


INITIAL PRESENTATION
Chief Complaint: Blurry and light sensitive left eye
History of Present Illness
A 72-year-old Caucasian female patient with an eight-year history of mycosis fungoides (MF) was referred to an academic medical center for a central corneal ulcer in her left eye. Her past medical history was significant for a diagnosis of MF in 2016, for which she was on 12.5 mg of methotrexate daily. She had also recently experienced a recurrent cold sore. She presented two months prior to her referring physician with an erythematous and edematous left eyelid, subconjunctival hemorrhage, increased eye dryness, aching pain, and progressively blurry vision following minor trauma from plant debris to her left lateral canthus. Concurrently, she reported palmar desquamation and full-body urticaria associated with narrow band ultraviolet B (UVB) treatment for her T-cell lymphoma. The patient was empirically started on moxifloxacin eye drops, topical erythromycin ointment, oral prednisone (5 mg daily), valacyclovir (1000 mg three times a day), and doxycycline (100 mg daily). Upon referral to UIHC, her pain and swelling improved, however she had persistent blurry vision, redness, reduced floaters, and new onset photosensitivity in the left eye (Figure 1A, Figure 1B). She was also noted to have a cyst on her right lower lid.
Past Ocular History
Past Medical History
Medications
Allergies (reaction)
Family History: Non-contributory
Social History: Non-contributory
Review of Systems: Negative except for what is detailed in the history of present illness
OCULAR EXAMINATION
DIFFERENTIAL DIAGNOSIS:
CLINICAL COURSE
A targeted systemic workup was performed: the patient tested negative for antineutrophil cytoplasmic antibody (ANCA), rheumatoid factor (RF), and hepatitis C. Tear samples were sent for HSV detection by polymerase chain reaction (PCR), and samples from the corneal ulcer bed were sent to microbiology for Gram staining and fungal and bacterial cultures. Gram stain, KOH preparation, and cultures were negative; but the tear sample returned positive for HSV-1. She was treated for presumptive HSV epithelial keratitis with valacyclovir 1000 mg three times daily, and her prednisone use was tapered.
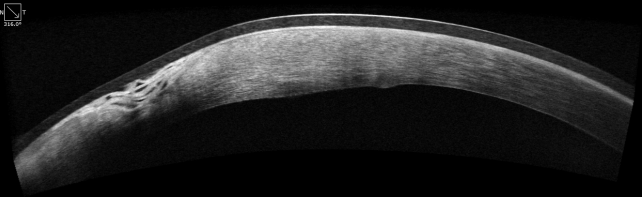
During this time, the patient’s dermatologist identified a new lesion on her cheek. A biopsy of the lesion returned positive for cutaneous T-cell lymphoma, and the patient underwent focal radiation therapy. Two weeks later, she returned with pruritus, discharge, and moderate photophobia in the left eye. The KP resolved with the patient’s course of valacyclovir. Her referring physician had placed an amniotic membrane graft (AMG) and a large diameter-soft bandage contact lens (BCL) due to progressive thinning in the interim. At her next visit, an anterior segment optical coherence tomography (OCT) demonstrated the degree of thinning. The AMG and bandage contact lens were also well-visualized (Figure 2a). A week later, the patient reported her left eye was itching substantially. While the visual acuity of the left eye improved from 20/400 to 20/150, slit-lamp exam revealed that the stromal thinning had worsened from 50% to 80% nasally. Anterior segment OCT showed 20% residual bed in most worrisome areas, with the AMG dissolved. The patient elected to undergo same-day conjunctival resection and tape tarsorrhaphy. Cyanoacrylate glue was placed to fill the trough and provide tectonic support. Her prednisone dose was increased to 30 mg.
Two weeks post-operatively, the patient’s slit-lamp exam of the left eye demonstrated conjunctival healing with resolution of the epithelial defect. Her stromal thinning had improved from 80% to 50% thinning. The patient continued her course of moxifloxacin, doxycycline 100 mg daily, and valacyclovir 1000 mg daily. She began a prednisone taper to 15 mg for a week and started fluorometholone eye drops three times a day. The bandage contact lens and glue fell off at the post-operative month 1 visit with gentle pressure with a cotton-tip applicator.
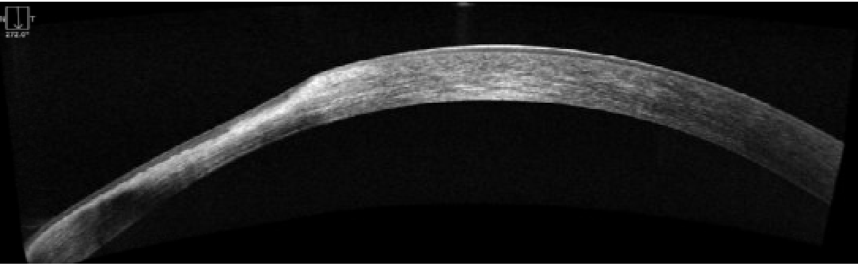
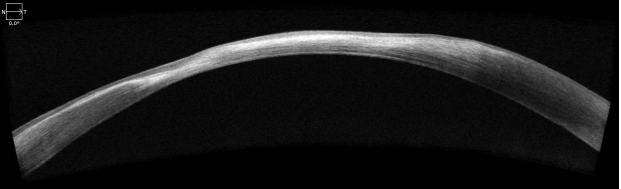
At her two-month post-operative visit, her visual acuity measured 20/50 uncorrected, and 20/30 with pinhole. Her slit-lamp exam revealed an intact epithelium with thickening in areas of underlying thin stroma and mild vascularity where tissue was resected (Figure 2b, 2c). Her referring physician increased her valacyclovir dosage to 1000 mg three times a day. This was maintained, and her fluorometholone use was tapered to once daily. Surgical options of crescentic deep anterior lamellar keratoplasty (DALK) or penetrating keratoplasty (PKP) were presented with the patient electing to defer for now.
DISCUSSION
The present case illustrates a rare corneal finding of PUK associated with the progression of MF. Notably, our patient’s initial presentation to the cornea clinic coincided with palmar desquamation and full-body urticaria associated with UV treatment for her T-cell lymphoma. This patient had a systemic inflammatory response coinciding with her PUK symptoms; therefore, we suspect that the corneal epithelium may have also been damaged during this reactive episode. There were multiple red herrings in this case: trauma with vegetative matter as well as the positive HSV PCR. However, this patient’s minimal response to valacyclovir suggests the HSV co-infection was less likely the primary disease driver. Our patient responded immediately the conjunctival resection, the established treatment for PUK.
Pathophysiology
PUK is a pathological condition most often resulting from systemic disease. As host autoimmunity becomes perturbed in systemic illness, complex inflammation leads to alterations in the physiology and anatomy of the cornea and surrounding environment. The fundamental causes of PUK may range from infectious etiologies such as staphylococcus to autoimmune disorders such as rheumatoid arthritis.(1) Cases of PUK without a systemic association are referred to as Mooren’s Ulcer.
Both humoral and cellular immune mechanisms can be involved in the pathogenesis of PUK. Immune complexes, formed from the combination of self-antigens and autoantibodies, activate B cells which can stimulate T cells to secrete cytokines that stimulate inflammation. Immune complexes in conjunction with angiogenesis contribute to pannus formation in the setting of PUK.(2)
The development of PUK in association with MF may be related to matrix metalloproteinase (MMP) upregulation in the setting of MF. Systemic MMP-2 and MMP-9 expression have been found to increase throughout the natural history of MF.9 Fujimura et al. reported an increase in mRNA expression of MMP-2 and MMP-9 as MF progresses, though the exact pathogenesis of this finding remains unclear.8 The patient’s flare of full body urticaria and palmar desquamation, which we assume to be related to her MF, could have resulted in a corresponding increase of MMP-2 and MMP-9. Smith et al. found a correlation between PUK, an increase in MMP-2 in the stroma, and MMP-9 in tear secretions. Given that PUK often occurs near sites of conjunctival inflammation, they suggested inflammatory cells stimulate a local increase in corneal gelatinases, which either provoke or sustain PUK.11 Thus, the patient’s MF progression and assumptive increase in MMP could have elicited an inflammatory cascade that resulted in the development of PUK. It is suspected that the initially unbeknownst HSV infection exacerbated the PUK healing process as the patient was in a severely immunocompromised state. There is also the possibility, as previous case reports have documented, that there may be direct tumor cell invasion of the cornea from malignant cells in the conjunctiva.12 This unique case highlights the potential for cutaneous T-cell lymphoma to be associated with PUK in the absence of lid findings which is a sequela that has not yet been reported in literature.
Pathophysiology
PUK is a pathological condition most often resulting from systemic disease. As host autoimmunity becomes perturbed in systemic illness, complex inflammation leads to alterations in the physiology and anatomy of the cornea and surrounding environment. The fundamental causes of PUK may range from infectious etiologies such as staphylococcus to autoimmune disorders such as rheumatoid arthritis.(1) Cases of PUK without a systemic association are referred to as Mooren’s Ulcer.
Both humoral and cellular immune mechanisms can be involved in the pathogenesis of PUK. Immune complexes, formed from the combination of self-antigens and autoantibodies, activate B cells which can stimulate T cells to secrete cytokines that stimulate inflammation. Immune complexes in conjunction with angiogenesis contribute to pannus formation in the setting of PUK.(2)
The development of PUK in association with MF may be related to matrix metalloproteinase (MMP) upregulation in the setting of MF. Systemic MMP-2 and MMP-9 expression have been found to increase throughout the natural history of MF.(9) Fujimura et al. reported an increase in mRNA expression of MMP-2 and MMP-9 as MF progresses, though the exact pathogenesis of this finding remains unclear.(8) The patient’s flare of full body urticaria and palmar desquamation, which we assume to be related to her MF, could have resulted in a corresponding increase of MMP-2 and MMP-9. Smith et al. found a correlation between PUK, an increase in MMP-2 in the stroma, and MMP-9 in tear secretions. Given that PUK often occurs near sites of conjunctival inflammation, they suggested inflammatory cells stimulate a local increase in corneal gelatinases, which either provoke or sustain PUK.(11) Thus, the patient’s MF progression and assumptive increase in MMP could have elicited an inflammatory cascade that resulted in the development of PUK. It is suspected that the initially unbeknownst HSV infection exacerbated the PUK healing process as the patient was in a severely immunocompromised state. There is also the possibility, as previous case reports have documented, that there may be direct tumor cell invasion of the cornea from malignant cells in the conjunctiva. (12) This unique case highlights the potential for cutaneous T-cell lymphoma to be associated with PUK in the absence of lid findings which is a sequela that has not yet been reported in literature.
Epidemiology
Mycosis fungoides is the most common cutaneous T-cell lymphoma, affecting approximately 3.7 per million people per year. Prognosis is favorable with an estimated 5-year survival of between 79% and 92%.(4) PUK has a similar incidence of approximately 3 per million per year, with rheumatoid arthritis and granulomatosis with polyangiitis being the most common underlying pathology.(5)
This is the first reported case of PUK caused by MF with concurrent corneal HSV-1 infection; and the first case of corneal involvement, without lid findings, in the setting of MF. Previous cases of ocular involvement in patients with lymphoma have been reported, including one association with PUK.(6,7) In patients with MF specifically, only two corneal manifestations have been reported: a case of circumferential infiltration and subsequent perforation; and a case of focal interstitial keratitis.(7,8)
EPIDEMIOLOGY OR ETIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT/MANAGEMENT
|
Sarin SA, Davis K, Ahmad NUS, Donegan P, Matharu KS. Peripheral Ulcerative Keratitis in the Setting of Mycosis Fungoides. Posted Feb. 25, 2025. Available from https://eyerounds.org/cases/363-PUK_Setting_Mycosis_Fungoides.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.