Tearing and blurry vision in the left eye.
A 72-year-old male was referred to the oculoplastics service for evaluation of left lower eyelid retraction in the setting of left facial nerve palsy secondary to metastatic lymphoma and radiation therapy. He had prior treatment by the otolaryngology service including a left temporalis fascia sling, left upper eyelid platinum gold weight and a left lateral tarsal strip. He had persistence of tearing and blurry vision in the left eye which seemed to improve with the instillation of artificial tears.
Visual acuity without correction, distance
Pupils: No afferent pupillary defect
Extraocular motility: Full
Confrontation visual fields: Full
External exam (Figure 1)
Slit lamp exam
Fundus exam

Figure 1. External photograph demonstrating left lower eyelid retraction with inferior scleral show. There is left lagophthalmos present during eyelid closure.
Because of the patient's significant exposure keratopathy, the decision was made to proceed with a left lower eyelid spacer graft from the hard palate in addition to a left drill hole cheek lift with repeat lateral tarsal strip and lateral tarsorrhaphy.
At the 2 week post-operative follow-up there was minimal lagophthalmos present (around 1 mm medially) and the lower eyelid was found to be in excellent position. At the 5 month post-operative follow-up there was significant improvement in the ocular surface with no corneal exposure. He continued with excellent eyelid position (Figure 2), but he had a foreign body sensation from an aberrant eyelash, which was ultimately removed.
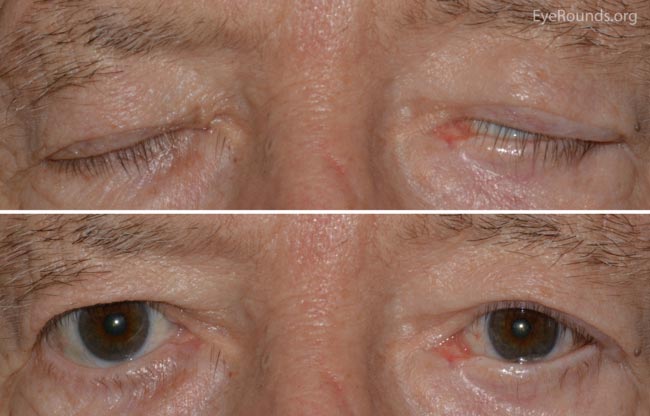
Figure 2. External photograph demonstrating stable lower eyelid position. There is persistence of mild lagophthalmos during eyelid closure without corneal exposure.
The facial nerve arises from the pons and travels through the internal auditory canal and the petrous portion of the temporal bone before innervating the muscles of facial expression. It is accompanied by the parasympathetic fibers of the nervus intermedius, which is responsible for tearing, salivation and taste. Voluntary facial movement arises from the precentral gyrus while involuntary blinking arises from basal ganglia extrapyramidal connections. Innervation of the upper facial muscles originates from bilateral corticobulbar projections to the upper part of the ipsilateral facial nucleus. The lower facial muscles receive innervation from contralateral corticobulbar projections to the lower part of the ipsilateral facial nucleus. Thus, a lesion to the upper motor neuron would result in paralysis of only the contralateral lower facial muscles. A lower motor neuron lesion would result in ipsilateral paralysis of both the upper and lower facial muscles and is the most common form of facial paralysis. This distinction is important in localizing lesions that cause facial paralysis (1).
The branches of the facial nerve include the temporal, zygomatic, buccal, mandibular and cervical divisions. The orbicularis oculi is innervated by the temporal, zygomatic and sometimes the buccal branch of the facial nerve. The orbital portion of the orbicularis oculi muscle is responsible for forced eyelid closure and the pretarsal portion is responsible for involuntary blinking.
Bell's Palsy
Encompassing around 51% of cases of facial nerve palsy, Bell's palsy is a unilateral, acute onset (<72 hour), and idiopathic facial paralysis affecting around 23 people per 100,000 per year or about 1 in 60-70 people in a lifetime (2). It occurs equally between men and women and peaks between the ages of 10 and 40 (3). It is more common in those with diabetes, upper respiratory ailments, immune compromise and pregnancy and often is accompanied by a viral prodrome (4). Most patients (70-80%) with Bell's palsy have some spontaneous recovery beginning within 2-3 weeks of the onset of symptoms, but it can take months to resolve completely. Around 13% of patients have permanent insignificant sequelae and 16% have permanent and significantly altered facial function (5). Approximately 7% of patients experience recurrence of Bell's palsy. Though still considered a diagnosis of exclusion, an association with herpes simplex virus has recently been suggested (6). Treatment typically consists of oral anti-viral and corticosteroid therapy, though the significance of these regimens remains unclear (7).
Infection
Severe bacterial infections including otitis media, otitis externa and mastoiditis can cause facial nerve palsy due to involvement of the facial nerve. Lyme disease caused by the transmission of Borrelia burgdorferi via tick bites causes facial nerve palsy in 10% of infected patients with 25% of these being bilateral (8). Herpes zoster virus can cause facial nerve palsy in addition to a classic painful vesicular eruption and is called Ramsay Hunt syndrome or genicular ganglionitis. These patients often have considerable pain and are less responsive to therapy (9). A number of other infections have been noted to cause facial nerve palsy including diphtheria, enterovirus, HIV, varicella, polio, mumps, leprosy, dengue fever and cat scratch (10).
Trauma
Damage can occur to the facial nerve in the setting of blunt or penetrating trauma or iatrogenically during surgery on the face, neck, or ear—especially the parotid gland. In addition, involvement of cranial nerves V, VI, VIII, and Horner syndrome can occur after resection of cerebellopontine angle tumors (10).
Neoplastic
Tumors of the pons, cerebellopontine angle, inferior temporal bone, external auditory canal or parotid gland can damage the facial nerve and usually present with a more gradual onset of paralysis compared with Bell's palsy or infection (10).
Miscellaneous
A number of other etiologies of facial nerve paralysis are documented including congenital facial paralysis (Mobius syndrome), diabetes, Guillain-Barre syndrome, Melkersson-Rosenthal syndrome, sarcoidosis (Heerfordt syndrome), infarction, pontine demyelination, and vasculitis (11).
Facial nerve palsy most commonly presents as an acute onset of unilateral facial weakness or loss of facial expression including loss of forehead wrinkling, brow ptosis, incomplete eyelid closure, and drooping of the mouth with possible drooling. There can be associated pain around the jaw or behind the ear, headaches, and changes in taste, tearing, or hearing.
Grading of facial nerve palsy can be performed using the House-Brackman guide (adapted from 12).
Grade I. Normal blink and eyelid closure
Grade II. Full eyelid closure with minimal effort
Grade III. Full eyelid closure with maximal effort
Grade IV. Incomplete closure with normal facial symmetry
Grade V. Incomplete closure with facial asymmetry
Grade VI. No eyelid movement
Common ocular signs of facial nerve palsy include upper eyelid retraction, lower eyelid paralytic ectropion and laxity with widening of the palpebral fissure, lagophthalmos, incomplete blink, corneal exposure keratopathy, and dry eye. Signs of chronic exposure include corneal pannus, thinning, and corneal ulceration. It is important to check corneal sensation in all patients with facial nerve palsy to ensure there is no involvement of cranial nerve V as this portends a worse prognosis for corneal exposure. Evaluation of upward eye movement with attempted eyelid closure—called Bell's phenomenon—should be noted as it can serve to protect the cornea. The extent of voluntary closure can be tested by having the patient forcibly close the eyelids and observing the extent to which the eyelashes are buried. Health of the ocular surface should be assessed using Schirmer and dye testing (such as fluorescein, lissamine green or rose bengal) as there is loss of parasympathetic tear stimulation and meibomian gland morphology has been shown to be altered after greater than 3 months of facial nerve palsy (13).
The primary ophthalmic concern in facial nerve palsy is corneal exposure and lagophthalmos. Fluorescein dye can reveal areas of keratopathy secondary to exposure, which can range from mild punctate epithelial erosions to large epithelial defects and corneal infiltrates. Prolonged exposure can lead to corneal thinning and perforation, especially in the setting of diminished corneal sensation.
In addition to corneal exposure, patients may suffer from epiphora due to lower eyelid ectropion and poor tear pumping mechanism, reflex tearing from dry eye or aberrant innervation of the lacrimal gland, facial synkinetic movements such as blinking or eyelid retraction with oral movement, and poor peri-ocular cosmesis (10).
When presented with a case of facial nerve palsy, the first decision is often to determine if more work-up is needed to rule out a potentially more sinister cause for the paralysis. Observation is warranted in the setting of a classic viral prodrome with rapid onset of partial unilateral palsy which is present for less than 3 weeks. Further evaluation, including imaging, is recommend if the palsy progresses over a period of 3 weeks, is complete in nature or has a gradual onset (4). At our institution, the tendency is toward imaging in all cases of facial nerve palsy lasting greater than 3 weeks, given the ease with which these can often be obtained and the potential medical and legal ramifications of missing an occult process.
Medical
Ophthalmologic consultation is recommended in the setting of facial nerve palsy when ocular symptoms are present or there is concern about decreased corneal sensation (i.e., CN V involvement). In addition, it is advised for patients where prolonged or permanent facial nerve paralysis is expected as more intensive therapy is anticipated.
Conservative management can be divided into five broad categories including lubrication, retaining moisture, obstruction of tear outflow, improvement of tear quality and bandage or scleral contact lenses.
Aggressive lubrication of the ocular surface includes the administration of artificial tears in mild cases and thicker lubricating gels or ointments for more severe cases. Ointment can be placed on the eye at bedtime to prevent corneal exposure. Preservative-free preparations are preferred when used chronically to decrease the incidence of allergy or toxicity.
Retention of moisture can be obtained by room air humidifiers, turning off fans in the environment, wearing humidification goggles or Saran Wrap ™ chamber, moisture release eyewear or simply taping the eye shut.
Obstruction of tear flow can be accomplished by the placement of silicone punctal plugs or permanent thermal cautery of the punctum in cases where there is no lower eyelid malposition. This is most often used in younger patients who are less likely to have lower eyelid malposition given the fact that their eyelids are tighter.
Video 1. Punctal cautery. If video fails to load use this link: https://vimeo.com/132967651/.
The tear film quality can be improved by frequent artificial tears in addition to increasing the lipid component of the tears through warm compresses, lipid-enhanced artificial tears, oral omega-3 fatty acids (fish and flaxseed oil), doxycycline, or procedures such as LipiFlow®. In addition, autologous serum eye drops can be used to stabilize the ocular surface and replace factors commonly found in natural tears.
Bandage soft contact lenses can be placed to protect the ocular surface from exposure, but require antibiotic prophylaxis, instruction on duration of wear, and close follow-up to prevent infectious complications. Scleral hard lenses are especially beneficial in patients with CN V and CN VII palsies in that they can provide an excellent long-term solution for corneal exposure and can be customized to the patient's corneal and refractive needs.
Temporary interventions
The upper eyelid can be lowered using adhesive stick-on weights with or without a splint resulting in immediate eyelid closure. Examples include the Blinkeze™ external lid weights, Stamler lid splint, and the temporary eyelid closure appliqué (14).
Protective ptosis can be induced with botulinum toxin (5-15 units) injected into the levator muscle. Ptosis onset occurs on average 4 days after injection and lasts around 6 weeks (15). Complications of toxin injection include diplopia which has been described to last up to 9 months after injection (16). In addition, hyaluronic acid gel can be injected to mechanically lower the eyelid. An advantage of hyaluronic acid is that is reversible with hyaluronidase (17).
The eyelids can be closed temporarily using cyanoacrylate glue or Dermabond® which generally lasts 2 weeks, but can be taken down by cutting the eyelashes after anesthesia with 4% lidocaine gel (18, 19, 20).
Video 2. Glue tarsorrhaphy. If video fails to load use this link: https://vimeo.com/132966666.
Temporary suture tarsorrhaphy involves using absorbable (2-3 weeks) or non-absorbable suture to close the eyelids. Bolsters can be used to prevent the suture from pulling through the eyelid and a releasable technique can allow intermittent opening of the eyelids for corneal examination (21, 22, 23).
Video 3. Temporary Bolster tarsorrhaphy. If video fails to load use this link: https://vimeo.com/132967652.
Permanent tarsorrhaphy
Lateral tarsorrhaphy is the most common form of permanent tarsorrhaphy and involves closing the temporal palpebral fissure. While very effective, it may limit peripheral vision and be cosmetically objectionable. The amount of tarsorrhaphy can be adjusted for the desired effect (protection vs cosmesis or temporal vision).
Video 4. Lateral tarsorrhaphy. If video fails to load use this link: https://vimeo.com/132967645/.
A medial tarsorrhaphy results in relatively good cosmesis and improves the medial descent when orbicularis tone is poor, but is less effective than a lateral tarsorrhaphy (24).
Video 5. Medial tarsorrhaphy. If video fails to load use this link https://vimeo.com/132967647/.
A pillar tarsorrhaphy involves connecting the upper and lower eyelid on either side of the pupil which can provide complete closure while allowing examination of the cornea (25, 26).
Video 6. Pillar tarsorrhaphy. If video fails to load use this link: https://vimeo.com/132967649.
Rehabilitation
Eyebrow rehabilitation involves lifting the brow and can be accomplished by several techniques depending on skin type, hairline, and rhytids. The amount of lift and patient cosmetic expectations should be considered prior to surgery.
Video 7. Paralytic brow ptosis repair. If video fails to load use this link: https://vimeo.com/132966661.
Surgical upper eyelid rehabilitation can be thought of as static or dynamic in nature. Static interventions include gold or platinum upper eyelid weights which mechanically lower the eyelid and improve passive eyelid closure with increased closure during blink.
Video 8. Gold weight insertion. If video fails to load use this link: https://vimeo.com/132966668.
Complications of weight placement include lash ptosis or trichiasis, visibility through the skin, displacement or extrusion of the weight, allergy, and infection (27, 28, 29). Dynamic eyelid closure is achieved using a palpebral spring that attaches between the lateral orbital rim and the tarsus and forces the eyelid closed during levator inaction.
Lower eyelid malposition in facial nerve palsy should be treated more aggressively than simple ectropion and should instead be thought of as lower eyelid retraction. In addition to lower eyelid tightening procedures such as the lateral tarsal strip, placement of a spacer is often indicated and can be augmented with a midface lift and medial tarsorrhaphy.
Video 9. Hard palate graft for lower eyelid retraction. If video fails to load use this link: https://vimeo.com/132966657.
Video 10. Drill hole midface lift. If video fails to load use this link: https://vimeo.com/132966665.
Video 11. Enduragen graft with a preperiosteal midface lift for treatment of lower eyelid retraction. If video fails to load use this link: https://vimeo.com/133680716
In longstanding or recovering facial palsies—most commonly Bell's palsy—aberrant innervation can occur in three forms. Hypertonicity occurs as the affected side appears contracted at rest despite decreased dynamic function. Synkinesis involves regenerating axons reinnervating different muscles than those originally served; for example, movements of the lower face can cause eyelid closure or blinking can cause mouth twitching. In addition, gustatory lacrimation or "crocodile tears" can occur as fibers to sublingual and mandibular glands reinnervate the lacrimal gland and cause tearing during chewing. Hyertonicity, synkensis, and gustatory lacrimation have been successfully treated with botulinum toxin administration (30, 31).
Direct eyelid reanimation through reinnervation and corneal neurotization are two future directions in facial nerve palsy therapy. Corneal neurotization has been shown to successfully reinstate sensation to the cornea through introduction of donor nerve tissue placed subconjunctivally near the corneal limbus. Approaches include donor contralateral supratrochlear or supraorbital nerves which leave an insensate forehead and bicoronal scar or leg sural nerve transfer which can be performed bilaterally and induces less scarring (32, 33).
Etiology
|
Signs
|
Symptoms
|
Management
|
Welder JD, Allen RC, Shriver EM. Facial Nerve Palsy: Ocular Complications and Management. EyeRounds.org. posted July 14, 2015; Available from: http://www.EyeRounds.org/cases/215-facial-nerve.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.