Chief Complaint: Persistent red left eye (OS) for two weeks
History of Present Illness:The patient is an otherwise healthy 22-year-old African-American male who presented with a two week history of red left eye. He describes ocular discharge, mattering of eye lashes and a swollen upper eyelid. He was seen at Student Health and prescribed ciprofloxacin drops every four hours for suspected infectious conjunctivitis. When the redness and other symptoms did not resolve he was referred to the Ophthalmology Department at the University of Iowa for further evaluation and care.
Past Ocular History: Unremarkable for any past ocular surgery or trauma. No contact lens use.
Medical History: On review of symptoms, the patient describes prior episodes of recurrent erythema multiforme, predominantly affecting his acral surfaces and oral mucosa, which was treated with valacyclovir. He denies any history of sexually transmitted infections.
Medications: Valacyclovir 1000 mg daily and ciprofloxacin eye drops, every four hours, OS.
Family History: Non-contributory
Social History: The patient is a college student entering his senior year. He recently relocated to Iowa.
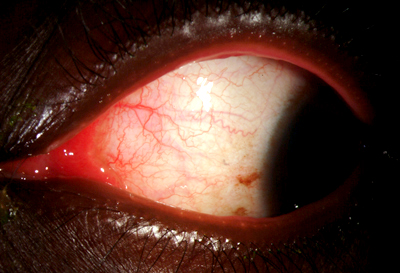
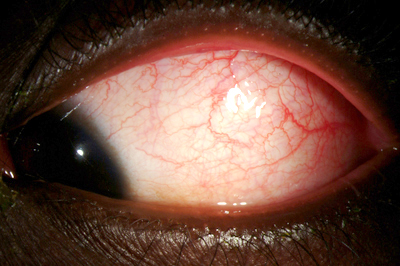
| 1A: Slit lamp view, OS. Note the conjunctival and episcleral injection as well as the inflammed plica semilunaris | 1B: Conjunctival injection, OS. Papillae were present on the tarsal conjunctiva. |
 |
 |
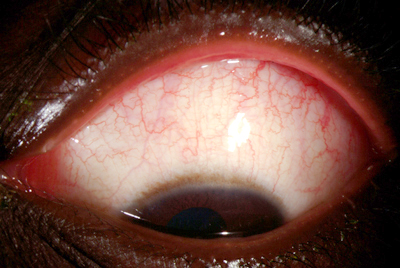
1C: Conjunctival injection noted in downgaze |
|
 |
Course: The patient was placed on topical prednisolone acetete 1% every 6 hours. At the one week follow-up appointment, he had resolution of his presenting symptoms and the topical steroid was tapered. Recognized and treated early, the lesions never progressed to the classic target lesions.
Discussion: Erythema multiforme (EM) is an acute, often recurrent, inflammatory disease characterized by the sudden onset of raised erythematous macules which rapidly progress to papules and then evolve into the classic target lesions. These lesions usually resolve spontaneously in one to four weeks. The dorsal and acral surfaces of the hands and feet and the extensor surfaces of the extremities are commonly involved. Approximately 70% of patients with EM have mucosal manifestations, frequently affecting the lips, buccal mucosa or tongue, and may involve the genitalia or conjunctiva. (Habif, et al. 2004).
EM is most prevalent during the third and fourth decades of life and has a slight male predilection. (Ogundele et al. 2006) Factors involved in the etiology of EM include antecedent upper respiratory tract infection, Mycoplasma infection, herpes simplex virus infection, and medication, including antibiotics, anti-seizure, anti-gout, and anti-inflammatory drugs. Recurrent EM is more commonly associated with drug reactions and herpes simplex virus infection. However, the precipitating cause is often not known. (Power, et al. 1995; Yi-Sheng Chang, et al. 2007)
Ocular manifestations occur in approximately 20% of patients with EM and are usually mild. Ocular findings include conjunctival injection, chemosis, eyelid edema, erythema, blepharitis and a watery to purulent discharge. More severe ocular manifestations of EM may include conjunctival membrane or pseudomembrane formation.
Ocular manifestations should be ruled out in every patient who presents with EM. Severe and prolonged ocular inflammation can lead to ocular sequelae, the most common being dry eyes. An inflammatory reaction involving the ocular surface may result in destruction of conjunctival goblet cells, leading to a decrease in mucin production and an abnormally short tear film break-up time. (Wilkins et al. 1992)
Treatment: Management is aimed at reducing ocular inflammation with topical steroids and hydrating the ocular surface with artificial tears and lubricants. Topical antibiotics may also be indicated if the ocular surface epithelium is compromised. Systemic corticosteroids have no effect on the incidence or severity of ocular manifestations.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Ames J, Fillmore PD, Oetting TA: Erythema Multiforme: 22-year-old male with a persistent red eye for two weeks. EyeRounds.org. August 20, 2007; Available from: http://www.EyeRounds.org/cases/73-Erythema-Multiforme-Red-Eye.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.