Chief Complaint: Blurry vision and discomfort in the right eye (OD).
History of Present Illness: A 12-year-old female complains of blurry vision, foreign body sensation, and photophobia in her right eye. While she has had chronic problems for years in both eyes, she has noted the acute onset and progressive worsening of the symptoms in the right eye for one week.
Past Ocular History: Since the age of 6, the patient has struggled with meibomian gland dysfunction and chronic staphylococcal blepharoconjunctivitis, as well as seasonal allergic conjunctivitis. She has been treated with topical corticosteroids, antibiotics, and antihistamines since age 8 and systemic doxycycline since age 9.
Medical History: Otherwise healthy.
Medications: Since her last exam 8 months prior to this presentation, she was completely asymptomatic on a regimen of:
The patient had discontinued all of these systemic and topical medications one month prior to the current episode upon the suggestion of a maternal aunt who recommended adoption of a "holistic and naturalistic" approach to the managment of her chronic ocular disorders.
Family History: Noncontributory
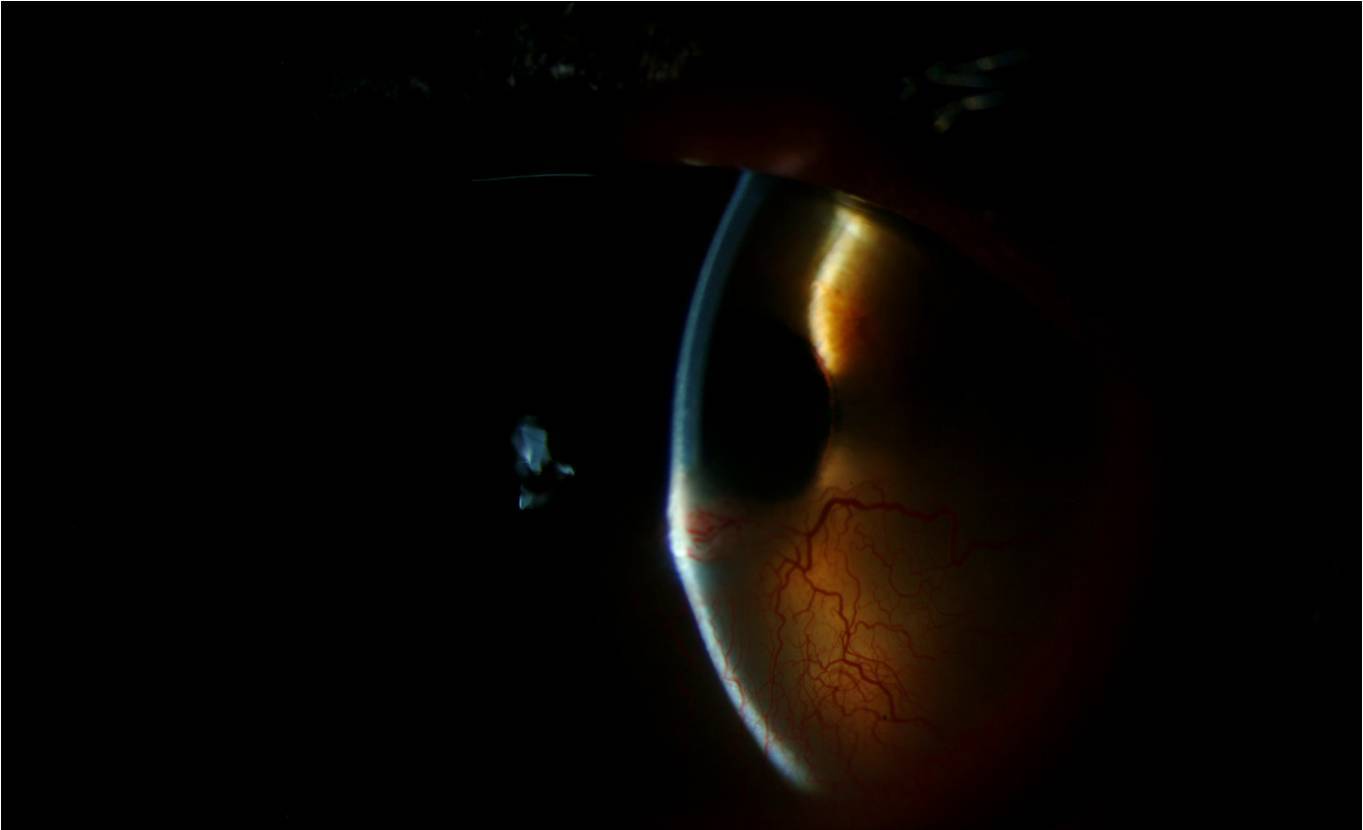
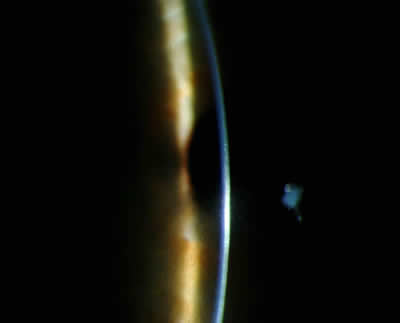
| Figure 1A: Right Eye external exam exhibits | Figure 1B: External exam, elevated yellow nodule. |
 |
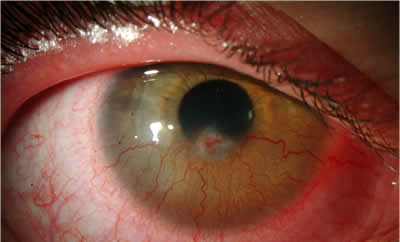 |
| Figure 1C: Anterior Segment Exam | Mild anterior blepharitis with diffuse conjunctival injection. The cornea shows a 1x1 mm elevated yellow nodule with central erosion and fluorescein uptake with surrounding engorged hyperemic vessels, slightly inferior to the visual axis. |
 |
| Figure 2A: External Exam. Left eye. | Figure 2B: External Exam of left eye shows mild anterior blepharitis |
 |
 |
Discussion: Phlyctenular keratoconjunctivitis (PKC) is a localized noninfectious inflammatory/ hypersensitivity disorder of the ocular surface characterized by subepithelial nodules of the conjunctiva and/or cornea. These "phlyctenules," are derived from "phlyctena," the Greek word for "blister." The blister characterization was likely chosen due to the tendency for the nodules to ulcerate once necrosis occurs. Histopathologically, phlyctenules are subepithelial inflammatory nodules containing histiocytes, lymphocytes, plasma cells, and neutrophils. Mononuclear phagocytes, dendrites Langerhans cells, and neutrophils make up the majority of the inflammatory cells in the epithelium overlying the phlyctenule.
The pathogenesis of PKC is thought to be a hypersensitivity reaction to an antigen of bacterial origin. PKC has been classically associated with M. tuberculosis (especially in developing countries). However, Staphylococcus aureus is the cause in majority of cases in the United States. A number of other organisms are also associated with PKC (Table 1).
|
Most often, phlyctenulosis is a corneal sequelae of chronic Staphylococcal blepharitis, a disorder that often presents in the clinic as chronic conjunctivitis or keratitis characterized by punctate epithelial keratopathy, and/or marginal corneal infiltrates (Table 2). When present, symptoms of PKC depend upon the location of the lesion. Conjunctival lesions usually present with mild to moderate symptoms, including foreign body sensation, tearing, photophobia, burning, and itching. Corneal lesions typically present with more severe symptoms of the same variety.
Corneal phlyctenules usually begin at the limbus and spread centrally, perpendicular to the limbus, leaving no clear zone between the lesion and the limbus. The vessels run in a straight course from the limbus. They can become necrotic and ulcerate centrally or spontaneously involute within 2 to 3 weeks. Upon resolution, a wedge-shaped fibrovascular scar may remain. Centripetal migration of successive inflammatory lesions may develop as in this case. Rarely, inflammation associated can lead to keratolysis and perforation.
Treatment: Management of PKC requires both anti-inflammatory and anti-bacterial management, as well as management of chronic blepharitis. Control of inflammation can be achieved with topical corticosteroids, which should be tapered very slowly to avoid recurrences. Antibacterial measures may include a several week course of application of topical antibiotics to the eyelid margin and conjunctiva, especially at bedtime. Management of chronic blepharitis requires a consistent regimen of lid hygiene and warm compresses, as well as systemic administration of tetracycline derivatives, such as Doxycycline for patients without contraindications. Tetracyclines should not be used in children under age 8 because permanent tooth discoloration can occur. In addition, tetracycline is teratogenic and should be avoided in pregnant women, as well as in nursing mothers.
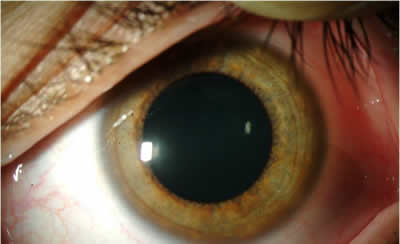
Follow-up Course: Our patient responded dramatically to topical prednisolone acetate 1% which was initially used every 2 hours while awake. She was treated with a 1 week course of topical gatifloxacin drops four times daily (to prevent infection at the epithelial defect) and a 3 week course of TobraDex® ointment at bedtime. Management of chronic blepharitis was achieved by reinstating a strict program of lid hygiene and warm compresses, along with reinstituting doxycycline 100 mg orally twice daily for one month and then once daily thereafter. Within 1 week, she responded readily to this treatment with improved vision and decreased discomfort (post-treatment images Figure 3A-D), after which topical corticosteroid therapy was gradually tapered.
| Figure 3A: Right eye, post-treatment | Figure 3B: Right eye, post-treatment |
 |
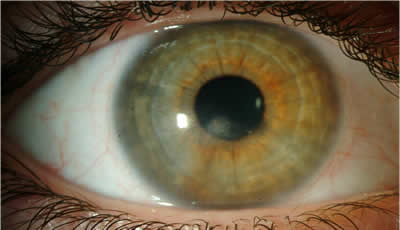 |
| Figure 3C: post-treatment | Figure 3D: post-treatment anterior eye exam. |
 |
 |
Diagnosis: Phlyctenular keratoconjunctivitis
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
1. Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. 2nd ed. Philidelphia: Saunders; 2000. p. 1093-1099.
4. Krachmer JH, Mannis MJ, Holland EF, eds. Cornea. 2nd ed. Philadelphia: Elsevier Mosby; 2005. p. 1235-1238.
5. Rapuano CJ, Luchs JI, Kim T. Anterior Segment: The Requisites in Ophthalmology. St. Louis: Mosby; 2000. p. 165-168.
Wagoner MD, Bajart AM, Allansmith MR. Phlyctenulosis. In: Fraunfelder FT, Roy FH Current Ocular Thearapy 3. Philadelphia, PA; W.B. Saunders Co. 1990. p. 454-445
Muthialu A, Jensen LE, Wagoner M. Phlyctenular Keratoconjunctivitis: 12-year-old Female with Staphylococcal Blepharitis. EyeRounds.org. February 27, 2009; Available from: http://www.eyerounds.org/cases/89_Phlyctenular-Keratoconjunctivitis-Staphylococcal-Blepharitis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.