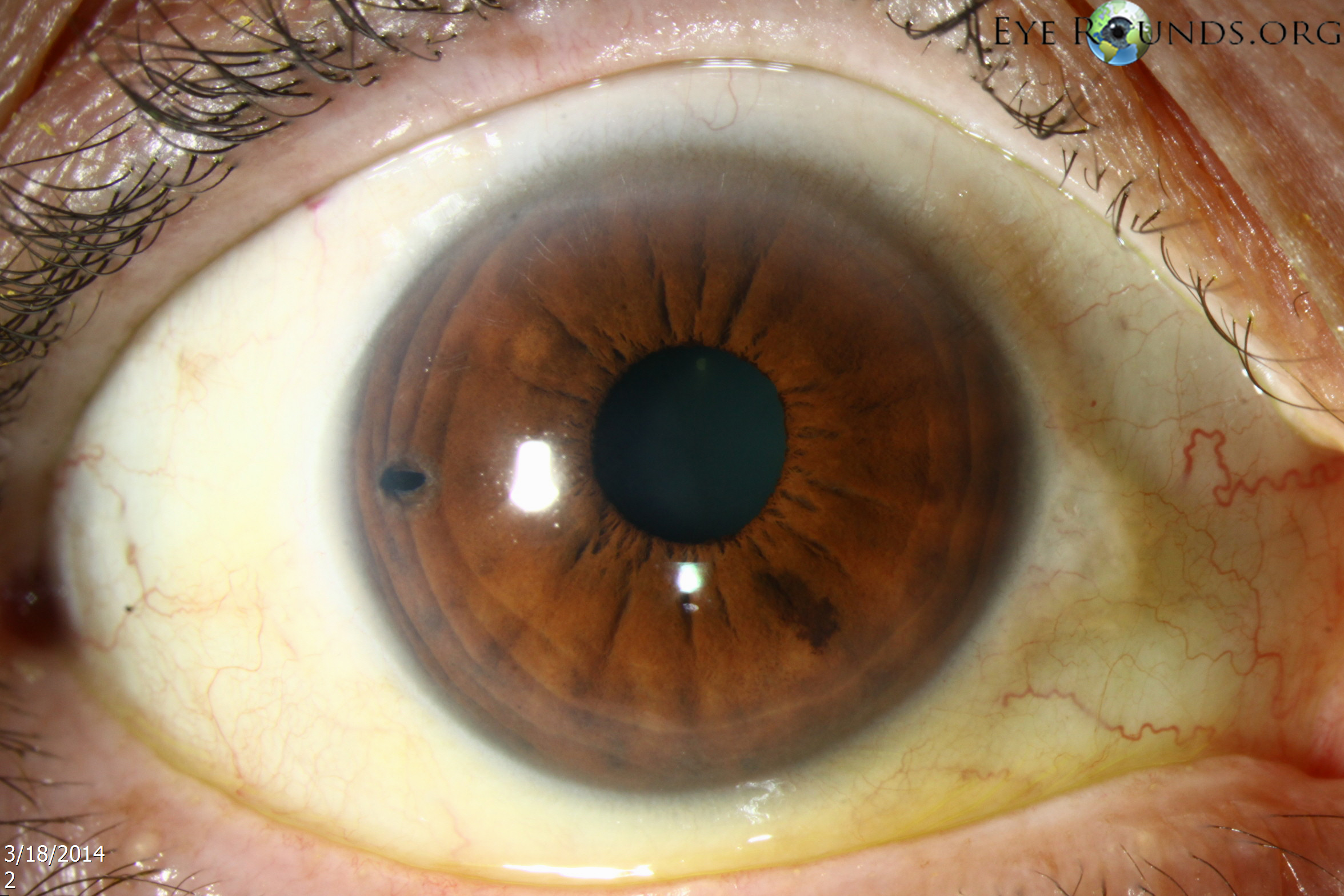
References:
The lateral rectus is one of the six extraocular muscles that control the movements of the eye. The LR muscle is responsible for lateral movement of the eyeball (i.e., abduction) and is controlled by cranial nerve VI. Sixth nerve palsies lead to loss of abduction with resultant binocular, horizontal diplopia; there are multiple etiologies, including compression, microvascular/infarction, or infiltration.
In sagging eye syndrome, there is often subacute-onset, acquired, esotropia resulting from involutional changes in the extraocular muscles and inferomedial displacement of the lateral rectus muscle belly.
References:
Limbal relaxing incision is a partial thickness corneal incision placed to reduce or eliminate pre-existing astigmatism during cataract surgery or refractive lens exchange surgery. LRIs alter the corneal curvature by flattening the cornea in the meridian in which they are placed and steepening the cornea 90 degrees away.
This tutorial on astigmatism management reviews the options for astigmatic management around the time of cataract surgery, including the advantages and disadvantages of LRI procedures.
Limbal relaxing incision is a partial thickness corneal incision placed to reduce or eliminate pre-existing astigmatism during cataract surgery or refractive lens exchange surgery. LRIs alter the corneal curvature by flattening the cornea in the meridian in which they are placed and steepening the cornea 90 degrees away.
This tutorial on astigmatism management reviews the options for astigmatic management around the time of cataract surgery, including the advantages and disadvantages of LRI procedures.
LUL refers to the upper eyelid of the left eye. The oculoplastics surgery techniques page has numerous videos on upper eyelid procedures, including biopsy, eyelid lesion removal, chalazion drainage, ptosis repair, blepharoplasty, tarsorrhaphy, and repair of upper eyelid entropion or retraction.
Microaneurysm is an dilation of the venous end of a retinal capillary primarily associated with diabetic retinopathy (DR). When MAs are present in the perifoveal region associated leakage can result in clinically significant macular edema. Focal laser directly to microaneurysms can be performed to close these vascular abnormalities and decrease the retinal edema present (192).
References:
Melanoma-associated retinopathy is a paraneoplastic condition that causes visual symptoms of scotomas, night-blindness, and photopsias (193). Like cancer-associated retinopathy (CAR), MAR is rare autoimmune disease where the body develops autoantibodies to retinal antigens, in particular retinal bipolar cells. Optical coherence tomography (OCT) may show increased reflectivity of outer retina and/or retinal pigment epithelium (RPE), among other findings. Electroretinography is helpful as there is commonly retinal dysfunction with electronegative waveforms, specifically a markedly attenuated b-wave. Early fundus examination is often normal, but vessel attenuation, nerve pallor, and retinal atrophy are late findings (194).
Also called anterior basement membrane dystrophy (ABMD) or epithelial basement membrane dystrophy (EBMD), MDF is the most common type of corneal dystrophy. The clinical course has two phases: an early phase characterized by recurrent epithelial erosions and a second phase with visual disturbances. This occurs as a result of abnormalities in the formation and maintenance of the epithelial basement membrane adhesion complex of the corneal epithelium (195). Though the majority of patients remain asymptomatic or experience only minor episodic discomfort, some will complain of recurrent corneal erosions and/or visual disturbances. Management focuses on improving vision and reducing the rate of recurrence of recurrent corneal erosions with application of nighttime lubricating or hyperosmotic ointments, use of bandage soft contact lenses, or, in more severe cases (see below links), treatment with surgical interventions, such as superficial keratectomy (SK).

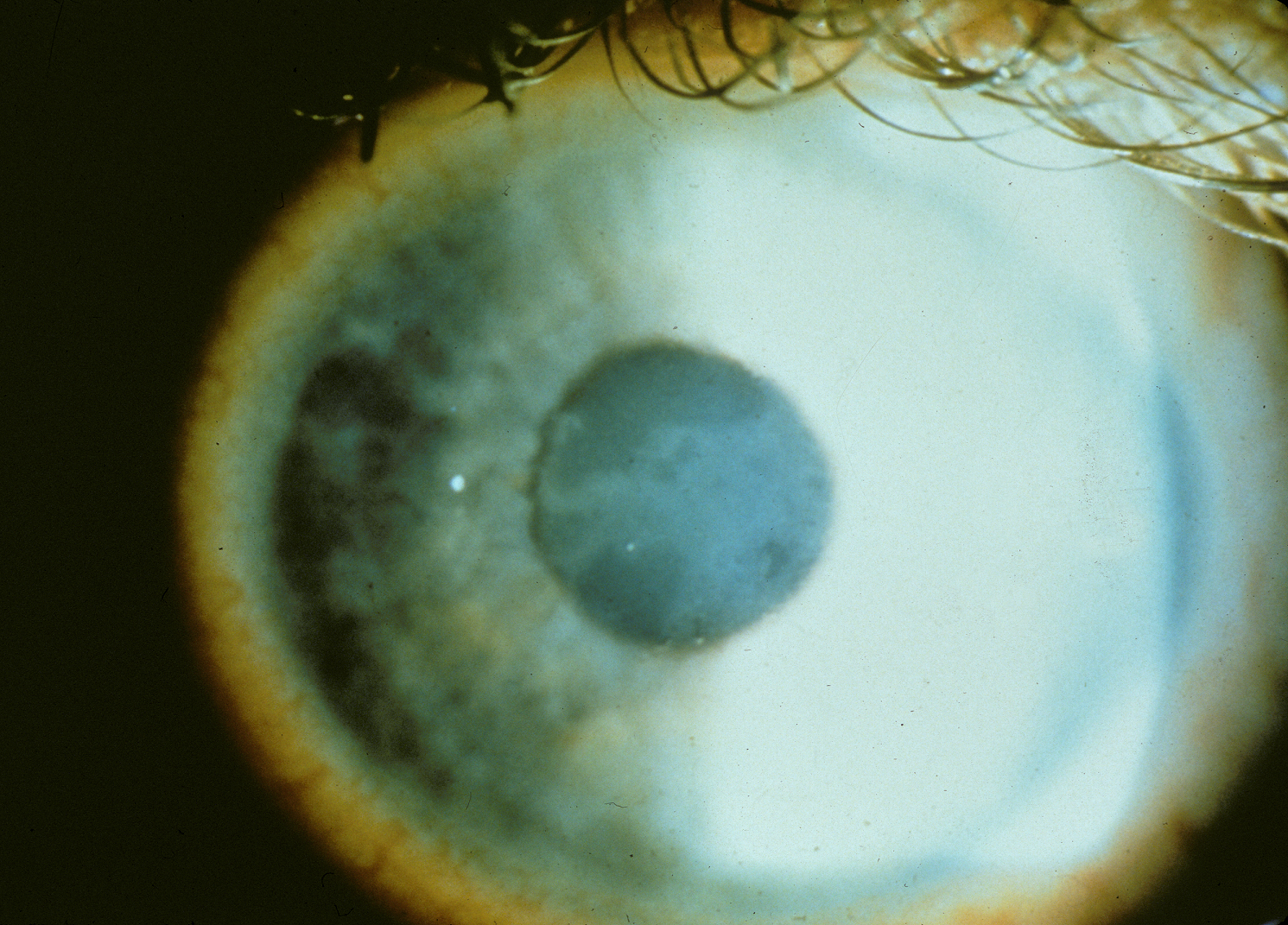
References:
Multiple evanescent white dot syndrome is an inflammatory retinal disorder, typically observed in young myopic patients (women more than men), that is characterized by unilateral vision loss and the presence of small, punctate, grey-white lesions that involve the outer retina and retinal pigment epithelium (197). This is often self-limiting, and prognosis is excellent.
Classically, fundus fluorescein angiography (FFA) shows early punctate hyperfluorescence with late staining of the lesions arranged in a wreath-like" configuration around the fovea.
References:
Myasthenia gravis is a chronic autoimmune neuromuscular disease affecting postsynaptic acetylcholine receptors (199). MG, although a systemic disease that may affect breathing and cause profound arm/leg weakness, may present with only ocular symptoms 50% of the time. Patients often present complaining of binocular diplopia, and the ocular motility deficits may mimic other neurologic disorders, such as 6th nerve palsy, 4th nerve palsy, internuclear ophthalmoplegia, etc. The hallmark signs of MG include fluctuation & fatigability, diplopia, ophthalmoplegia, ptosis, weakness of jaw, weak neck/trunk/limbs, dysphagia, hoarseness, dysarthria, and dyspnea.
Chest imaging is warranted in confirmed cases as thymomas are commonly associated with MG. Review the below case to learn more about MG diagnosis, including utility of anti-Ach recetor antibody testing, Tensilon testing, and ice/rest testing.
References:
Meibomian gland dysfunction is a condition where blockage or some other abnormality of the meibomian glands causes them to not secrete enough oil into the tears. As a result, the tears then evaporate too quickly.
Dry eye syndrome is often due to meibomian gland dysfunction and associated blepharitis.
Please review this comprehensive evaporative dry eye tutorial to learn more about dry eye diagnosis and management.
Malignant Melanoma is a form of cancer that arises when melanocytes, pigment-producing cells, mutate and become cancerous. MM can affect the eye (200).
Please read about the Collaborative Ocular Melanoma Study (COMS).
References:
Müller muscle conjunctival resection is a posterior eyelid ptosis repair technique that spares the tarsus (201). MMCR remains an effective tool for the repair of small amounts of blepharoptosis and gives more predictable results compared to levator procedures. It is cosmetically appealing as it is a posterior ptosis repair with the incision being through the conjunctiva and not through skin, leaving no visible scar behind.
References:
A membrane peel is a type of procedure in which the contracting membranes on the retinal surface are carefully stripped away. This procedure is commonly performed for progressing epiretinal membranes (ERMs) affecting the central macula or macular holes. Further, tractional membranes can develop in proliferative diabetic retinopathy (PDR) and proliferative vitreoretinopathy (PVR).
Improved visualization of these membranes is sometimes achieved with dilute indocyanine green (ICG), brilliant blue, and/or dilute Kenalog.
References:
The medial rectus is one of the six extra-ocular muscles that adducts the eyes. It is innervated by the inferior division of cranial nerve III, thus third nerve palsies often lead to a “down and out” eye with limited adduction due to unopposed action of the lateral rectus and superior oblique muscles.
References:
Margin to reflex distance 1 (MRD1) is the distance from the margin of the upper lid to the central corneal reflex (normal is 4.0-5.0 mm). The distance from the pupillary light reflex to the lower eyelid margin is the MRD2, which is normally ~5mm.
MRD1 + MRD2 = palpebral fissure height
Review this Primer on Ptosis to better understand the various examinations performed for ptosis evaluation, the etiologies of ptosis; and the most common ptosis repair procedures.
Manifest refraction refers to the use of trial lenses with or without a phoropter using a standard visual acuity protocol to obtain the refractive error for a patient and the best corrected visual acuity. This is performed as a monocular test with occlusion of the fellow eye during testing.
References:
Multiple sclerosis is a demyelinating disease in which the myelin of nerve cells in the brain and spinal cord are damaged. This process can lead to problems in vision (e.g., optic neuritis), balance, muscle control, autonomic function, and other symptoms.
Classic white matter lesions in MS can be seen here. Please review this tutorial and this case to better understand the signs and symptoms, pathophysiology, management of optic neuritis, which is the presenting symptom in 15-20% of cases of MS.
Motor vehicle accident refers to a collision where a motor vehicle strikes or collides another vehicle, object, etc.

References:
Non-arteritic anterior ischemic optic neuropathy refers to loss of perfusion and/or oxygenation of the optic nerve that typically causes sudden vision loss in one eye without any pain (203). In most cases, NAION presents with significant loss of vision in one eye immediately upon waking up in the morning. The visual loss typically remains stable, without getting markedly better or worse once it has occurred.
Patients should be screened for hypertension, obstructive sleep apnea, diabetes mellitus, anemia, nocturnal hypotension (using hypertension medications late at night), and/or migraines as these are associated with an increased risk of NAION. Small cup to disc ratio and elevated intraocular pressure can also increase the risk. Risk factor management is key as the fellow eye is at risk of NAION, especially if the optic nerves both have small cups.
Giant cell arteritis, which causes arteritic AION, should be considered and ruled out, when warranted.

References:
Non-accidental trauma refers to abuse or maltreatment (often of a child by an adult) and is a leading cause of childhood traumatic injury and death.
The differential diagnosis for retinal hemorrhages in an infant includes non-accidental trauma, sepsis, coagulopathy, leukemia, uncontrolled hypertension, cardiopulmonary resuscitation, and hyperviscosity syndromes, amongst others (205). It is prudent to rule out other causes by history, physical exam, and laboratory testing.
The primary mechanism of RHs in child abuse is mechanical with resultant shearing and damage to the retinal blood vessels, with or without direct blunt injury to the child. It is known that a correlation exists between the severity of ocular and intracranial injury and the presence of numerous retinal hemorrhages.
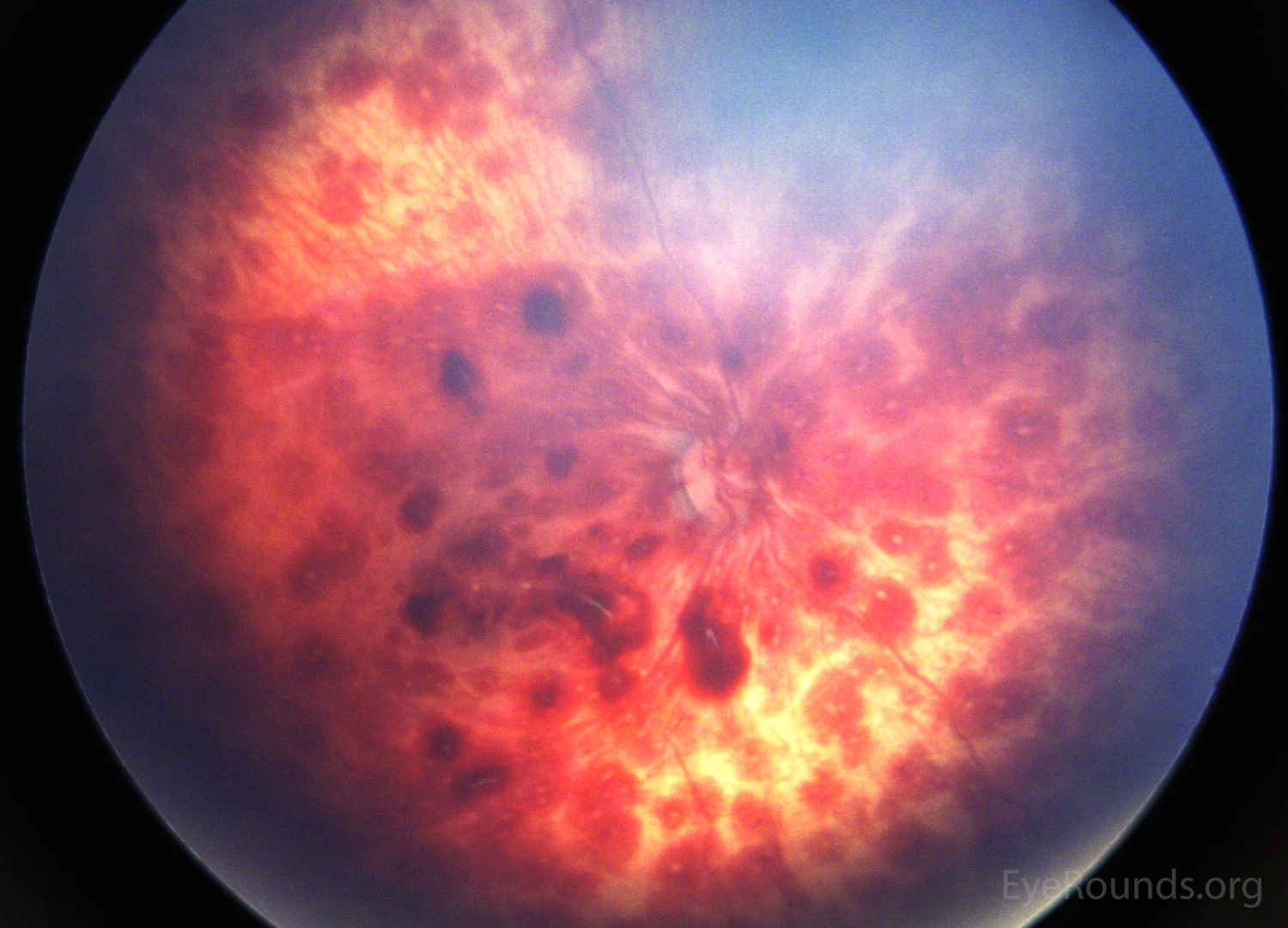
References:
North Carolina macular dystrophy is an autosomal dominant condition resulting in congenital, stationary macular abnormalities. Mild disease can present with central macular yellow-white drusen-like lesions at the level of the retinal pigmented epithelium (RPE). More severely affected individuals can exhibit severe macular dystrophy, often surrounded by a characteristic white ring of exposed sclera (207).

References:
Neurofibromatosis type 1 is a condition characterized by changes in skin pigmentation and the growth of tumors along nerves in the skin, brain, among others (208). Beginning in early childhood, almost all people with neurofibromatosis type 1 have multiple café-au-lait spots. Most adults with NF1 develop neurofibromas, benign tumors that are usually located on or just under the skin.
During childhood, benign hamartomas called Lisch nodules often appear on the iris. Some affected individuals also develop optic nerve gliomas. These tumors may lead to reduced vision or total vision loss. In some cases, optic gliomas have no effect on vision and can be monitored with serial head imaging.
Clinical diagnosis of NF1 requires 2 or more of the following (See NF1 case):
References:
Neurofibromatosis type II is a disorder characterized by the growth of non-cancerous tumors in the nervous system. The most common tumors associated with neurofibromatosis type 2 are called vestibular schwannomas or acoustic neuromas (209).
The signs and symptoms of neurofibromatosis type 2 usually appear during adolescence or in a person's early twenties. The most frequent early symptoms of vestibular schwannomas are hearing loss, tinnitus, and problems with balance (209).
References:
No improvement indicates there is no noticed improvement in the patient’s overall condition. This is often used to note that there has been no improvement in the visual acuity with the use of pinhole testing.
No known drug allergies means that as far as the patient and the provider knows, the patient is not allergic to any medications.
Nasolacrimal duct obstruction is the obstruction of the nasolacrimal duct and may be either congenital or acquired.
Dacryocystorhinostomy is a procedure for nasolacrimal duct obstruction (NLDO) that creates an anastomosis between the lacrimal sac and the nasal mucosa via a bony ostium in the nose (112, 113).
Review this case of sarcoidosis causing NLDO for an overview of the many diagnoses that can lead to acquired NLDO.
References:
No light perception refers to total blindness and the complete lack of light perception and form perception.
Near point convergence is a measurement of how close one can bring a fixation target to the nose while maintaining fusion. The examiner slowly moves the target closer to the nose until the patient reports diplopia or ocular divergence is noted by the examiner. Normal NPC varies slightly from patient to patient, but is usually less than 10 cm from the nose.
A near point of convergence of greater than 10 cm is a common finding in convergence insufficiency.
Non-proliferative diabetic retinopathy is a class of diabetic retinopathy characterized by no neovascularization. NPDR is a pathological condition associated with the initial stages of diabetic retinopathy. Hyperglycemia may result in damage to retinal capillaries, causing retinal changes, including microaneurysms, “dot-blot” hemorrhages (DBH), cotton wool spots (CWS, infarctions of the nerve fiber layer), and venous beading and dilation. NPDR may progress to proliferative diabetic retinopathy (PDR), characterized by the formation of new and abnormal blood vessels (46).
Review the following tutorial to learn about the classification of NPDR, including the 4-2-1 rule for severe NPDR, screening recommendations, treatment options, and further resources.

References:
Nothing by mouth is a medical instruction meaning to withhold food and fluids. Common instructions for surgery are to remain NPO after midnight on the night prior to surgery.
Non-reactive can refer to an examination finding, such as the pupils being non-reactive, or this can be a laboratory result indicating a negative finding. For example, this may indicate that the syphilis test was negative (non-reactive).
Near refraction refers to a refraction test done at near as part of an eye examination.
References:
Nuclear sclerosis refers to cloudiness, hardening, and/or yellowing of the central region of the lens, which is called the nucleus. As nuclear sclerosis progresses, the patient may have worsening vision, decreased color contrast sensitivity, and increased glare and haloes. A discussion of nuclear cataract stages can be found here.
Cataract surgery for Greenhorns provides an overview of cataract surgery steps. Information for patients can be found here.
References:
Normal tension glaucoma is a form of glaucoma characterized by open angles, glaucomatous optic discs, progressive visual field changes, and thinning of the retinal nerve fiber layer in individuals with intraocular pressures consistently lower than 21 mmHg (210, 211). There are several NTG risk factors, including noctornal hypotension, anemia, and obstructive sleep apnea, that should be addressed in these patients. Non-glaucomatous optic neuropathies, such as optic nerve compression from mass effect, should be considered, especially in cases of unilateral, progressive disease.
Management of NTG is similar to primary open angle glaucoma (POAG); topical medical therapy and glaucoma surgery can be reviewed at the Iowa Glaucoma Curriculum.
References:
Neovascularization is the formation and presence of new blood vessels, usually in the form of functional microvascular networks, that form collateral circulation in response to local poor perfusion or ischemia. Angiogenic factors, such as vascular endothelial growth factor (VEGF), stimulate growth of these new retinal blood vessels. Common disease states associated with NV include diabetic retinopathy, retinal vein occlusions (especially ischemic), and ocular ischemic syndrome (OIS).
The presence of NV is the determining factor of whether a patient with diabetic retinopathy has non-proliferative (no NV) or proliferative (NV present) diabetic retinopathy. Careful evaluation of the iris, angle, nerve, and retina should be common practice for all diabetics as early intervention in PDR can help prevent devastating complications, such as dense vitreous hemorrhages, tractional retinal detachments, and/or neovascular glaucoma.
This case on neovascular glaucoma in the setting of a central retinal vein occlusion provides an overview of NV-related exam findings and complications, including histological evaluation post-enucleation.
References:
NVA refers to neovascularization (see NV) of the iridocorneal angle. This is performed with gonioscopy; a representative gonioscopy video of NVA can be see here at gonioscopy.org. In advanced cases, NVA can close the angle and lead to secondary angle closure glaucoma. Such progression may require a glaucoma drainage device (e.g., Ahmed tube) or a cyclodestructive procedure.
NVD to neovascularization (see NV) of the optic disc. Proliferative diabetic retinopathy is deemed high risk when more than one-third of the optic nerve has NVD; there is any NVD with vitreous hemorrhage; or there is NV elsewhere (NVE) greater than ½ disc area in presence of vitreous hemorrhage. In these cases, 360 degrees of panretinal photocoagulation should be performed with or without adjuvant intravitreal anti-VEGF injections to prevent severe vision loss.
References:
NVE refers to the presence of neovascularization (see NV) of the retina. Proliferative diabetic retinopathy is deemed high risk when more than one-third of the optic nerve has neovascularization of the disc (NVD); there is any NVD with vitreous hemorrhage; or there is NVE greater than ½ disc area in presence of vitreous hemorrhage. In these cases, 360 degrees of panretinal photocoagulation should be performed with or without adjuvant intravitreal anti-VEGF injections to prevent severe vision loss.
References:
Neovascularization of the iris, also known as rubeosis iridis, is when small fine, blood vessels develop on the anterior surface of the iris in response to retinal ischemia. These changes most often develop at the pupillary border.
Angiogenic factors, such as vascular endothelial growth factor (VEGF), stimulate growth of these new retinal blood vessels. Common disease states associated with NV include diabetic retinopathy, retinal vein occlusions (especially ischemic), and ocular ischemic syndrome (OIS).
The presence of NV is the determining factor of whether a patient with diabetic retinopathy has non-proliferative (no NV) or proliferative (NV present) diabetic retinopathy. Careful evaluation of the iris, angle, nerve, and retina should be common practice for all diabetics as early intervention in PDR can help prevent devastating complications, such as dense vitreous hemorrhages, tractional retinal detachments, and/or neovascular glaucoma.
References:
Ocular cicatricial pemphigoid is a subtype of mucous membrane pemphigoid (MMP). OCP is a type of chronic, autoimmune process that leads to scarring of the conjunctiva, and, if untreated, it can lead to blindness due to severe ulceration and membrane formation (212). This is diagnosed with a tissue biopsy given the classic staining with IgG, IgA, IgM, and C3 in a linear pattern in the basement membrane zone of the conjunctival epithelium.
Please review this case on OCP, which discusses pathophysiology, pathology, and management of these difficult cases. Systemic symptoms of MMP, including mucous membrane lesions and ulcerations, should be asked about in all OCP cases.
References:
Optical coherence tomography is a non-contact imaging test that uses low-coherence light (near infrared spectrum; long wavelengths) to capture cross-sectional images of the retina, optic nerve, or anterior segment (AS-OCT). In OCT, a light source emits a beam of light, which strikes the tissues then reflects back to a detector. The echo time delay of the backscattering of light is measured against light traveling a reference path with a known time delay. This technique is known as low-coherence interferometry.
An easy tool to utilize in clinic, OCT is safe to use for serial examinations. High resolution images allow detection of fluid within or under the retina; disruption of retinal layers; thinning of the nerve fiber layer; visualization of the anterior chamber anatomy (angle, lens placement, etc.); among many other pathologic findings. This technology provides clinicians an in situ detailed image of parts of the eye that would previously have only been visualized via histological analysis.
OCT-A is built on the same principles as optical coherence tomography (see OCT), with only slight modification in the process. OCTA still uses the echo time delay of the backscattering of light measured against a reference beam to generate an image. The modification is that multiple sequential images are generated through exactly the same cross-section of the tissue. This technology provides a non-invasive method for visualizing choroidal and retinal vascular plexi on a level of detail not previously available in vivo.
Oculus dexter (OD) refers to the right eye.
Ocular hypertension is when the intraocular pressure (see IOP) is higher than 21mmHg. Ocular hypertension is a risk factor for developing glaucoma. Review the Iowa Glaucoma Curriculum to learn more about ocular hypertension and glaucoma suspects.
The average IOP is 15.5mmHg with 21mmHg being the cutoff for normal (two standard deviations above average). The ocular hypertension treatment study (OHTS) showed that controls (not treated) progress to glaucoma more than patients who were treated. However, 90% of patients with ocular hypertension did not progress to glaucoma. This study also demonstrated that central corneal thickness (CCT) is associated with higher IOP readings. Thus, clinicians should weigh the risk and benefits of starting medical therapy for OHT. There is a risk calculator through Washington University in St. Louis available to help make these decisions.
Ocular ischemic syndrome is a rare but vision-threatening condition associated with severe carotid artery occlusive disease leading to ocular hypoperfusion (213). Principal symptoms include visual loss and/or ocular pain. Clinically these patients present with neovascularization (see NV), retinal hemorrhages, iris atrophy, retinal artery attenuation, and venous dilation. OIS commonly occurs in the elderly with men more affected than women, owing to the higher incidence of atherosclerosis and carotid artery disease in these patients. OIS has important systemic implications, as disease of the common or internal carotid arteries may cause ipsilateral ocular signs and symptoms that in turn could herald a cerebral infarction.
The optic nerve is the second cranial nerve and transmits visual information from the retina to the brain. The optic nerve should be examined closely for signs of glaucoma (thinning of the nerve fiber layer and optic nerve rim), optic nerve edema or pallor (secondary to ischemic optic neuropathy, compression, IIH, inflammation, granuloma, etc.), abnormal perfusion or blood vessel formation (see NVD), optic nerve drusen, optic nerve hypoplasia, among other nerve abnormalities.
The Optic Neuritis Treatment Trial (ONTT) established guidelines for examination and evaluation of patients with optic neuritis, firmly establishing magnetic resonance imaging (MRI) as the procedure of choice for determining relative risk and possible therapy for multiple sclerosis and highlighting the possible importance of treatment and further clinical trial investigation on the clinical course of early MS (214). This study group found that patients with no brain lesions on MRI had a 25% risk of progression to multiple sclerosis within 15 years compared to a 72% risk of progression in patients with at least one demyelinating lesion seen on MRI (214).
Review the diagnosis and treatment of optic neuritis at the below case.
References:
The outer plexiform layer is a retinal layer that consists of a network of synapses between dendrites of horizontal and bipolar cells and photoreceptor axons. The photoreceptor cone and rod axons are also referred to as Henle’s layer;
Acute macular neuroretinopathy (AMN) lesions often occur between the outer nuclear and outer plexiform layers and frequently involve the inner segment/outer segment junction and interdigitation zone.
Oculopharyngeal muscular dystrophy is a late-onset autosomal dominant inherited disease of skeletal muscles. It is associated with progressive blepharoptosis, dysphagia, and ophthalmoplegia. Other voluntary muscles may become affected over time, including the proximal muscles of the lower limbs. Symptom onset is typically in the fifth and sixth decades of life.

References:
Over-refraction is the technique of determine the additional correction needed (i.e., residual refractive error present) while the patient is wearing corrective lenses (either glasses or contact lenses). This technique allows the examiner to determine if a refractive change is necessary.
Ocular surface squamous neoplasia is an umbrella term that encompasses dysplastic lesions involving the squamous epithelium of the conjunctiva or cornea. OSSN includes squamous papilloma, conjunctival-cornea intraepithelial neoplasia (CIN), carcinoma in situ (CIS), and invasive squamous cell carcinoma (SCC). The clinical presentation of OSSN varies across a wide spectrum and is classified by the degree of epithelial and stromal (substantia propria) infiltration. The epithelial infiltration can range from mild to severe dysplasia (i.e. mild, moderate, or severe CIN) to full-thickness epithelial dysplasia (CIS) to invasive SCC, when tumor cells invade through the epithelial basement membrane. Fortunately, of these conditions, invasive SCC is the least common.
Please review the below case on OSSN to better understand the diagnosis, management, and prognosis of these lesions.
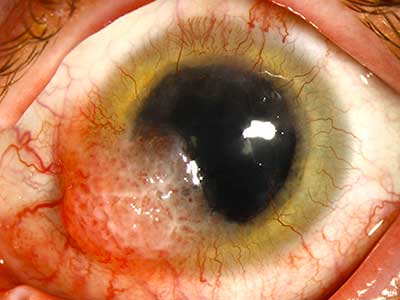
References:
Oculus sinister (OS) refers to the left eye.
Oculus uterque (OU) refers to both eyes.
Primary acquired melanosis refers to a melanocytic lesion on the conjunctiva; these are usually patchy areas of flat, brown pigmentation. Once noted, it should be followed over time because of the possibility of malignant transformation into melanoma. Management can vary based on severity, but biopsy is generally recommended to assess risk of malignant transformation. Progression to melanoma can be assessed by extent of spread of PAM in clock hours across the eye and level of atypia on biopsy. One study found that of 311 eyes, 35% had enlargement of PAM at 10 years and 12% had transformation into melanoma (217). They saw 0% transformation in PAM without atypia or with mild atypia and 13% transformation in PAM with severe atypia.

References:
Synechiae are adhesions between two structures in the eye. Peripheral anterior synechiae refers to an adhesion between the iris and trabecular meshwork. This can be caused by an inflammatory process such as uveitis or by a force pushing the two structures together, such as in closed-angle glaucoma. Gonioscopy will show the adhesion and allow assessment of how much of the angle is affected (218). Management is usually based on the underlying cause.
The below image is an example of PAS in a patient with iridocorneal endothelial syndrome, which classically is associated with high PAS formation and angle closure glaucoma.
References:
Pseudophakic bullous keratopathy occurs when trauma during cataract surgery causes the loss of the corneal endothelial cells. Patients with underlying corneal endothelial dysfunction may be at higher risk for developing PBK. Because these endothelial cells are responsible for transporting fluids and solutes out of the cornea to ensure transparency, dysfunction causes corneal edema with epithelial and/or subepithelial bullae formation.
Because of the high density of nerve endings in the cornea, PBK is commonly associated with pain, photophobia, and tearing. PBK is an uncommon complication of cataract surgery, affecting 1-2% of patients (220). Treatment involves administration of topical dehydrating agents, intraocular pressure-lowering agents, and, in some cases, therapeutic soft contact lenses. Corneal transplant is often curative in the most severe cases.
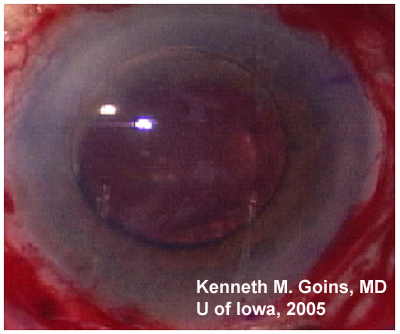
References:
A PCIOL is an artificial lens surgically placed in the posterior chamber of the eye. The lens can be placed in either the original lens capsular bag if it is still intact or within the ciliary sulcus. Placing the lens in the capsule is generally preferred but not always possible if the capsule or supporting structures have been damaged (221).
There are numerous cataract and intraocular lens videos on EyeRounds.org: Cataract procedures.
References:
Posterior capsular opacification is also referred to as a “secondary cataract,” which can form following cataract surgery. It involves leftover lens epithelial cells on the anterior capsule proliferating and eventually spreading to the posterior capsule. These cells eventually reach the visual axis of the capsule and scatter light, which can result in a loss of vision and increased glare problems (222).
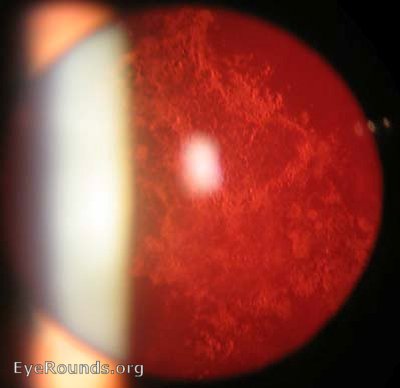
References:
Prism diopters are used to measure the refractive power of a prism. Prisms refract light and are used in ophthalmology to move an image through bending the light. This is useful for treating conditions like strabismus, where the eyes are misaligned. A pair of glasses with a prism on the deviated side can effectively move the image to adjust for the misalignment, thus correcting any diplopia the patient may experience (224). Prism diopters correlate with the angle that light bends when it passes through the prism. For every 1 prism diopter, light measured 100 cm past the prism will bend 1 cm.
References:
Diabetic retinopathy is a chronic disease of the vasculature of the eye in diabetic patients. It can take on one of two forms: proliferative or non-proliferative. PDR is the more advanced stage of diabetic retinopathy and is characterized by new vessel formation (see NV) in an attempt to perfuse tissues suffering from ischemia due to small vessel damage. Additional findings unique to PDR are vitreous or preretinal hemorrhages, which take on a boat-shaped appearance.
Treatment can involve laser panretinal photocoagulation (PRP), in which the peripheral retina is treated with a laser to ablate the ischemic tissue and suppress release of VEGF (vascular endothelial growth factor). Alternatively, an anti-VEGF medication can be injected intravitreally to suppress VEGF and stop proliferation of vessels (225).

References:
Pigmentary dispersion syndrome involves abnormal accumulation of pigment from the iris within the aqueous humor. This occurs due to friction between the lens zonules and posterior iris surface as they rub past each other, which leads to scattering of pigment into the anterior chamber and posterior chamber. The pigment can collect in the trabecular meshwork and impede draining of aqueous humor, leading to elevated intraocular pressure and pigmentary glaucoma in some cases. One study estimates pigmentary glaucoma affects between 0.5-5% of people with glaucoma in the Western world (227).
Please review this case on pigmentary glaucoma for additional information on diagnosis and management.
References:
Photodynamic therapy involves using a photosensitizing agent and light to cause a chemical reaction at a specific location. The agent is stable until exposed to a specific wavelength of light, at which point it activates and causes the desired chemical reaction. PDT can be used in many different medical conditions but in ophthalmology is primarily used to treat vascular abnormalities in the choroid and retina.
PDT is used most commonly to treat central serous retinopathy (CSR), neovascular age-related macular degeneration, and choroidal hemangiomas. An agent called verteporfin is typically used in these treatments. When exposed to light, it reacts with local substrates and releases free radicals that can damage and kill local cells. This makes it effective as a targeted therapy to stop neovascularization-induced pathology while minimizing systemic toxicity (228).
References:
Pigmentary epithelium detachment refers to detachment of the retinal pigment epithelium (RPE) from the choroid. Several different diseases can cause this detachment with varying pathogenesis, but the most common cause is age-related macular degeneration (AMD). In AMD, degenerative changes in Bruch’s membrane, which is the tissue layer between the choroid and retinal pigment epithelium, is believed to contribute to PED. Accumulation of cellular waste products and lipids in Bruch’s membrane can destroy the normal tissue architecture, facilitating detachment of the RPE from the choroid. This can occur alongside drusen formation in the space created by detachment and neovascularization, both of which can worsen PED. PED and associated complications can be sight-threatening and contribute to loss of central vision (229).
References:
Punctate epithelial erosions are commonly seen in the context of dry eye syndrome (DES). They are spots in which inadequate tear film and lubrication have caused small erosions in the cornea. On a tear film breakup test, punctate epithelial erosions as well as evidence of tear film breakup in less than 10 seconds are both characteristic of evaporative dry eye disease (230).
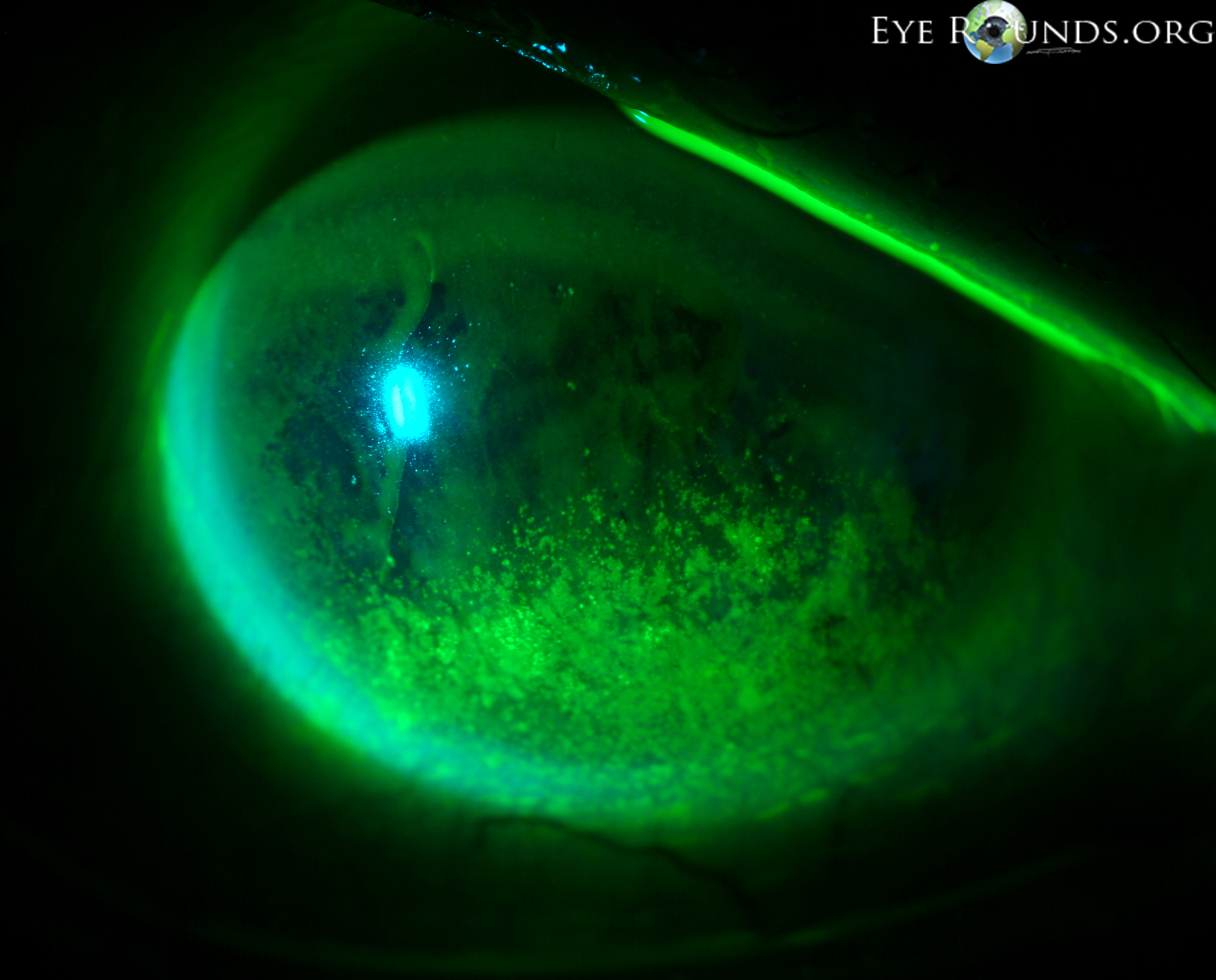
References:
Punctate epithelial keratitis involves small pointed lesions on the surface of the cornea secondary to an inflammatory process. Some common causes of PEK are viral infections, such as with herpes simplex virus (HSV). While HSV keratitis is not the only cause of PEK, it is the leading cause of infectious blindness in developed countries, so it must be on the differential when evaluating a patient with punctate epithelial keratitis (232). Early HSV keratitis will cause PEK while later in the disease larger ulcers will be visible on fluorescein staining. Treatment of PEK is dependent on the underlying etiology but may include antibiotic ointment, topical antivirals, and/or topical corticosteroids.
References:
Punctate epithelial keratitis involves small pointed lesions on the surface of the cornea secondary to an inflammatory process. Some common causes of PEK are viral infections, such as with herpes simplex virus (HSV). While HSV keratitis is not the only cause of PEK, it is the leading cause of infectious blindness in developed countries, so it must be on the differential when evaluating a patient with punctate epithelial keratitis (232). Early HSV keratitis will cause PEK while later in the disease larger ulcers will be visible on fluorescein staining. Treatment of PEK is dependent on the underlying etiology but may include antibiotic ointment, topical antivirals, and/or topical corticosteroids.
References:
Prednisolone Acetate 1% is a corticosteroid eye drop used to treat certain inflammatory conditions of the conjunctiva, cornea, and uvea. It is commonly prescribed in the post-operative period after eye surgery to decrease the amount of inflammation. Corticosteroid eye drops must be used with care as they can cause elevated intraocular pressure (IOP) and lead to glaucoma. Additionally, secondary infection can occur in the context of the immune suppression that PF causes.
The palpebral fissure is the opening between the eyelids, measured as the distance between the upper and lower eyelids (MRD1 + MRD2; height) and the medial and lateral canthi (width). Variations in the size and slant of the palpebral fissure are normal between people but also can be seen in some developmental conditions, such as fetal alcohol syndrome, Down syndrome, and Marfan syndrome (233). Surgery may be done to widen the palpebral fissure for cosmetic reasons or to preserve sight, such as in patients with acquired ptosis (234).
References:
Artificial tears are used to lubricate the eye, especially in the context of dry eye syndrome (see DES). While preservative-free artificial tears can be more expensive, there is some evidence that some preservatives, such as benzalkonium chloride, can reduce nerve fiber density and aqueous tear production (235). Because of this, preservative-free artificial tears are generally the preferred product to recommend to patients.
Please review this comprehensive evaporative dry eye tutorial to learn more about dry eye diagnosis and management.
References:
Perfluoron, also called perfluorocarbon, is a heavy liquid used intraoperatively in the repair of a retinal detachment. Due to its density, low viscosity, and immiscibility in water, the PFO is able to displace sub-retinal fluid (SRF) and/or blood anteriorly, allowing for retinal unfolding and stabilization during repair. While the PFO is applying pressure to the retina, an endolaser can be used to laser the retina around tears or retinal pathology. The subretinal fluid can then be removed, along with the perfluoron, with replacement usually gas or silicone oil (236).
References:
Persistent fetal vasculature refers to a sporadic, non-heritable congenital eye disease where there is persistence of vasculature between the optic nerve and the lens. The hyaloid artery and associated tunica vasculosa lentis normally regress completely by the eighth month of gestation; however, in PFV, these vessels can remain anteriorly, posteriorly, or a combination of both. The stalk of vessels can block vision, halt eye development/growth, and/or contract and cause retinal detachment (237). PFV has a variable clinical presentation and outcome, but generally presents with leukocoria shortly after birth and requires surgical intervention to improve and preserve visual acuity. Please read the below case for a detailed overview of PFV pathophysiology, presentation, and management.
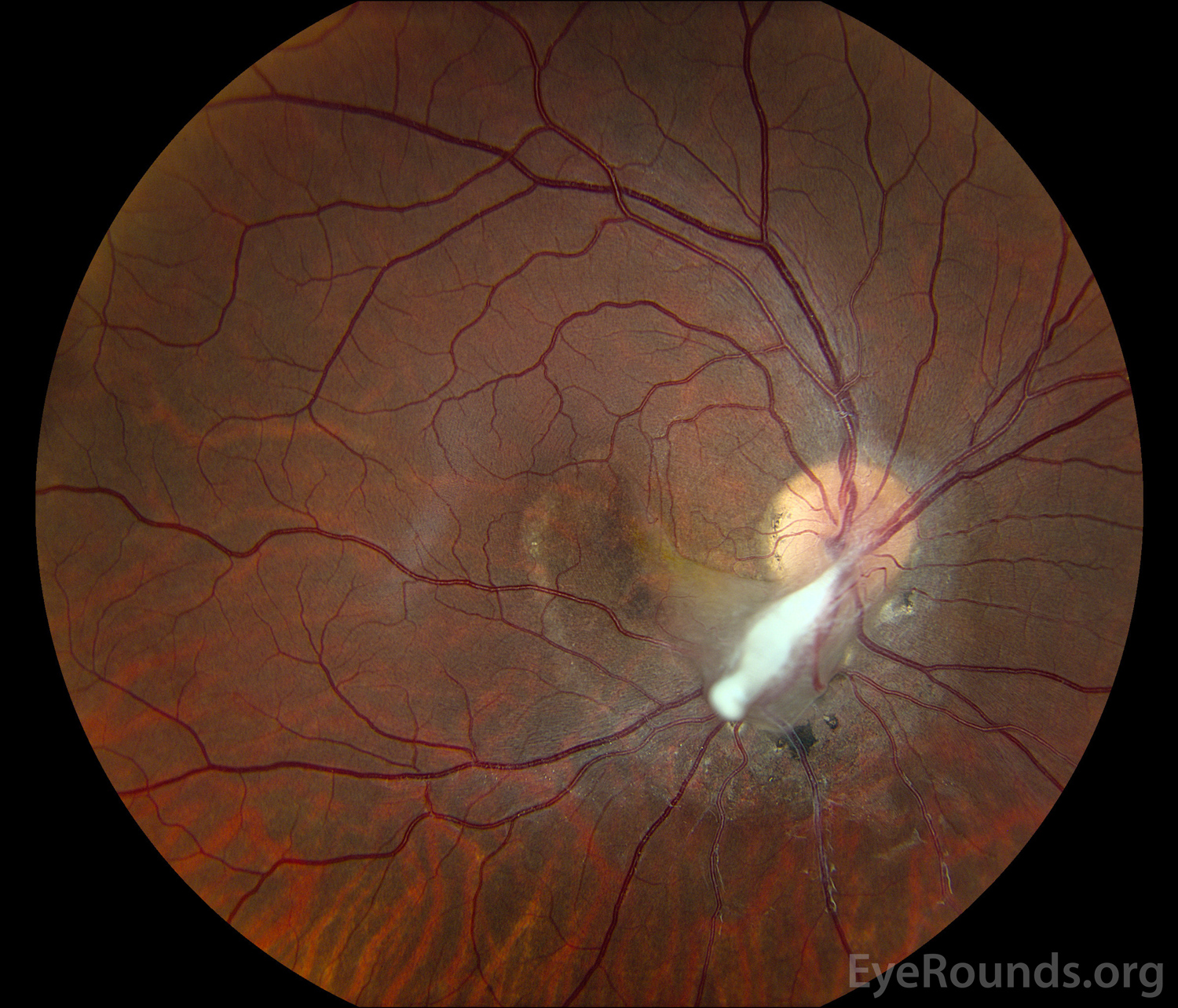
References:
A pinhole occlude/aperture is a device that blocks all light except for light coming straight through the pinhole. The purpose of a pinhole is to eliminate refractive error; light only passes through the center of the user’s lens, where refraction is not required to focus the light onto the macula. If a patient has poor visual acuity, use of a pinhole occluder is a simple way to tell if they have a significant refractive problem.
References:
Polyhexamethylene biguanide is used as a preservative in contact lens solutions as well as an eye drop to treat Acanthamoeba keratitis (238).
References:
Persistent hyperplastic primary vitreous was the prior name for persistent fetal vasculature (PFV). Persistent fetal vasculature refers to a sporadic, non-heritable congenital eye disease where there is persistence of vasculature between the optic nerve and the lens. The hyaloid artery and associated tunica vasculosa lentis normally regress completely by the eighth month of gestation; however, in PFV, these vessels can remain anteriorly, posteriorly, or a combination of both. The stalk of vessels can block vision, halt eye development/growth, and/or contract and cause retinal detachment (237). PFV has a variable clinical presentation and outcome, but generally presents with leukocoria shortly after birth and requires surgical intervention to improve and preserve visual acuity. Please read the below case for a detailed overview of PFV pathophysiology, presentation, and management.
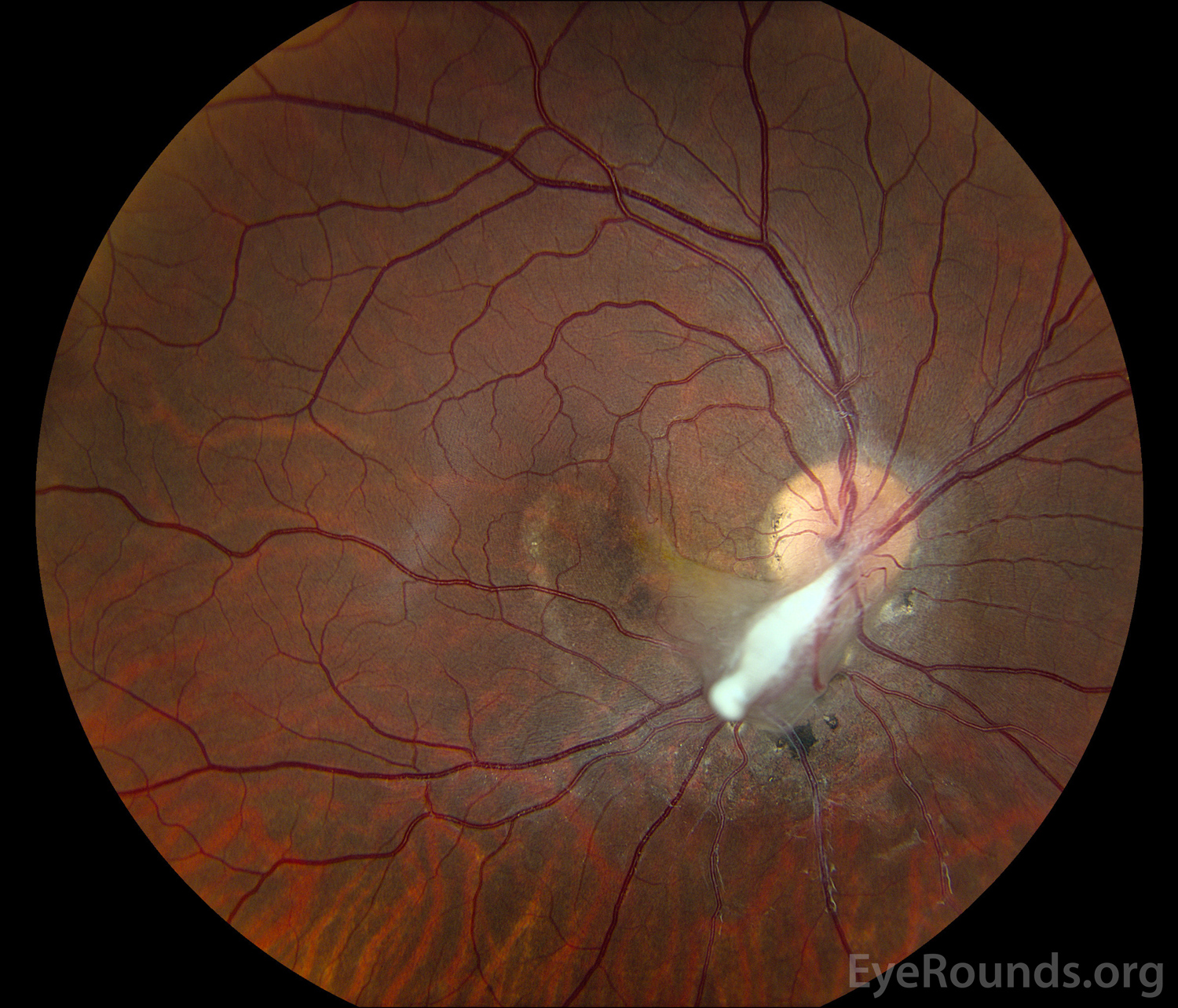
References:
Peripheral iridotomy is performed using a laser (usually a yttrium-aluminum-garnet, or YAG laser), to create a shunt between the anterior and posterior chambers of the eye. This process is indicated for pupillary block, when aqueous humor can’t flow through the pupil. In acute angle-closure glaucoma, rapid pressure elevation occurs as the aqueous humor is being produced with no outflow. In this situation, a peripheral iridotomy allows aqueous humor to flow into the anterior chamber and relieve the pressure (239).
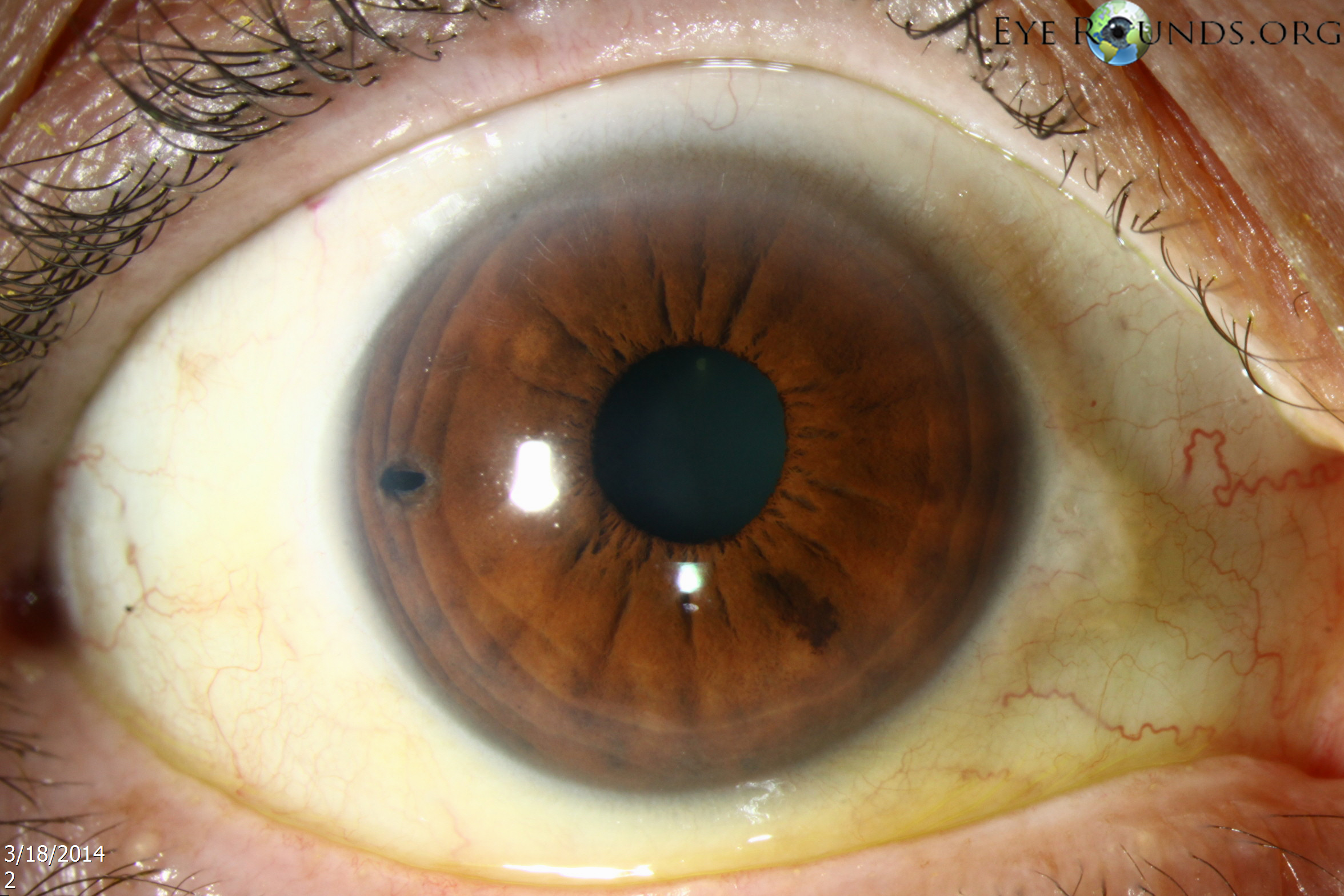
References:
Posterior ischemic optic neuropathy involves ischemic damage to the intraorbital portion of the optic nerve with acute, painless vision loss in one or both eyes. In contrast to the much more common anterior ischemic optic neuropathy (AION), PION has no visible changes in the optic disc until pallor occurs 6-8 weeks after the ischemic event. A relative afferent pupillary defect (RAPD) may be present; however, the diagnosis is difficult to make. PION has three main etiologies: peri-operative, arteritic, and non-arteritic. Perioperative PION is secondary to disruptions in blood delivery to the optic nerve in the setting of profound hypotension and poor perfusion during or around a procedure. Arteritic PION is most likely related to giant cell arteritis (GCA), whereas non-arteritic PION may be due to systemic vascular diseases, similar to NAION (240).
Review the risk factors and management of PION here.
Penetrating keratoplasty is a full-thickness corneal transplant. This is in contrast to other methods of corneal transplant that may replace selective layers of the cornea depending on the patient’s pathology. PKs are performed primarily for visually significant stromal scarring, opacities with significant posterior corneal involvement, and corneal ectasia. As with any graft, rejection is a concern, but anti-rejection drugs are not needed for corneal transplants.
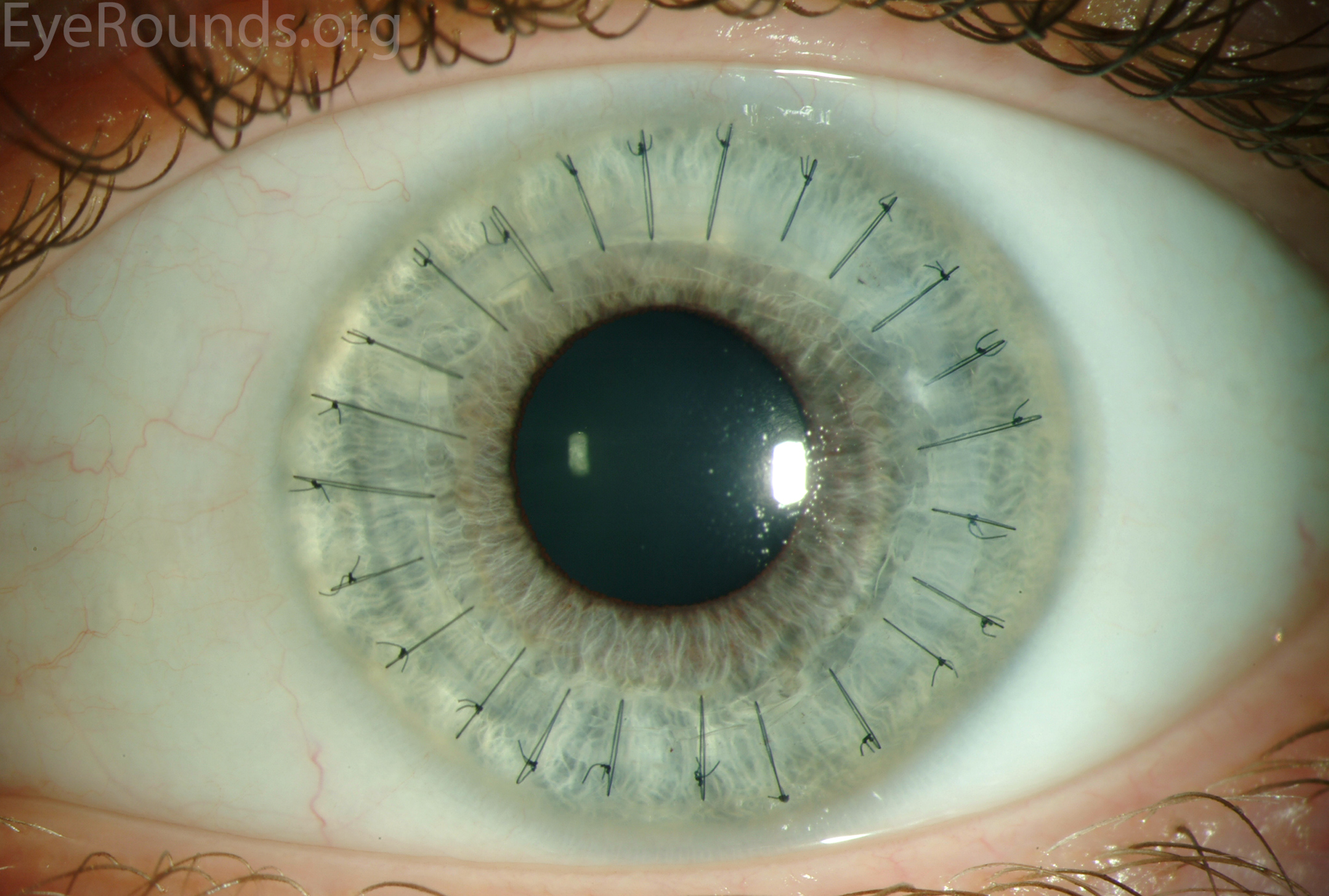
References:
Past medical history is a section of the patient interview alongside history of present illness, social history, family history, physical exam, and review of systems. It typically consists of the patient’s chronic health problems, medications used, history of surgeries, previous hospitalizations, medication allergies, and immunization history.
PO is short for “per os” in Latin, which translates to “by mouth”. It is generally used in relation to oral medications as opposed to other routes of administration, such as topical, intravenous, or sublingual.
Primary open angle glaucoma involves damage to the optic nerve, usually due to elevated intraocular pressure, but without blockage of the iridocorneal angle. In open angle glaucoma, other pathologic processes such as reduced flow through the trabecular meshwork lead to elevated intraocular pressure without iridocorneal angle closure. This leads to optic nerve damage which can be observed on fundoscopy as an elevated cup to disc ratio and loss of neuroretinal tissue.
Glaucoma can occur insidiously over time, so it is important to screen adults by documenting the intraocular pressure, examining optic nerves, and testing visual fields. Glaucoma commonly causes an arcuate visual field loss that respects the midline, causing an arc-shaped loss of visual acuity in either the superior or inferior hemisphere of vision.
Review the POAG and glaucoma management videos using the Iowa Glaucoma Curriculum.
References:
Presumed ocular histoplasmosis syndrome is secondary to Histoplasma capsulatum infection. Histoplasmosis is a fungal infection typically seen in the Midwest and Southern United States. POHS causes peripapillary atrophy and chorioretinal scars and can lead to choroidal neovascularization membranes (see CNVM) under the retina, which can result in central vision loss if present in the central macula. These areas of choroidal neovascularization can be treated through laser photocoagulation in areas outside the macula or anti-VEGF therapy (241).
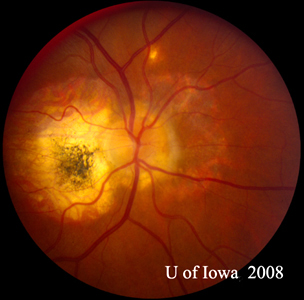
References:
Progressive outer retinal necrosis is a vision-threatening necrotizing herpetic retinopathy generally associated with HIV/AIDS and varicella zoster virus (VZV). It can be rapidly progressive given it is most commonly seen in AIDS patients and others who are severely immunocompromised. VZV infection causes necrosis in all layers of the retina with minimal inflammation and few hemorrhages (unlike ARN). There are commonly patchy areas or outer retinal whitening that coalesce rapidly with posterior pole involvement. Ganciclovir or foscarnet should be promptly administered intravitreally along with systemic anti-viral therapy (243).
Peripapillary atrophy refers to thinning of the choroid and retina as well as the retinal pigment epithelium around the optic disc. It is seen in eyes with high myopia, as well as eyes with glaucoma. It can be assessed through optical coherence tomography as a marker for glaucomatous damage, but overall it is non-specific and doesn’t indicate ocular damage is happening. On fundoscopy, a “beta zone” will be visible as a darker zone around the optic disc which correlates with the neuroretinal rim (the larger the beta zone, the thinner the rim). This area is actually the underlying choroidal vasculature which is visible due to atrophy of the tissue normally overlying it (244).

References:
A purified protein derivative test is used to evaluate if a person has been exposed to tuberculosis (TB). It involves an intradermal injection of a combination of proteins from Mycobacterium tuberculosis and evaluating it 2-3 days later for a response. The size of the surrounding induration is then evaluated along with the patient’s individual risk factors to establish if they have been infected by tuberculosis or not. One important note is that if someone has received the BCG vaccine against tuberculosis, they may test positive even if they do not carry the organism.
References:
Pars plana lensectomy is a method for extracting the lens through the pars plana region, which is an area of the eye behind the ciliary body but anterior to the retina. In cataract surgery, most lenses are removed anteriorly. However, in some eyes with complicating conditions, removing the lens posteriorly through the pars plana may carry a better risk-benefit profile (245). One example in which PPLx would be indicated is subluxation of the lens posteriorly into the vitreous, such as in Marfan syndrome.
References:
Posterior polymorphous corneal dystrophy is a rare, autosomal dominant disease of the corneal endothelium. The corneal endothelium is responsible for osmotic balance in the cornea. In PPMD, dysfunction in the corneal endothelium and Descemet’s membrane, the layer underneath the endothelium, can lead to corneal edema and further complications. This happens through proliferation of epithelial cells, which replace the endothelium and disrupt its function (246). Clinically, there are endothelial vesicle-like lesions, band lesions, and diffuse opacities. Treatment can consist of Descemet membrane endothelial keratoplasty (DMEK) or penetrating keratoplasty (PK) in more severe cases.

References:
Pars plana vitrectomy is a procedure in which the vitreous humor is removed through the pars plana, which is an area of the eye posterior to the ciliary body and anterior to the retina. Going through the pars plana allows entry into the vitreous chamber without damaging the retina, reducing the risk of complications like retinal detachment. Vitrectomy is used in treatment of a number of diseases, including but not limited to retinal detachment, vitreous hemorrhage, vitreomacular traction, epiretinal membrane peel.
References:
A photoreceptor is a cell that absorbs light and transduces it into a neurological signal. These cells exist as rods or cones. Rods are responsible for low light vision and are much more sensitive to light, requiring a lower threshold in order to be stimulated. Cones are responsible for color vision and require more visual stimulation via brighter light.
There are numerous photoreceptor diseases, most which are inherited retinal degenerations. These include retinitis pigmentosa, cone rod dystrophy, Leber congenital amaurosis, congenital stationary night blindness, among many others. Please visit StoneRounds to review photoreceptor diseases in detail.
Posterior reversible encephalopathy syndrome is a neurological syndrome that involves rapid onset of symptoms, such as seizures, headache, altered mental status, and visual problems. It is often associated with acute hypertension (170-190 systolic), which is believed to be the trigger in most cases. It is thought that PRES occurs through disrupted autoregulation of blood flow to the brain and/or endothelial dysfunction, which reduces perfusion and causes neurologic symptoms (248). Diagnosis is achieved through computed tomography (CT) and magnetic resonance imaging (MRI), and management involves treating the underlying cause through managing systemic inflammatory disease and controlling hypertension.
Photoreactive keratectomy involves using a laser to treat refractive errors by reshaping the cornea. PRK is a surface ablation technique that, unlike LASIK, does not require a surgical flap to ablate the stroma within the cornea. Instead, the epithelium is removed by one of several methods, including alcohol, blade, or brush. The Excimer laser procedure is similar to LASIK. Unlike LASIK, PRK patients often have post-operative pain due to the large corneal abrasion and the vision improves over several weeks to months (not days like LASIK). Please review the below tutorial to learn about these procedures, indications, and complications.
References:
PRN is a common abbreviation that stands for “pro re nata”, which is Latin for “when necessary.” It generally refers to medications and will appear as “give every 6 hours prn”, which means the medication can be given as often as every 6 hours but only if the patient requests it or it is indicated. PRN is often followed by a descriptor such that the medication is only given “as needed for pain,” for instance. The alternative is a scheduled drug, which in this example would be one given every 6 hours whether the patient requests it or not.
Panretinal photocoagulation is a treatment for certain retinal conditions that involves employing laser spots to the retina to prevent neovascularization (NV) in diseases, such as proliferative diabetic retinopathy (PDR), central retinal vein occlusion (CRVO), ocular ischemic syndrome (OIS), etc. Untreated NV and retinal ischemia can lead to retinal detachment with threatened vision. Because the macula is spared, vision is mostly preserved with some patients noting some decrease in peripheral vision. Intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) can inhibit neovascularization while minimizing trauma to the retina. However, one study found worse outcomes in eyes with proliferative diabetic retinopathy that received only anti-VEGF compared to PRP (249). PRP is a more definitive options than injections and should be considered in all high risk PDR eyes or in patients who may have trouble making clinic appointments.
References:
Posterior synechiae are abnormal attachments between the iris at the pupillary margin and anterior lens capsule. This limits pupillary dilation, causes irregular pupil shape, and can cause angle closure glaucoma by blocking aqueous humor flow from the posterior chamber to the anterior chamber. In contrast, peripheral anterior synechiae occur with there are attachments between the peripheral iris and the cornea, potentially closing the angle. Both types of synechiae can lead to elevated intraocular pressure. Posterior synechiae are often a result of severe or chronic uveitis. However, this can also occur as a complication during some ocular surgeries or trauma if the lens is involved (250).

References:
A posterior subcapsular cataract is a cataract that forms on the posterior side of the lens underneath the lens capsule. This is in contrast to some of the other common types of cataract, such as nuclear and cortical cataracts. Posterior subcapsular cataracts can occur as a normal age-related cataract, but they usually occur due to ocular inflammatory conditions, diabetes mellitus, topical steroid use, and/or procedures, such as pars plana vitrectomy. PSC differs from other cataracts in that dim light vision is preserved but visual acuity decreases in bright light. PSC is also found to cause a myopic shift in affected eyes, which can cause them to act more nearsighted (252).
References:
Peripheral ulcerative keratitis is an inflammatory condition affecting the cornea. It is typically associated with systemic inflammatory conditions, such as rheumatoid arthritis, and can have serious consequences for vision if allowed to progress. One such complication is corneal melt syndrome, in which progressive corneal thinning can result in corneal perforation. PUK typically presents with corneal ulceration, usually crescent-shaped and within 2 mm of the limbus (254). Treatment generally consists of systemic corticosteroid therapy and may use other non-steroidal immunosuppressive therapeutics to spare steroids in chronic treatment.
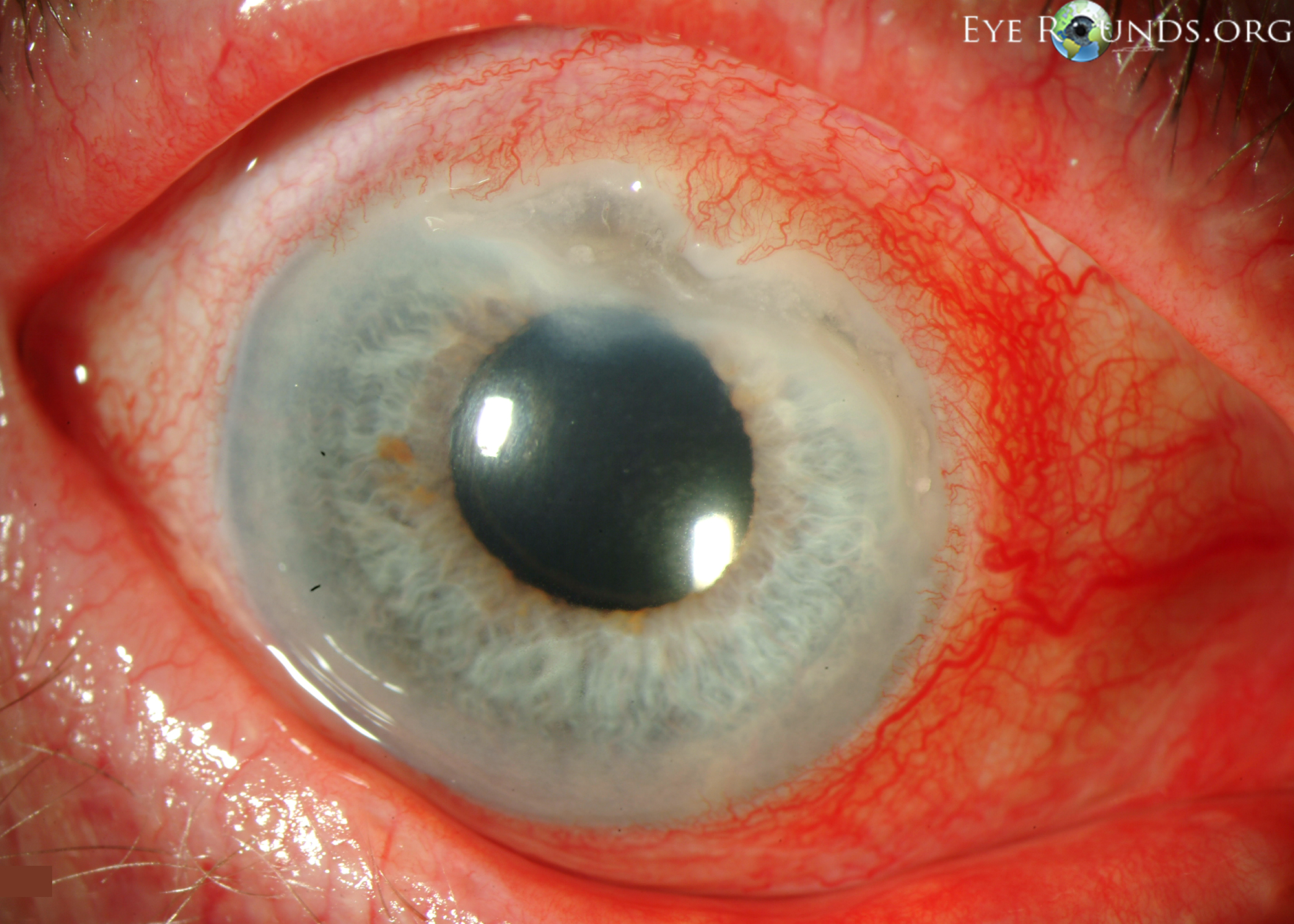
References:
Posterior vitreous detachment is a generally benign process in which the vitreous humor and hyaloid separate from the retina. It occurs much more frequently with age, with prevalence increasing from 24% in 50-59 year old patients to 87% in 80-89 year old patients (255). An acute PVD is associated with increased risk of retinal tears and/or detachment.
The floaters (small objects in the field of view) are caused by abnormal vitreous folding or aggregations of cells or collagen. The other characteristic symptom is flashes, which appear to the patient as sudden flashes of light in their vision, caused by the vitreous pulling on the retina and activating photoreceptor cells. Because both of these symptoms are present in PVD and retinal tears, a thorough exam should be performed to rule out peripheral retinal pathology that may need urgent treatment.
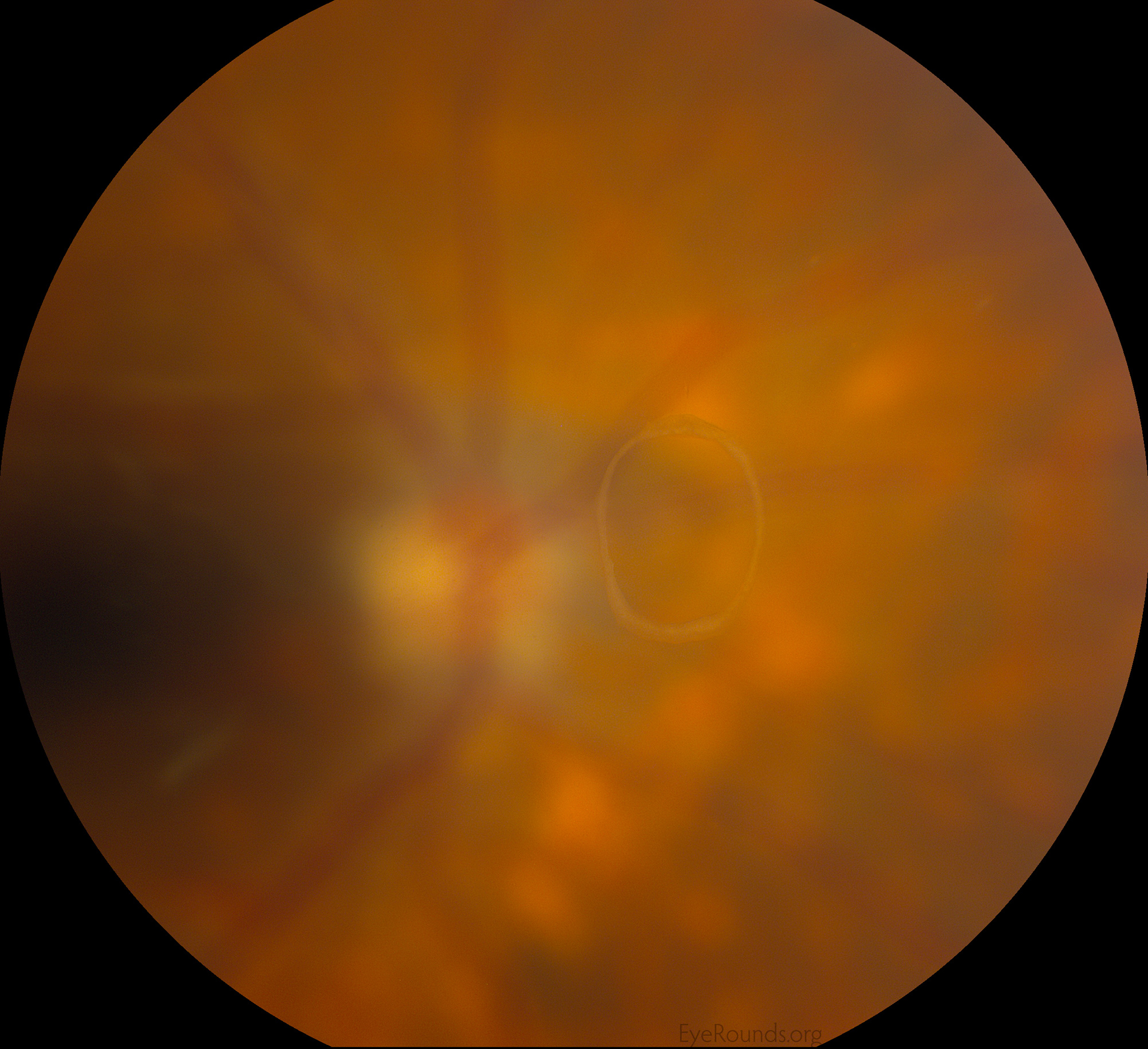
References:
Proliferative vitreoretinopathy occurs when proliferating cell sheets are present in the vitreous humor and in the periretinal area. These cell sheets form a epiretinal membrane, which causes traction in the retina and can lead to retinal detachment. This typically occurs as a late complication after a retinal detachment is repaired (256).
References:
Pseudoxanthoma elasticum is an autosomal recessive genetic disease involving the ABCC6 gene, which results in abnormal mineralization of elastic tissues. Small yellow papules (raised bumps) on the back and sides of the neck as well as in sites of flexion are characteristic of PXE. PXE can have serious ophthalmologic sequelae as it can create “angioid streaks” in the retina, which represent damage to Bruch’s membrane in the choroid. This can result in choroidal neovascularization and subretinal hemorrhages (258).
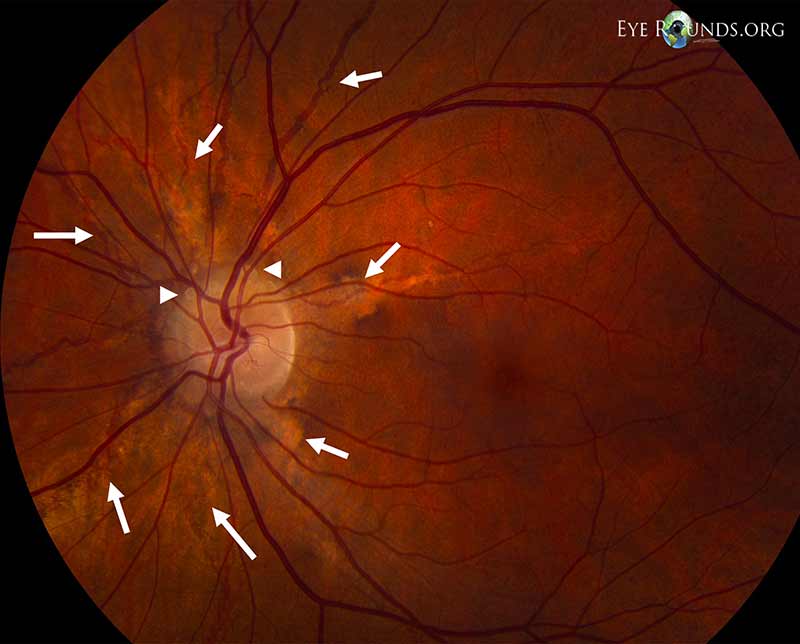
References:
Pseudoexfoliation syndrome is a systemic disease that involves accumulation and deposition of various material, called pseudoexfoliative material, in extracellular locations throughout the body. This material can be made of collagen, amyloid, elastic fibers, or other normal body materials. It is inconclusive exactly what role pseudoexfoliation syndrome plays systemically, but it is clear that it causes ocular pathology, such as pseudoexfoliation glaucoma. The diagnosis of PXF is made definitively through visualizing pseudoexfoliative material on the anterior lens. PXF is associated with a higher risk of cataracts and higher rates of surgical complications for any surgery done on the eye (260).
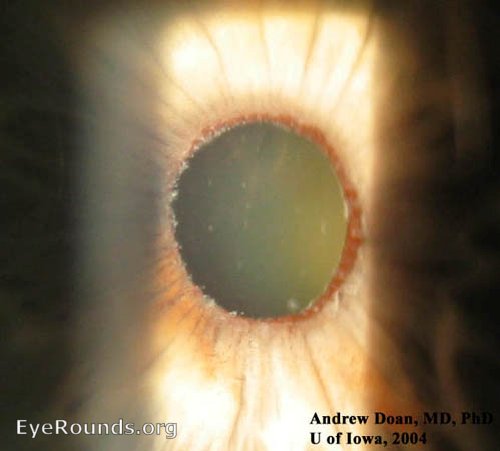
References:
q1h is used to indicate something should be done every hour. This might refer to a medication or blood work.
q2h indicates something should be done every other hour.
qAM is usually used to specify medications should be specifically taken or administered in the morning.
qd means something should be done once daily but doesn’t specify morning, afternoon, or evening.
HS refers to “hora somni”, which means at bedtime. qHS is generally used to indicate medications should be taken/administered at bedtime.
QID indicates something should be done four times a day, usually every 6 hours.
“Round and reactive” is a common way to describe the pupils. A quick examination with a light can give two important pieces of information – the symmetry and responsiveness of the pupils. If the pupils are round, that helps rule out trauma that might cause a peaked pupil. If the pupils are both responsive to light, that makes damage to cranial nerves II and III less likely. Asymmetric pupils might indicate a unilateral brain or cranial nerve injury.
References:
Rheumatoid arthritis is an inflammatory autoimmune arthritis that characteristically affects the joints of the hand and wrist but can have other systemic effects. Rheumatoid arthritis is typically treated with DMARDs, or disease modifying anti-rheumatic drugs, in order to slow progressive degeneration of joints. RA is associated with peripheral ulcerative keratitis (see PUK), dry eye syndrome (See DES), anterior scleritis, scleromalacia, and episcleritis (262). Treatment of these conditions may be long-term and require collaboration with a rheumatologist, as RA is a lifelong disease and these conditions can be debilitating enough to require treatment.
A relative afferent pupillary defect is an exam finding that suggests unilateral optic nerve damage, such as in compressive thyroid eye disease, and/or severe retinal damage, such as with a central retinal artery occlusion (CRAO). An RAPD is identified using the swinging flashlight test, in which a light source is directed into each eye individually, alternating between the eyes. If the eye is normal, then both pupils should constrict when a light is directed into the normal eye. If the optic nerve and/or retina are damaged, both eyes will fail to constrict when the light is directed into the abnormal eye.
Consult this article by Dr. David Broadway for a more detailed description of RAPD and the swinging flashlight test (263).
Retinoblastoma is a childhood cancer deriving from retinal cells. While it is a rare tumor, it is the most common primary malignant intraocular cancer in children and it has a good prognosis with treatment, so screening for retinoblastoma is important (264). The most common finding in children with retinoblastoma is leukocoria, or an abnormal red reflex that appears white. This is due to the tumor disrupting the normal red reflex. Treatment may consist of enucleation to remove the primary tumor in advanced cases, but there are many adjunct options including radiation, laser, and/or chemotherapy that may treat the tumor and salvage the eye.
References:
Risks, benefits, and alternatives should be discussed with every patient whenever a medical decision is made. An example of this would be counseling a patient on side effects of medications or discussing the lifestyle changes they can make as an alternative to starting a medication. This process is especially important pre-operatively so that the patient can provide informed consent.
A retrobulbar block is an anesthetic nerve block delivered through an injection to the retrobulbar space. The purpose of a retrobulbar block is to anesthetize the sensory nerves of the cornea, uvea, and conjunctiva, as well as paralyze the eye through inhibiting cranial nerves III, IV, and VI as well as the ciliary nerves. This is generally done for surgeries as an alternative to general anesthesia to avoid the risks associated with general anesthesia. A retrobulbar block can be uncomfortable to the patient as a needle must be inserted behind their eye, so it is usually paired with an IV sedative like a benzodiazepine and an analgesic such as fentanyl (266).
References:
Red blood cells facilitate oxygen delivery to tissues through hemoglobin, an iron compound that can store and release oxygen depending on its environment. RBCs are unique in that they have no nucleus or organelles and exist to deliver oxygen to tissues. Information related to RBCs is typically gathered with a complete blood count, or CBC.
Retinal detachment is a vision-threatening emergency involving the separation of the retina from the underlying retinal pigment epithelium. There are three types of retinal detachment: rhegmatogenous, tractional, and exudative. Rhegmatogenous is the most common and involves a break in the retina through which fluid flows underneath the retina and causes an expanding detachment. Tractional involves a force pulling the retina off of the retinal pigment epithelium, which could be from a vitreous detachment or from scar tissue. In exudative, fluid accumulates underneath the retina usually as a result of trauma or inflammation but without a break in the retina.
Retinal detachment treatment is aimed at reattaching the retina and preventing further detachment. Treatment is tailored to the etiology of the detachment, but generally it involves placing a gas bubble or silicone oil into the vitreous chamber to apply pressure to push the retina back onto the retinal pigment epithelium. Laser phototherapy or cryotherapy may be used to seal breaks in the retina and to prevent areas of fluid accumulation underneath the retina from spreading (267).
References:
Rheumatoid factor is an autoantibody that is named for rheumatoid arthritis (RA), as it was first found in patients with RA. RF is an antibody against the tail end Fc fragment of an IgG antibody and can be identified as part of lab work in patients that may have RA. RF can be elevated in many other diseases or even as a benign finding, so RF can’t be diagnostic of any one disease without further diagnostic work-up.
Children with juvenile idiopathic arthritis (see JIA) have an increased risk of uveitis when the RF antibody is negative.
Rigid gas permeable lenses allow oxygen access to the cornea at the cost of initially being less comfortable than soft contact lenses. Rigid gas permeable lenses are generally better for patients with dry eye as they allow tears to flow underneath the lens.
A major benefit of scleral RGP contact lenses over corneal RGP contact lenses is that scleral lenses completely vault the cornea.
Rhabdomyosarcoma is a mesenchymal soft tissue cancer that accounts for 5% of all childhood cancer (268). Rhabdo has a familial component, although most cases occur sporadically. Rhabdo is often on the differential diagnosis for pediatric ophthalmologists as it can present in the soft tissues of the orbit. It has a bimodal age distribution with peaks in the 2-6 age range and 10-18 age range. It is a do-not-miss diagnosis as it has a good prognosis if caught early before it spreads. It presents as a painless mass that may cause proptosis, or bulging of the eye, along with displacement of the globe depending on location. Treatment plans depend on the patient but often include chemotherapy, radiation, and surgical removal of the primary tumor.
References:
Radial keratotomy is a surgical procedure in which incisions are made at regular intervals in the cornea to treat keratoconus, myopia, and astigmatism. The incisions go from the edge of the cornea to just short of the center of the cornea. RK can be done with 4, 8, 12, 16, or 32 incisions depending on the patient and surgeon. RK has largely been replaced by modern refractive surgeries like photorefractive keratectomy (PRK) and LASIK due to issues with complications and long-term stability (269).
The retinal neve fiber layer is a measurement of the thickness of the optic nerve as it reaches the retina. Evaluating the optic nerve and its thickness is important in glaucoma, where damage to the optic nerve will result in a thinner RNFL. Monitoring the RNFL is an important tool for tracking glaucoma progression over time which can help tailor the treatment plan. It can be measured through several clinical imaging modalities, such as confocal scanning laser ophthalmoscopy, optical coherence tomography, and scanning laser polarimetry (270).
The right lower lid is the lower eyelid of the right eye.
References:
Premature newborns are exceptionally vulnerable to health problems and the retina is no exception. Newborns experience a hyperoxygenated state; this hyperoxia leads to reactive oxygen species formation, which premature newborns are less equipped to deal with because they have fewer antioxidants. Reactive oxygen species can interrupt normal retinal vascularization, which causes hypoxia and induces vessel proliferation. This results in retinopathy of prematurity and can lead to retinal detachment in advanced cases.
Oxygenation in preterm neonates is a balancing act in which too little oxygenation can lead to increased mortality, but too much oxygen increases the risk of retinopathy of prematurity (271). Treatment in patients with severe retinopathy can consist of cryotherapy, but generally laser or anti-VEGF therapy is preferred. Please see the below ROP case for a detailed discussion of diagnosis, screening, and management.
References:
Retinitis pigmentosa describes a variety of genetic disorders that cause progressive visual loss through deterioration of the retina. RP is a heterogenous group of photoreceptor diseases with different modes of inheritance with different genetic abnormalities. Retinitis pigmentosa starts with night blindness, or nyctalopia, in the early stage, with preserved vision in normal lighting. Classically, RP starts with rod degeneration and eventually causes destruction of cones with central loss of vision and photophobia. Unfortunately, treatment options remain limited for RP, although gene therapy trials are promising.
Leber congenital amaurosis is the most severe retinal dystrophy, causing blindness by the age of 1 year. The first FDA approved gene therapy, Voretigene Neparvovec-rzyl (Luxturna), was developed for RPE65-associated LCA (189).
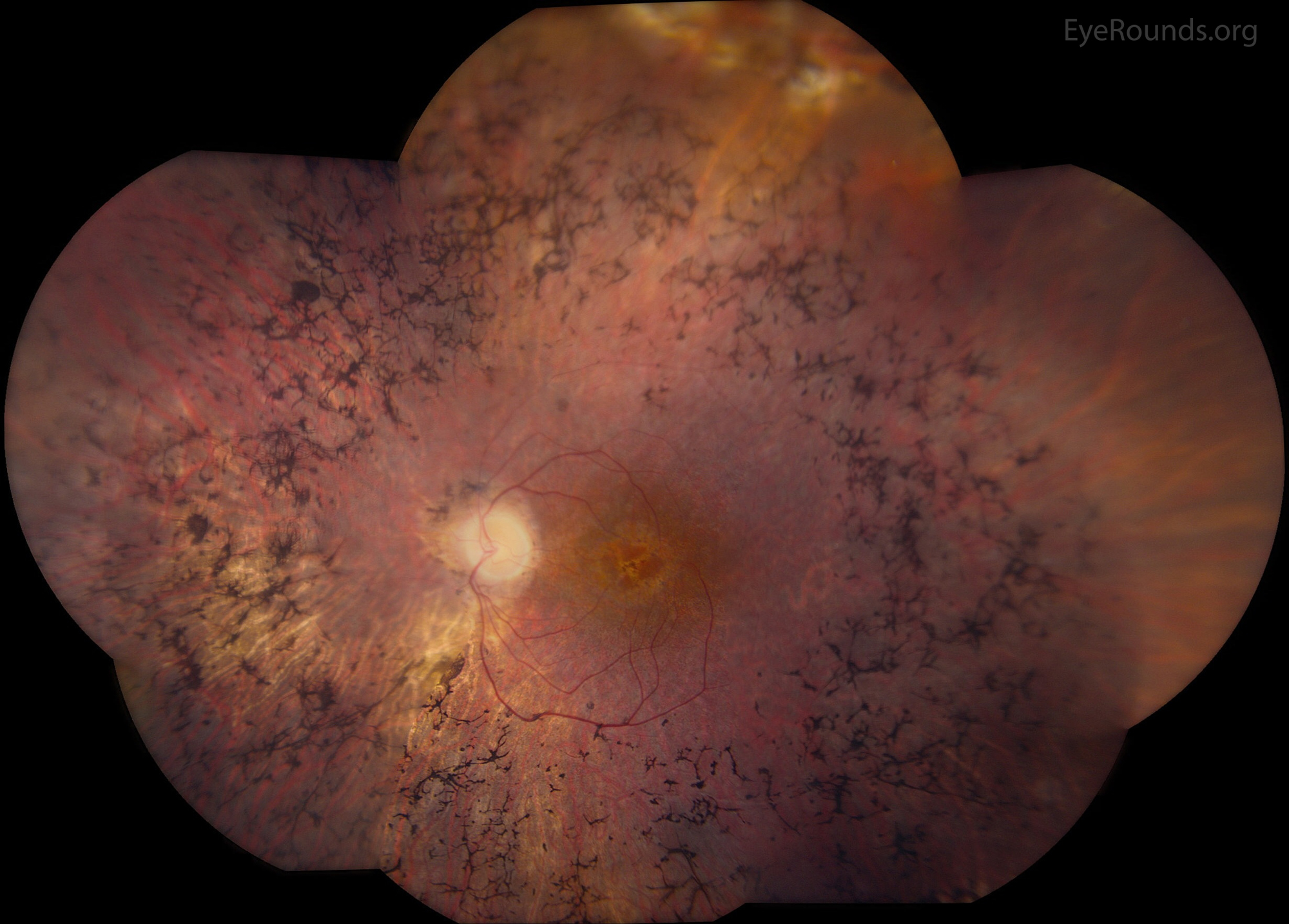
Please visit StoneRounds.org to learn more about inherited retinal diseases, including RP.
The retinal pigment epithelium is a layer of epithelial cells between the retina and choroid that are pigmented, causing them to have a dark appearance. The RPE is important in the visual cycle with the ability to uptake, transport, store, metabolize, and isomerize vitamin A. RPE also absorbs excess light that is not absorbed by the photoceptor cell. This helps stop photo-oxidative damage from occurring in the vessels of the choroid. The RPE also helps form the blood-retina barrier and contributes to the immune privilege of the eye, helping to prevent inflammatory processes from occurring that could threaten the eye (273).
An ATPase NA+/K+ pump, the retinal pigment epithelium cells help retinal adhesion with removal of subretinal fluid. Thus, the RPE plays an important role in some diseases of the eye like age-related macular degeneration (AMD). In AMD, deposits of cholesterol and protein accumulate between the RPE and Bruch’s membrane.
Rhegmatogenous retinal detachment involves a tear in the retina through which vitreous humor flows under the retina, causing a detachment from the underlying choroid. The urgency associated with diagnosis of a rhegmatogenous retinal detachment is that more fluid can keep flowing underneath the retina, causing further detachment. Retinal detachment is a medical emergency and needs urgent care by an ophthalmologist, as it can threaten vision if the detachment continues to worsen. The characteristic symptom of a retinal detachment is a “dark curtain” coming down or up over the patient’s vision in one eye (274). Other symptoms include flashes and floaters, which are flashes of light in one area of vision and small objects in the visual fields which are aggregates of protein or red blood cells in the vitreous humor.
Treatment involves several steps, the detached retina is reattached, followed by sealing of the retinal tear using laser therapy or cryopexy. Reattachment cab be performed with a scleral buckle, which is a thin silicone band placed around the eye to push the eye inward towards the detached retina, or vitrectomy, which involves replacing the vitreous humor with a gas bubble or silicone oil in order to tamponade the retina.
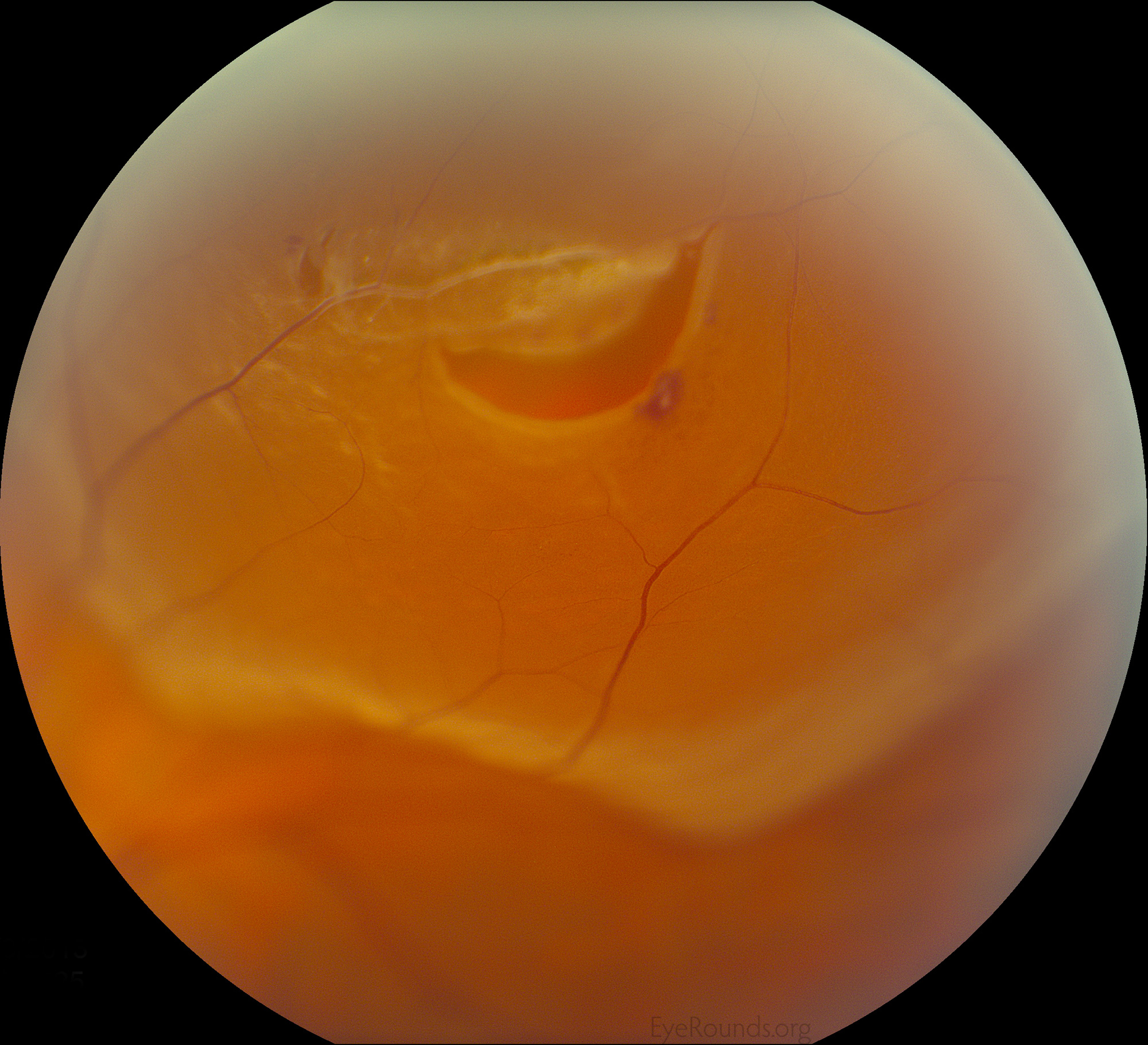
References:
RTC is an efficient way to write how soon the patient should return for a follow-up appointment. For example, “RTC 4 months” indicates a recommendation to follow-up in four months.
RUL is the upper eyelid of the right eye. The oculoplastics surgery techniques page has numerous videos on upper eyelid procedures, including biopsy, eyelid lesion removal, chalazion drainage, ptosis repair, blepharoplasty, tarsorrhaphy, and repair of upper eyelid entropion or retraction.
Status post is a way of denoting that a patient had something in their medical history. This is generally used to indicate procedures in the history, as you might want to denote that a patient is s/p peripheral iridotomy if they are being monitored for glaucoma.
A scleral buckle is a silicone band placed around the eye with the goal of applying pressure to the eye externally to relieve traction internally. Scleral buckles are primarily used in rhegmatogenous retinal detachments, in which a break in the retina causes accumulation of subretinal fluid from the vitreous. Bringing the retina back into contact with the wall of the eye aids in the absorption of the subretinal fluid and reattachment of the retina (275). Additionally, scleral buckling can aid in the closure of retinal tears through applying pressure to close the tear; this is commonly done in combination with either cryotherapy or laser with or without pneumatic retinopexy. Depending on the amount and distribution of subretinal present, this procedure may be combined with the external drainage of the subretinal fluid, usually with a needle.
Noting a visual acuity without correction indicates that it is the patient’s vision without any glasses or corrective eyewear. Displaying this along with the visual acuity with glasses or pinhole correction helps to know how much improvement the patient gets with refractive correction.
Squamous cell carcinoma is a cancer of the epidermis that is, in most cases, a skin cancer associated with excess UV radiation exposure, immunosuppression, or HPV. SCC carries a good prognosis if detected and treated early, which makes education and surveillance important.
Ophthalmology is primarily concerned with SCC of the eyelids, which is uncommon but just as dangerous as other forms of SCC if not detected as it can invade into nearby nerves or into the orbit. One study investigating eyelid SCC found lesions as small as 3mm and as large as 30mm, which again emphasizes the need for vigilance when the lesions are small (276). Treatment will generally consist of excision, with other options such as radiotherapy and cryotherapy depending on the patient.
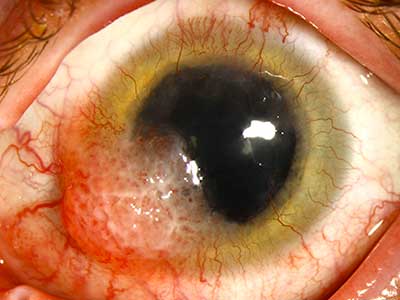
References:
Subconjunctival hemorrhage is generally a benign finding caused by a broken blood vessel within the conjunctiva. It can be frightening for patients to have a large blood spot on their eye, but patient should be reassured unless they have significant co-morbidities. For example, one case report found that in a 75 year-old woman, an epibulbar plasmacytoma was found that initially appeared like a subconjunctival hemorrhage (277). Some common causes are elevations in intraabdominal pressure such as straining and coughing or vigorously rubbing the eyes.
Ophthalmology is primarily concerned with SCC of the eyelids, which is uncommon but just as dangerous as other forms of SCC if not detected as it can invade into nearby nerves or into the orbit. One study investigating eyelid SCC found lesions as small as 3mm and as large as 30mm, which again emphasizes the need for vigilance when the lesions are small (276). Treatment will generally consist of excision, with other options such as radiotherapy and cryotherapy depending on the patient.

References:
Contact lenses come in two general categories: soft contact lenses and rigid gas permeable. Each have their advantages and disadvantages, but many people prefer soft contact lenses when they are first starting to wear contacts, because they are more comfortable and easier to put in. Soft contact lenses are also disposable, which some people find convenient. The disadvantage of an SCL is that they can dry out the eyes as they allow less oxygen supply to the eye. Rigid gas permeable lenses are better for those with dry eye and are more durable, but fall out of the eye or displace more easily and take more time to be worn comfortably.
A scleral depressed exam allows for a more complete examination of the peripheral retina via indirect ophthalmoscopy. A tool called a scleral depressor is inserted under the eyelid and pressed into the sclera at the location of a retinal lesion that needs better visualization. This pushes the retina towards the center of the eye and allows for better contrast between the lesion and retina. This is especially useful in a patient with suspected rhegmatogenous retinal detachment to visualize if a tear in the retina exists. Unfortunately, the SDE can be very uncomfortable for the patient. However, scleral depression is often a necessary procedure when performing laser retinopexy to ensure that there are adequate later burns surrounding a peripheral tear, especially if there is subretinal fluid present.
Subepithelial infiltrates are small leukocytes and particles underneath the epithelium of the cornea that are typically seen following epidermic keratoconjunctivitis, usually caused by an adenovirus. SEI occur following corneal involvement of the infection and will usually fade after 1-3 weeks but can persist for months to years in some cases. SEI can cause decreases in visual acuity, photophobia, visual halo effects, and glare so it can be debilitating for patients. Topical corticosteroids, antivirals, and cyclosporine can treat SEI, but some cases require further intervention such as phototherapeutic keratectomy, which is a safe and effective option for severe cases (279).
Stevens-Johnson Syndrome is a dermatologic emergency that involves widespread blistering and peeling of the skin and mucous membranes due to type IV, or T-cell mediated, hypersensitivity. SJS exists on a spectrum with toxic epidermal necrolysis, with SJS involving less than 10% of the skin and toxic epidermal necrolysis involving 10-30% of the skin. SJS is most commonly a drug adverse reaction but can be caused by an infection as well. Early discontinuation of the offending agent (allupurinol, anticonvulsants, and antibiotics are the most common) and rapid supportive treatment are crucial for improving outcomes, as mortality in SJS is about 1-5% (280).
Please review this case of ocluar manifestations of Stevens-Johnson syndrome.
Schwalbe’s line is the innermost (most posterior) layer of the cornea adjacent to the trabecular meshwork. Schwalbe’s line can be used to estimate how open the iridocorneal angle is when evaluating a patient for angle-closure glaucoma. This is done through a gonioscopic technique called parallelopiped technique, in which light reflections from the external surface and internal surface of the cornea come together at Schwalbe’s line. Once Schwalbe’s line has been identified using this technique, the trabecular meshwork can be evaluated as it is the full space between Schwalbe’s line and the scleral spur, which is easily visualized. While gonioscopy is the classic method for evaluating the iridocorneal angle, other methods using Schwalbe’s line such as optical coherence tomography also show efficacy in assessing the angle (281).
References:
Slit lamp examination is the standard tool in an ophthalmology clinic for visualizing the anterior and posterior structures of the eye. It is capable of providing a magnified view for visualizing the conjunctiva, cornea, iris, lens, and other structures of the anterior eye as well as doing a detailed fundoscopic exam. Once the SLE is complete, then additional examinations, such as indirect ophthalmoscopy, may be used to hone in on specific details with greater efficacy.
References:
Superior limbic keratoconjunctivitis is a chronic inflammatory disease involving the superior aspects of the outer eye (bulbar conjunctiva, upper cornea, and the limbus). It is a rare disease associated with autoimmune diseases, such as rheumatoid arthritis and autoimmune thyroid diseases. It tends to occur in women aged 30-55 years and is usually irritating and uncomfortable but not vision threatening. Because of the rarity of the disease, there is no gold standard treatment with options including surgical resection, cauterization, and topical therapy. One study investigating lodoxamide, an anti-inflammatory topical, found it was safe and effective (282) but no specific therapies are currently FDA-indicated for SLK.

References:
Selective laser trabeculoplasty is an outpatient laser technique for treating glaucoma. It aims to treat the trabecular meshwork and facilitate drainage of aqueous humor, thus lowering the intraocular pressure and preserving the optic nerve. Before SLT, the procedure was done using an argon laser, but it had more side effects and was technically more difficult to perform. SLT uses a neodymium-doped yttrium aluminum garnet (Nd-YAG) laser with a shorter pulse duration which has been shown to be effective and has considerably less side effects and ocular damage than an argon laser (284).
References:
Silicone oil is injected into the vitreous cavity intraoperative for treatment of retinal detachment. The process of placing a gas or liquid into the vitreous to apply pressure on the retina is called retinal tamponade. Retinal tamponade helps treat rhegmatogenous retinal detachment by applying surface tension on the retina, which helps prevent any fluid from entering the tear and accumulating under the retina. Silicone is less popular as an option for retinal tamponade because it is associated with higher rates of complications, such as elevated intraocular pressure and corneal edema (285). The advantage of silicone oil is that it is not position-dependent like a gas bubble, so it can be better for noncompliant patients or children. Vision is better through oil than gas; however, silicone oil must be removed surgically following treatment once the retina is deemed stable.
References:
The superior oblique is the only nerve innervated by cranial nerve IV, the trochlear nerve. The purpose of the superior oblique is to abduct, depress, and internally rotate the eye depending on its position. A CN IV palsy affecting the SO restricts these actions, causing a characteristic “head tilt” in pictures because the patient’s eyes only align when the head is tilted to the side.
Review this case for detailed discussion of diagnosis and management of trochlear nerve palsies.
Superior oblique overaction results in a vertical incomitance in lateral gaze. For SOOA, there is overdepression and intorsion of the adducting eye. In down gaze, there is an “A” pattern strabismus, in which the eyes are misaligned in downgaze (focusing on two points, like the two separate points at the bottom of the A). Treatment consists of surgically weakening the super oblique muscle, which eliminates the gaze incomitance (170).
The superior rectus is innervated by the superior division of the cranial nerve III, the oculomotor nerve, and is responsible for superior gaze.
Subretinal fluid refers to the accumulation of fluid in the subretinal space between the retina and the retinal pigment epithelium (see RPE). The subretinal fluid can come from a multitude of sources, but most commonly comes from the vitreous following a tear in the retina, causing a rhegmatogenous retinal detachment (RRD). Subretinal fluid changes distribution with changes in eye position and is affected by gravity, so that in the upright position, subretinal fluid accumulates under the inferior retina and vice versa. This can be important depending on the location of a retinal tear and will continue to be relevant in therapy if a vitrectomy with gas bubble is used to treat it.
SRF can be seen in cases of wet AMD, CSR, CRVO, among many others.
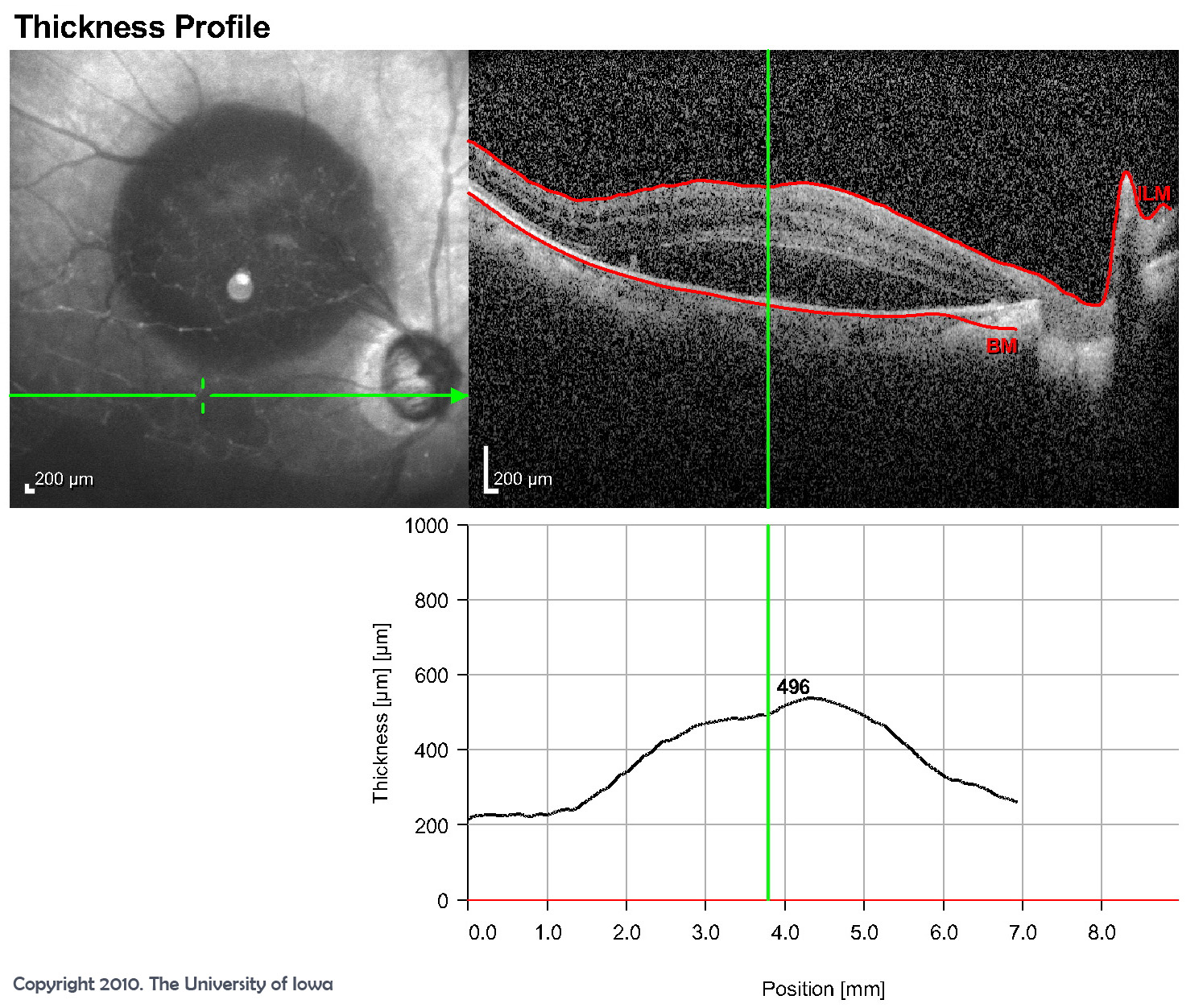
References:
Subretinal hyperreflective material refers to the presence of a bright signal on optical coherence tomography (OCT) in the subretinal space. This is an important aid in the diagnosis of neovascular age-related macular degeneration, as it can visualize the neovascular proliferation and give an idea of the prognosis (286).
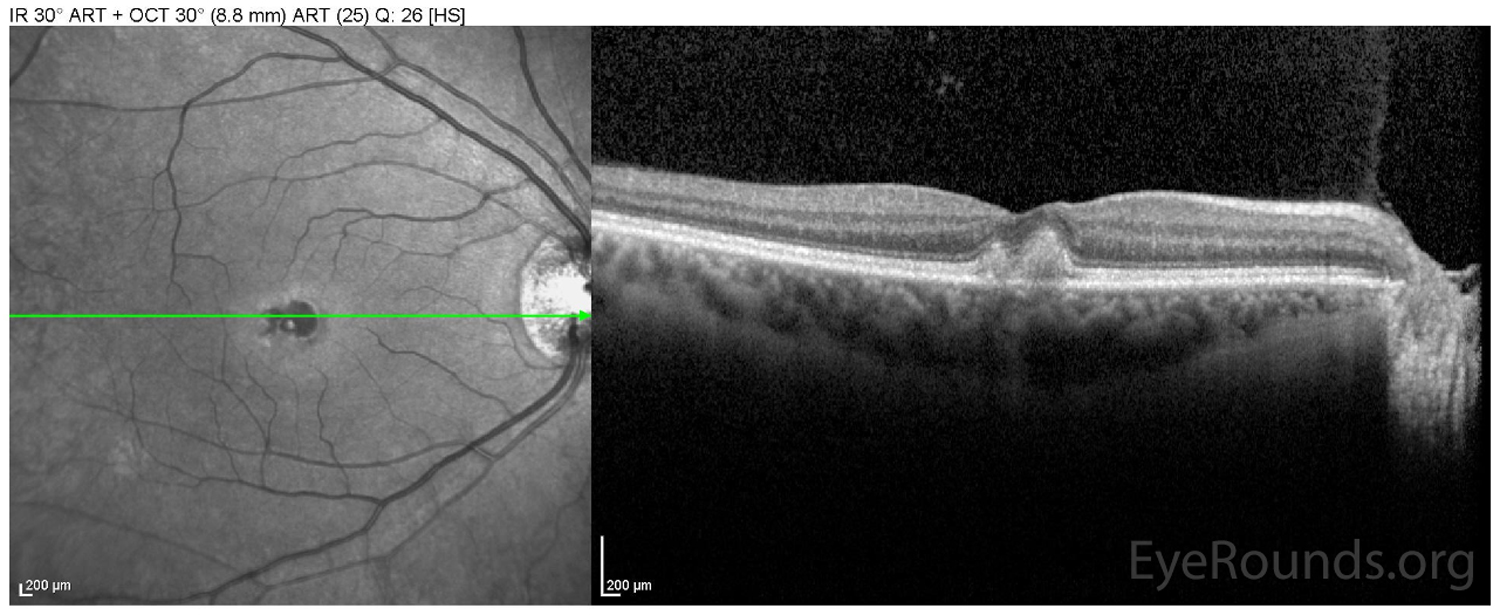
The scleral spur is the collagenous protruding portion of the sclera into the anterior chamber of the eye. It is attached posteriorly to the longitudinal ciliary muscle fibers and anteriorly to the trabecular network. It forms a ring, although on cross section it appears as a wedge shape like a spur. The scleral sulcus, where Schlemm’s canal lies, is formed at the edge of the scleral spur at the iridocorneal angle. A shorter scleral spur is associated with a higher risk of collapse of Schlemm’s canal and development of primary open-angle glaucoma.
A subtenons kenalog injection involves injecting Kenalog, a corticosteroid, underneath Tenon’s capsule, which is a dense fibrous tissue layer surrounding the eye and extraocular muscles (288). This technique allows for targeted delivery of corticosteroid to treat uveitis.
Tonometry by applanation is a method for measuring intraocular pressure (IOP). It involves pressing a probe against the eye and measuring the force it takes to flatten an area of it, which is equivalent to the IOP. A topical anesthetic is applied to the eye first for the patient’s comfort and quality of the exam. Goldmann tonometry is the gold standard for measuring IOP and is a version of tonometry by applanation.
The technique for performing Goldmann applanation can be reviewed here.
Tuberculosis is a highly communicable disease caused by the bacteria mycobacterium tuberculosis. It is spread person to person by air droplet. An infected person may either exhibit active TB with symptoms such as cough, hemoptysis, dyspnea, unintended weight loss, fatigue, night sweats, fever, loss of appetite or latent TB with no symptoms. Latent TB can turn into active TB, which makes surveillance and education important in patients with latent TB. The CDC recommends that people who are immunosuppressed, are from underdeveloped countries, use IV drugs, or are at high risk for coming in contact with infected individuals (in prisons, nursing homes, & in health care) should be regularly screened for TB. Between 3.1-5% of the U.S. population has latent TB, and without treatment, 5-10% will develop active TB in their lifetime.
References:
Thyroid eye disease is an autoimmune disease resulting from CD4+ T cells expressing Th1 cytokines and affecting orbital fibroblasts to secrete pro-inflammatory cytokines. It is most commonly associated with Graves’ disease but it can also occur with other thyroid dysfunction such as Hashimoto’s thyroiditis and even in the absence of thyroid dysfunction. The characteristic proptosis, or bulging of the eye, is caused by orbital inflammation leading to interstitial edema, adipose tissue genesis, and enlargement of extraocular muscles. TED can present with a variety of symptoms including edema in and around the orbit, exophthalmos/proptosis (protrusion of the eyes), eyelid retraction, exposure keratopathy (ocular dryness and redness), and eyelid lag in downgaze. This will generally manifest as the patient having large, protruding eyes. Treatment includes managing the underlying thyroid dysfunction and corticosteroids (289).

References:
Tear film breakup time is a test used in evaluating dry eye syndrome (see DES). It involves placing fluorescein dye on the patient’s eye and observing the time it takes for dry spots to appear on the eye. During this, the patient must refrain from blinking. In a normal eye, the tear film breakup time should be over 10 seconds, but in patients with evaporative dry eye disease, the tear film will break up before 10 seconds and cause the symptoms of dry eye.
TID is a common abbreviation generally referring to medications that should be taken three times a day.
Composed of endothelial-like cells and connective tissue, the TM is located immediately posterior to the corneal endothelium. It serves as a sieve to absorb aqueous humor, which then collects in Schlemm’s canal for drainage to the episcleral venous system. There are non-pigmented and pigmented regions of the TM, as shown in the below gonioscopy video and drawing.
Pathology of the TM: Axenfeld-Rieger syndrome, Grant syndrome, iridocorneal endothelial syndrome, melanocytoma of the iris and ciliary body, neovascular glaucoma, pigmentary glaucoma, plateau iris, pseudoexfoliation syndrome, among others
References:
Topiramate (Topamax) is an anticonvulsive drug used to treat seizure disorders, mood disorders and post-traumatic stress disorder. It is also prescribed for preventative treatment of migraine headaches and to treat alcohol dependence. In rare circumstances in adult and pediatric patients, during the first 1-2 months of treatment, this drug can cause acute myopia and pain associated with secondary angle closure glaucoma. Ophthalmologic findings include ocular redness, anterior chamber shallowing, myopia and increased IOP. Visual field defects have also been reported with TMX independent of increased IOP.
References:
Tonometry by tonopen involves using a tool called the Tono-Pen to evaluate intraocular pressure. While tonometry by applanation requires a tester trained to administer and evaluate the test, the Tono-Pen is much simpler to use and only requires the pen itself rather than a large device. The downside to Tp is that it is less accurate than tonometry by applanation, so an abnormal Tono-Pen intraocular pressure should be rechecked by applanation in an ophthalmology clinic.
The technique for performing tonometry can be reviewed here.
Trace refers to a very small quantity of something. For example, “trace cells in the anterior chamber” means that some cells can be visualized. This usually refers to one to five cells per high powered field (HPF).
Trabeculectomy is a surgical procedure to create an alternate outflow path for aqueous humor, bypassing the obstructed trabecular network in glaucoma treatment. This is typically performed after topical medication treatment and/or laser trabeculoplasty have inadequately controlled normalizing intraocular pressure. A fistula (hole) is created in the sclera with an overlying scleral flap to allow aqueous humor to escape in a controlled manner, thus lowering the intra-ocular pressure. Mitomycin C is used during surgery as an antifibrotic medication to prevent scarring of the subconjunctival space.
References:
Tractional retinal detachment is the second most common type of retinal detachment after rhegmatogenous RDs. It is a severe complication, usually associated with proliferative diabetic retinopathy, causing retinal traction and separation due to the presence of tractional membranes. This traction can lead to retinal breaks, retinal ischemia, and vision loss if not treated surgically. Vitrectomy surgery is indicated for TRD < 6 months duration involving the macula and progressive TRD threatening the macula. Chronic (> 6 months) TRD involving the macula may also benefit from surgery but the visual prognosis remains guarded.
The goal of care is to treat the underlying proliferative retinopathy before it becomes severe enough to cause a TRD; this often requires managing the underlying diabetes and using therapies such as panretinal photocoagulation or injection of anti-vascular endothelial growth factor through the pars plana region (290).
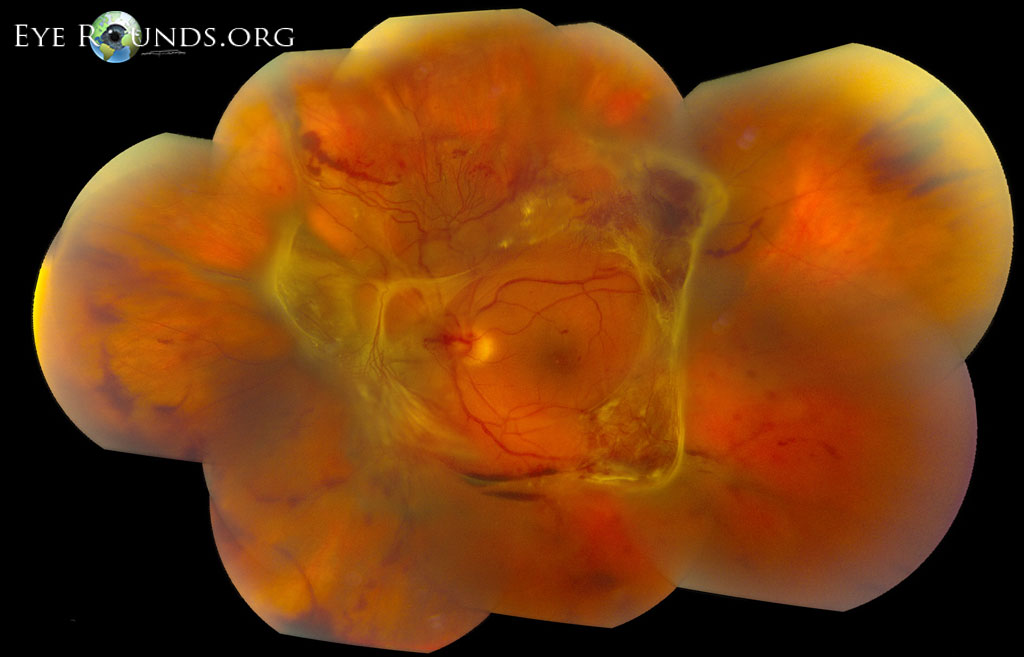
References:
A urinalysis is a laboratory test of a urine sample that checks the urine appearance, concentration, and content of the urine. A UA can check pH, specific gravity, protein, glucose, ketones, bilirubin, nitrites, leukocyte esterase, and a microscopic exam of cells if indicated.
For example, presence of nitrites, leukocyte esterase, WBC’s and bacteria may indicate a urinary tract infection (UTI). Increased protein with trace RBCs can be present in nephrotic syndromes, while RBCs and RBC casts with some protein may indicate nephritic syndrome. The presence of glucose or ketones suggests diabetes mellitus, and other findings may help in the diagnosis of other diseases. Overall, urinalysis is done to screen for disease, diagnose a medical problem, and monitor certain medical conditions.
UA is commonly ordered in the work-up of certain ophthalmic diseases, including TINU, TTP-HUS, and C3 glomerulopathy, among others.
Uveitis-glaucoma-hyphema syndrome is characterized by pigment dispersion and blood in the anterior chamber in eyes with a mispositioned artificial lens. If the artificial lens is misplaced over the iris, ciliary body, or iridocorneal angle, it can cause continual mechanical trauma. This trauma causes chronic inflammation as well as the characteristic hyphema, or blood in the anterior chamber. Additionally, this can cause dispersion of pigment which elevates the intraocular pressure through blocking aqueous humor outflow through the trabecular meshwork, as seen in pigmentary glaucoma. The incidence of UGH has gone down over time with innovations in lens design and surgery techniques (292).
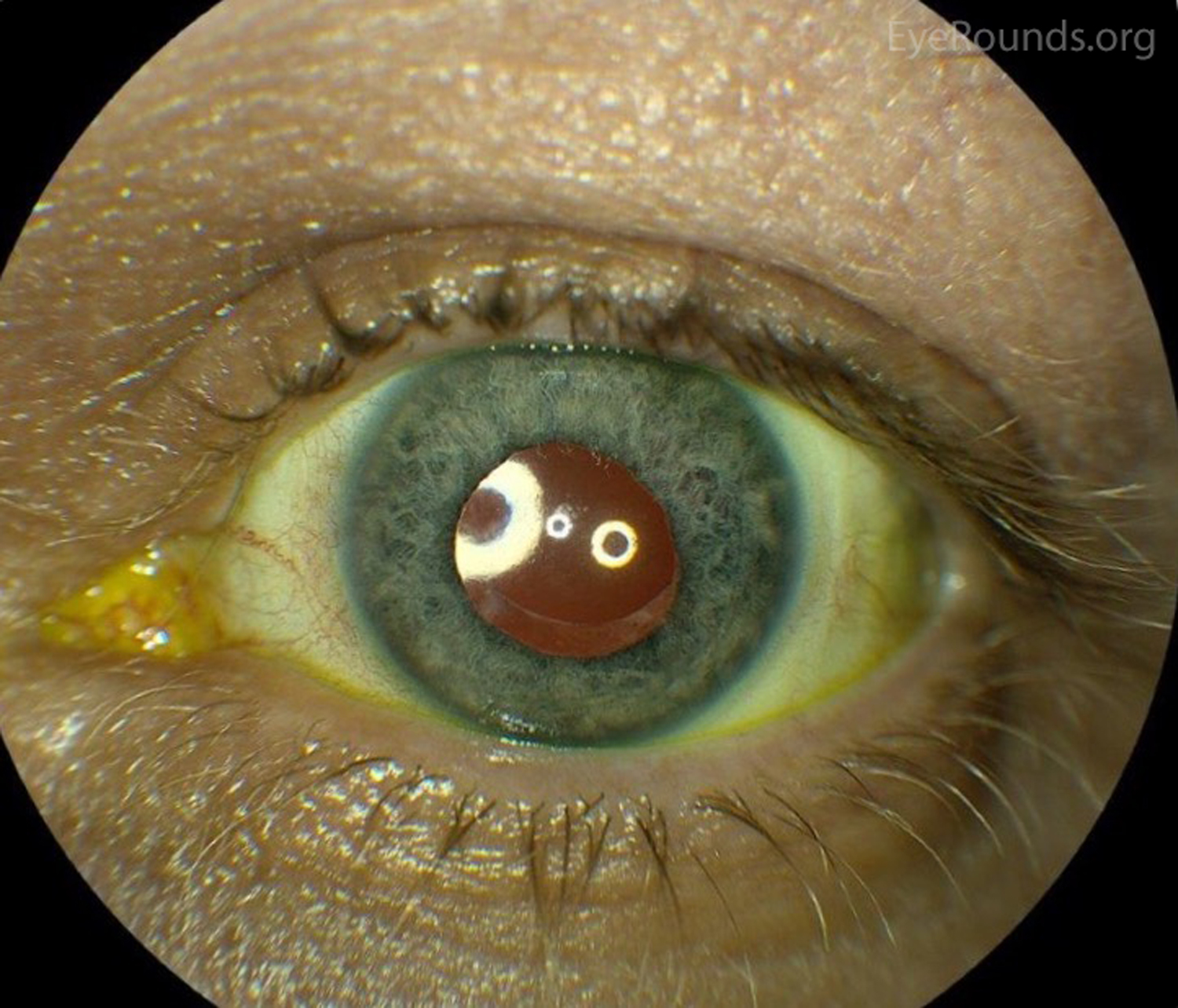
References:
In ophthalmology, ointment is a mixture of neomycin, polymyxin, and bacitracin. This is used as a topical for superficial bacterial eye and eyelid infections.
Visual acuity is a measure of clarity of vision and is dependent on the function of the retina, the eye’s ability to focus the image, and the neurological interpretation of the image by the brain. It is measured by testing the ability to read the smallest letters on a standardized chart (Snellen chart) 6 meters away. Vision can also be tested by a Snellen pocket chart from 14 inches away for a more convenient exam that doesn’t require a longer hallway but at the cost of being less accurate. Vision should be tested in each eye independently and with both eyes together to ensure a quality examination.
References:
Vascular endothelial growth factor is a signaling molecule released from hypoxic tissues to signal that an area of the body needs increased blood flow. In oncology, anti-VEGF therapy helps to stop tumors from growing new blood vessels and, therefore, starving them from oxygen and inhibiting their growth.
In ophthalmology, the primary use is for treating diseases that cause vascular proliferation in the retina, like proliferative diabetic retinopathy and wet age-related macular degeneration. These medications are delivered intravitreally by injection through the pars plana region, which is an area of tissue between the retina and anterior structures of the eye (293).
Visual evoked potential testing evaluates the integrity of the afferent visual pathway between the optic nerve and the occipital cortex of the brain. A light stimulus is given to the patient, which is converted into a neurologic impulse that is sensed by an electroencephalogram over the occipital cortex. The waveform peaks can then be analyzed for amplitude and latency of onset of the peak after the light stimulus. The usefulness of an abnormal VEP can be limited without an obvious cause of pathology because numerous factors in the pathway could be causing the problem. However, a normal VEP confirms that the visual pathways are intact. VEPs are generally useful for evaluating visual pathways in inarticulate adults and infants and for confirming intact visual pathways in patients who may have nonorganic disease.
References:
The visual field is the full area in which a person can see. The field of vision in each eye extends about 60 degrees nasally, 90 degrees temporally, 60 degrees superiorly, and 70 degrees inferiorly. Visual fields can be tested through confrontation (counting fingers), Goldmann kinetic perimetry, or Humphrey field testing (HVF). Evaluation of visual fields is important in various diseases but especially so in glaucoma, where changes in visual field can give an idea of disease progression (294).
References:
Vitreous hemorrhage is the abnormal presence of blood in the vitreous cavity. The three most common causes are proliferative diabetic retinopathy (see PDR), posterior vitreous detachment (see PVD), and ocular trauma. Symptoms can include sudden painless hazy vision or vision loss, new floaters, or even a red tint to vision. This can be accompanied by photopsias (flashes of light in peripheral vision) due to traction on the retina. The prognosis depends on the underlying etiology, as continued bleeding will cause more severe disease. In some cases, VH clears over time with conservative measures and prognosis is good for regaining baseline visual acuity. Patients with diabetic retinopathy or AMD have worse prognoses and are often treated with intravitreal drug injections and laser panretinal photocoagulation (PRP) treatments. Vitrectomy is also a good option for patients who have VH refractory to conservative therapy, significant hemorrhage, or comorbidities like retinal vein occlusion and retinal tear (295).
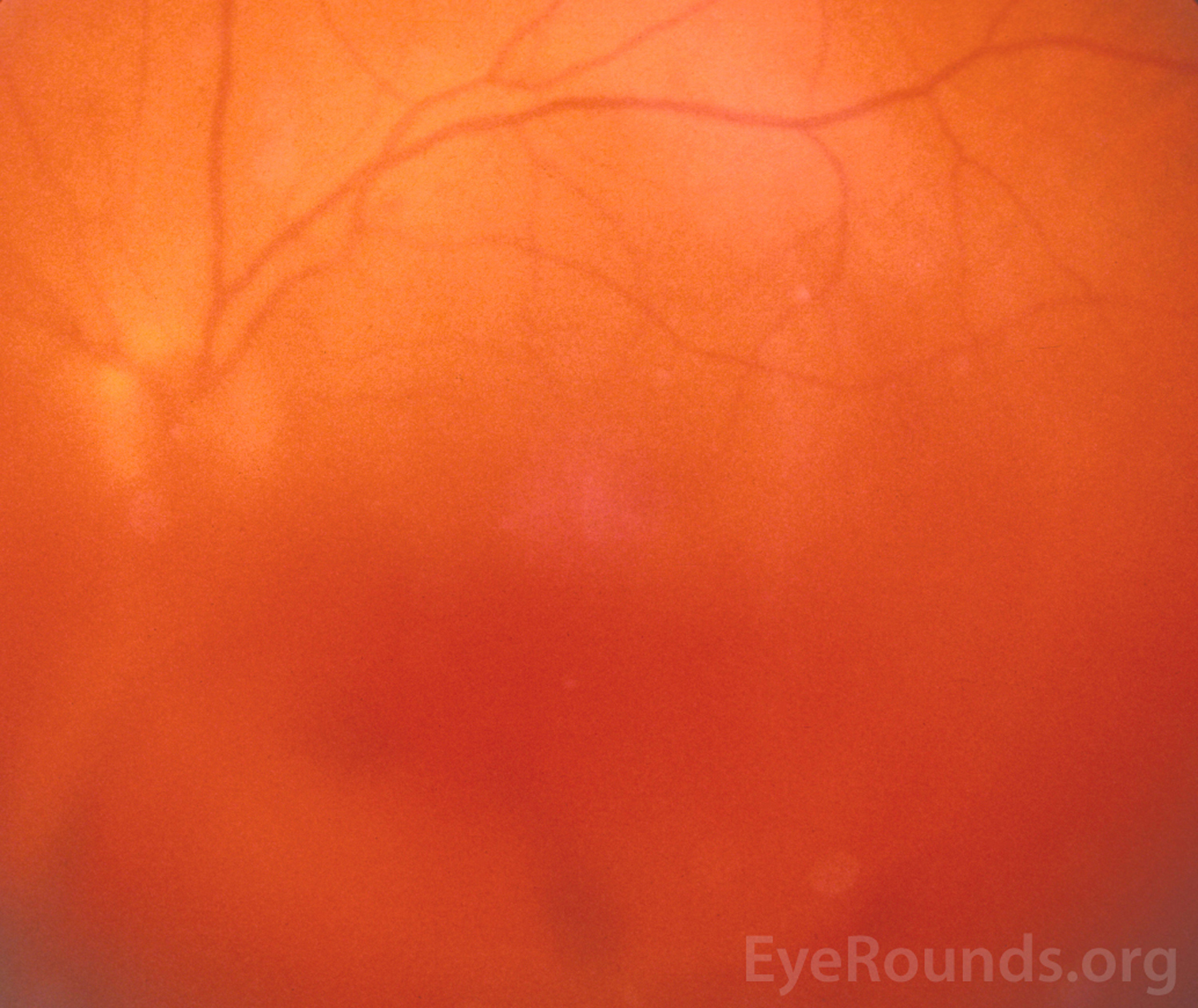
References:
Von Hippel-Lindau is a genetic disease involving the VHL gene on chromosome 3 that causes tumor growth at various places on the body, the most common of which is a hemangioblastoma. Hemangioblastomas are tumors made from blood vessel tissue, and while they are typically noncancerous they can still cause problems depending on their location in the body. One particularly dangerous location they can grow is within the eye, which happens when retinal capillary hemangioblastomas form. Treatment can involve laser or cryotherapy, but can involve radiation and even enucleation in very severe cases (296).
References:
Vernal keratoconjunctivitis is a severe, seasonal, sight-threatening allergic eye disease occurring primarily in children, causing inflammation of the cornea and conjunctiva. It is more common in male children with a history of allergies, asthma, or atopic dermatitis. In children of African or Asian descent, limbal VKC is the most common type.
VKC Symptoms include severe itching, tear production, thick ropy discharge, photophobia, and conjunctivitis. Treatment begins with topical antihistamines and frequently topical corticosteroids are required for flares. Complications include corneal ulcers/scars, and corticosteroid complications include increased IOP, glaucoma, cataract and infection. Immunomodulators such as cyclosporine and tacrolimus are an alternative therapy for VKC as a steroid-preserving agent due to the high side effect profile of corticosteroids (297). The high risk for severe complications and remodeling changes can lead to blindness for these children.

Vogt-Koyanagi-Harada is an autoimmune inflammatory eye disease characterized by severe bilateral granulomatous inflammation with serous retinal detachments, optic disk edema, and vitritis. Eventually the fundus develops an orange-red “sunset glow” appearance if treatment is delayed. VKH presents in 4 phases: prodrome, uveitic, convalescent, and recurrent. Extraocular symptoms can include headache, vitiligo, meningismus (meningitis like symptoms), hearing loss, and poliosis (whitening of a patch of hair).
Diagnostic of acute symptoms by optical coherence tomography (OCT) shows exudative detachments of the retina and choroid thickening, which eventually leads to choroid thinning. Treatment is with systemic corticosteroids initially, then transitioning to immunomodulatory medication like cyclosporine or methotrexate for maintenance therapy. Studies have shown that treating VKH with corticosteroids for greater than 6 months results in better ocular outcomes than those treated for a lesser duration, with steroids plus steroid-sparing agents also showing good outcomes (299).
Please review the VKH case for more information about pathophysiology, diagnosis, and management.
Venolymphatic malformations are abnormal connections of the venous and lymphatic system. They are associated with other vascular abnormalities and are a fairly common source of orbital masses at 4% (300). These connections result in lymphatic cysts with an endothelial lining. These cysts can suddenly enlarge in the context of hemorrhage or infection, which can lead to ptosis and proptosis as well as other symptoms depending on the location of the lesion. Surgery is generally required to fix problematic lesions.

References:
Vitreomacular traction is caused by vitreomacular adhesions from a detaching posterior vitreous. The traction from the detaching vitreous pulling on the retina may cause edema seen on fundoscopic exam and on optical coherence tomography (OCT). The patient may present with blurred vision and metamorphopsia (visually distorted lines/shapes) in one eye.
Spontaneous resolution can occur in 20% of cases without other ocular comorbidity, but in most cases VMT persists with risk of developing a membrane on the surface of the retina that can cause further traction on the retina or a macular hole, both of which require surgical intervention. One study examining outcomes of VMT found that pars plana vitrectomy was an effective treatment in patients with worsening VMT and that watchful waiting wasn’t always appropriate as many patients do not spontaneously improve (301).
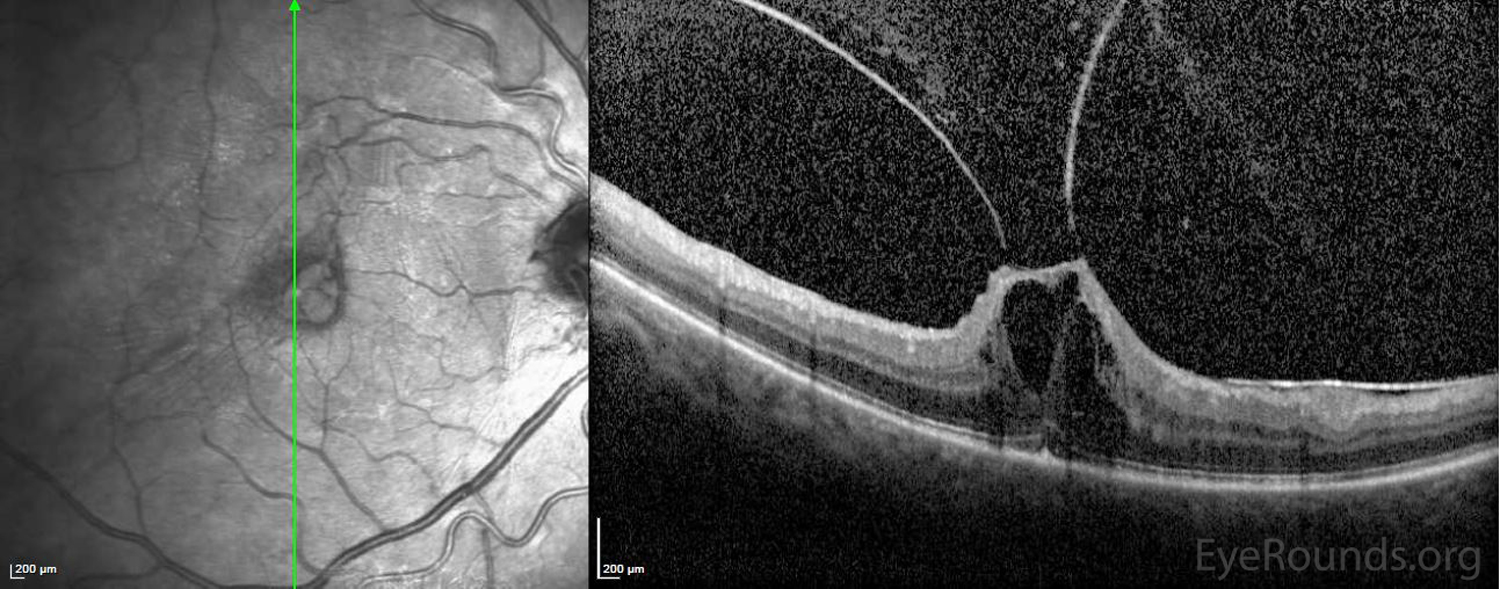
References:
Venereal disease research laboratory test is a test for syphilis, which is caused by Treponema pallidum. It is a serologic screen with a high sensitivity but poor specificity, so follow-up tests are required for definitive diagnosis. Syphilis can be a cause of uveitis and other ocular disease, so VRDL is an important test for a patient with risk factors for syphilis.
Laboratory testing for syphilis involves two types of assays: non-treponemal and treponemal. The non-treponemal tests, such as rapid plasma regain (RPR) and Venereal Disease Research Laboratory (VDRL) become negative after treatment. The treponemal tests, such as Treponema pallidum particle agglutination assay (TPPA) and FTA-ABS, are more sensitive and more specific, but they remain positive for life (148).
References:
Varicella zoster virus is the virus that causes chicken pox and shingles. It is a herpes virus that becomes latent in cranial nerve ganglia or dorsal root ganglia after an initial infection. When varicella becomes latent in the ophthalmic division of the trigeminal nerve, it causes a syndrome called herpes zoster ophthalmicus upon reactivation. This is an unfortunately common syndrome that causes extreme pain and is considered an ophthalmologic emergency as it can threaten vision and cause chronic pain (302).

References:
Worth 4 dot is a test to evaluate a patient’s binocular vision, or the ability of the eyes to fixate on an image together. This comes into play in the evaluation of strabismus (misalignment of the eyes), amblyopia (failure of one eye to reach normal visual acuity), and aniseikonia (a difference in perceived size of images). The patient wears a set of binoculars with a red lens over one eye and a green lens over the other and looks at a set of lights, which should take on a diamond appearance if they can visualize all four. If the patient primarily uses one eye because of an issue with the other, then they will fail to visualize all four dots.
Suppression of one eye and W4D testing is explained well using this case of monofixation syndrome.
This abbreviation indicates the corresponding action or therapy should be done while the patient is awake.
White blood cells are the immune cells of the body which can be measured on a complete blood count (CBC). WBC types include granulocytes (neutrophils, eosinophils, and basophils), monocytes, and lymphocytes (B cells and T cells).
Warm compresses are the application of warmed moist heat for therapeutic treatment of injured tissue. It aids in local tissue vasodilation and improved blood flow, which can aid in reabsorption of fluid from swollen tissue. For ophthalmology, warm compresses are mostly used for dry eye to aid in expression of meibomian gland secretions which help keep the eye lubricated.
Please review this comprehensive evaporative dry eye tutorial to learn more about dry eye diagnosis and management.
Exophoria refers to an abnormal tendency for one eye or both eyes to drift outward. This is a common finding in infants and children and should be worked up as it can have multiple etiologies. Exophoria is often elucidated through alternatively covering the eyes, during which one will visualize a tendency for an eye not currently fixating to deviate outward. This can be treated through glasses with a prism to help focus the image the same on both eyes or through exercises to train the eyes. Surgery can be used, but is rarely needed for exophoria as it is generally less severe than exotropia.
Exophoria at near is a more specific type of exophoria that happens when attempting to fixate on a nearby object. This is called convergence insufficiency and is typically treated with visual exercises to train the eyes to fixate together. Treatment can take several months and patients may experience headaches and difficulty reading in the meantime.
Intermittent exotropia at near is a further defined version of intermittent exotropia, a form of incomitant strabismus. When attempting to fixate on a near object, one or both of the eyes will turn outward. This is also a form of convergence insufficiency and is treated through visual therapy exercises that slowly train the eyes to fixate on a near object. Surgery may be an option if a muscular problem can be identified. Minus lens therapy is also an option as with intermittent exotropia by stimulating the eye to turn inward by wearing glasses that induce the eye to overcorrect inward to compensate for the glasses.
Intermittent exotropia is a form of incomitant strabismus in which the eyes can successfully align and focus together sometimes, but not at other times. In intermittent exotropia, at certain angles of gaze or under certain conditions, one or both eyes will deviate outward. This is generally considered to be a problem with the extraocular muscles. Patching can help treat this by training the extraocular muscles and surgery is also an option to correct abnormal muscles (303). Minus lens therapy is also an option in which overcorrected glasses induce the eye to turn inward to compensate for the overcorrected lens.
Exotropia is a misalignment of one eye or both eyes that causes deviation outward. It is more severe than exophoria and will be visible without needing an alternate cover test. If one eye is affected and not treated, it can develop into amblyopia (a lazy eye) later in life because the misaligned eye will fail to develop and reach peak visual acuity due to the lack of stimulation. Treatment can consist of patching to force use and stimulation of the affected eye or surgery to correct the deviation if possible. Glasses with a prism are also an option to bend the image onto the eye despite the deviation, causing both eyes to focus the image the same way.
Neodymium-yttrium aluminum garnet is a crystal used in solid state lasers as a lasing medium, delivering infrared waves in high-intensity pulsed or continuous modes. Applications in ophthalmology for using the Nd:YAG laser include but are not limited to iridotomy to treat acute angle-closure glaucoma, laser capsulotomy to treat posterior capsular opacification, photocoagulation treatment of diabetic retinopathy, and use in selective laser trabeculoplasty for glaucoma.