Chief Complaint: One week duration of central scotoma, OD.
History of Presenting Illness: The patient is an adult white female in her mid-twenties who experienced sudden awareness of a painless, central scotoma in her right eye while reading one week ago. There has been no pain or progression in the last week. There was no known trigger. She reports normal color vision. She denies headache. She denies preceeding viral illness.
Medical History: 1) An MRI six years previously showed enlargement of the pituitary gland with no focal adenoma. Endocrine evaluation showed normal pituitary function. 2) Motor vehicle accident, 1 year previously. No loss of consciousness. Computerized tomography (CT) without contrast was normal at that time. Other history was non-contributory.
Review of systems was otherwise negative except as noted.
Medications: Benzidine for acne. No steroid use.
EXAM OCULAR
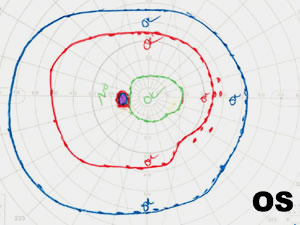
Goldman visual field (GVF) testing was performed and revealed a slightly enlarged blind spot and mildly reduced paracentral visual field overall, OD (see Figure 3).
 |
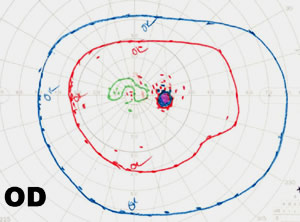 |
| 3A: GVF, OS, is essentially normal. | 3B: GVF, OD. Enlarged blind spot with reduction of the I1e isopter centrally. |
MEWDS (Multiple Evanescent White Dot Syndrome) is a rare, unilateral, self-limiting inflammatory disease that afflicts young women more than men in a 4:1 ratio. Despite the lack of treatment, the prognosis is excellent. Our patient is the typical age and gender. She had no preceeding viral illness, which can be present in approximately 1/3 of MEWDS patients. Visual field testing reveals enlargement of the blind spot, central, and/or paracentral scotomas. Fluorescein angiography of active lesions may be normal early on and demonstrate a "wreath-like" late hyperfluorescence of the white dots. ERG during the active phase may show a reduced a-wave, consistent with inflammation at the level of the photoreceptors. Typically, the visual acuity recovers, but the granularity of the foveal RPE remains.
EPIDEMIOLOGY
|
OCULAR SIGNS
|
SYMPTOMS
|
TREATMENT
|
Pramanik S, Beaver HA. Multiple Evanescent White Dot Syndrome (MEWDS): 24-year-old female with one week duration of central scotoma, OD. EyeRounds.org. April 8, 2005; Available from: http://www.EyeRounds.org/cases/37-MultipleEvanescentWhiteDotSyndromeMEWDS.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.