Chief Complaint: Mild bilateral eye irritation.
History of Present Illness: A 64-year-old gentleman who was referred to the Oculoplastics Service at the University of Iowa for longstanding irritation of both eyes. He was recently treated for "blepharitis" and allergic conjunctivitis. Despite using olopatadine (Patanol) drops and lid hygiene, his symptoms persistented. Prior ophthalmic examination revealed two rows of eyelashes on his lower eyelids bilaterally and bilateral punctate epithelial erosions (PEE). The patient reports that he was aware of his extra eyelashes, and that they had been there as long as he could remember.
Ocular History: Blepharitis, ocular hypertension, and allergic conjunctivitis. No history of ocular trauma or infection.
Medical History: Non-insulin dependent diabetes mellitus, hyperlipidemia, and hypertension.
Medications: olopatadine (Patanol), dorzolamide/timolol (Cosopt), simvastatin (Zocor), gyburide, and lisinopril.
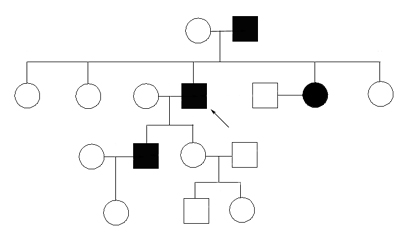
Family History: The patient's father, son, and at least one sister also have two rows of eyelashes (see Figure 1). He is not sure about his other sisters and is unaware of any other health problems affecting family members.
Social History: The patient is married. He is a smoker and recently retired
 |
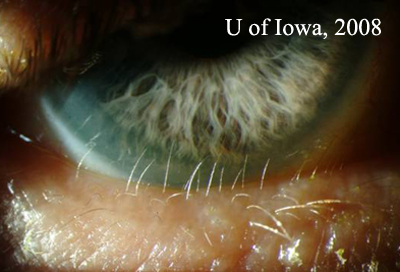
| Figure 2A: Slit lamp photograph of patient's left eye. Two rows of lashes are seen. The anterior row is normal and in proper position. There is an extra, more posterior row of fine, lightly pigmented lashes adjacent to the cornea and bulbar conjunctiva. | Figure 2B: Higher magnification slit lamp photography of extra row of lashes. Note the proximity to the inferior cornea. |
 |
 |
Course: The patient was diagnosed with distichiasis. Multiple options for treatment were considered and discussed with the patient (see Treatment below). The patient decided to proceed with surgical correction of his distichiasis. Treatment consists of a lower eyelid splitting procedure followed by cryotherapy of the posterior lamella (see Figure 3).
 |
Discussion: A normal eyelid has a single row of eyelashes located along its anterior margin. The posterior portion of the lid contains a row of Meibomian glands, which secrete the oily component of the tear film. Distichiasis refers to the condition in which there is an extra row of lashes. These lashes are present on the posterior edge of the lid margin in place of the Meibomian glands. This results from aberrant differentiation of basal epithelial cells into hair follicles instead of Meibomian glands. Distichiasis can be congenital or acquired, and can affect a single eyelid or all four lids. The abnormal lashes tend to be fine and lightly pigmented, but can be just as coarse and pigmented as normal eyelashes. Because these lashes line the posterior lid margin, they are often closely apposed to the globe and can cause chronic irritation, which can lead to corneal epithelial defects, corneal scarring, astigmatism, and even keratoconus.
Most cases of distichiasis are congenital. Congenital distichiasis is almost always associated with the Lymphedema-Distichiasis (LD) syndrome. As the name implies, the syndrome consists of a double row of eyelashes and lymphedema. Lymphedema is a chronic, often debilitating, swelling of the extremities that does not typically present until after puberty. Lymphedema-Distichiasis is an autosomal dominant condition, which has been mapped to the FOXC2 gene at 16q24.3. LD syndrome exhibits incomplete penetrance and marked variability of expression. Because of this, different individuals with the same mutation may exhibit varying phenotypes. Either lymphedema or distichiasis may be absent or mild, but distichiasis is almost always present. Over 35 different causative mutations have been found in the FOXC2 gene. The FOXC2 gene product is a transcription factor that is likely involved in a wide array of development processes. The majority of mutations found are nonsense mutations, which result in a truncated, nonfunctional gene product. LD syndrome is sometimes associated with other congenital abnormalities including ptosis, congenital heart defects, extradural spinal cysts, and cleft palate.
Acquired distichiasis is less common, and is seen in the setting of chronic inflammatory conditions of the eyelid such as blepharitis, ocular cicatricial pemphigoid, Steven Johnson syndrome, and following chemical injury. Acquired distichasis tends to be more symptomatic than its congential counterpart.
This patient's distichiasis also led to trichiasis. Trichiasis is misdirection of lashes toward the surface of the globe. The most widely observed causes of trichiasis include involutional lid changes, posterior lamellae scarring, epiblepharon, and distichiasis.
A variety of surgical procedures have been used to treat distichiasis. Most commonly, the eyelid is split along the gray line, which separates the eyelid into its anterior and posterior halves. After the lid is split, the abnormal lashes on the posterior lamella can be treated with a variety of procedures to remove the misdirected lashes without causing scarring to the normal lashes and anterior lamella. Procedures to remove the abnormal lashes include cryotherapy, trephination, epilation, and microhyfrecation. Lid splitting with cryotherapy is our procedure of choice.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Wendel LJA, Carter KD. Distichiasis: 64-year-old white male with bilateral eye irritation. EyeRounds.org. May 7, 2008; Available from: http://www.EyeRounds.org/cases/84-Distichiasis-Extra-Eyelashes.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.