Chief Complaint: Right eyelid swelling, pain, decreased vision, diplopia
History of Present Illness: 80-year-old female presented to our emergency room with a three-day history of worsening right eyelid swelling, eye pain especially with movement, inability to open her right eye, thick crusty mattering and blurry vision. She also experienced diplopia in all gazes.
Of note, she states that her symptoms started after her first dose of IV Reclast® (zoledronate) for her recent diagnosis of osteoporosis.
Past Ocular History:
Medical History:
Medications:
Allergies:
Family History: Macular Degeneration - Mother
Social History: Non-contributory
Review of Systems: 12 point Review of systems Chills, no fever, no trauma. Otherwise, all negative aside from symptoms and signs mentioned in History of Present Illness
EXTERNAL/SLIT LAMP EXAM:
DILATED FUNDUS EXAM:
Pertinent Laboratory Values:
 |
 |
 |
HOSPITAL COURSE:
The patient was admitted to the hospital and treated with systemic IV steroids for presumed orbital inflammation. She did not have other signs in her physical exam or her laboratory work up to suggest a systemic illness.
After 2 doses of Solu-Medrol® (methylprednosolone sodium succinate) 500mg IV, the patient's symptoms and signs improved significantly. She was discharged home the next day on a tapering dose of oral prednisone. Inflammation resolved completely after one week. There has been no recurrence of inflammation.
 |
 |
Orbital inflammation is generally categorized as infectious or non-infectious. Infectious etiologies include bacteria and fungi, most often related to sinus disease. Non-infectious etiologies are abundant, but often grouped under the heading of orbital pseudotumor or idiopathic orbital inflammation until a specific etiology is elucidated.
Orbital and ocular inflammation after bisphosphonate treatment has been adequately reported in the literature. Bisphosphonates are used in the treatment of osteoporosis, Paget's disease, metastatic bone disease, and are used as adjuvant therapy for breast cancer. They are synthetic analogues of a regulator of bone metabolism called pyrophosphates and stimulate the release of osteoclastic inhibitory factors from osteoblasts, inhibit the osteoclastic precursor differentiation, and induce apoptosis of osteoclasts. Newer nitrogen-based IV bisphosphonates such as pamidronate and zoledronate are the most widely used and potent.
This patient was treated with zoledronate, which is the most potent bisphosphonate; however, to date, the majority of reports in the literature are based on adverse reactions from pamidronate.
Symptoms occur usually within 6-48 hours after the infusion. It is most common with the first or second infusion. Rapid resolution of the inflammation is expected after discontinuation of the offending medication and systemic corticosteroid treatment.
Of note, certain bisphosphonates share several homologs with T cell ligands which activate antigentic receptor T cells and release cytokines. This interaction explains why certain patients may present with an acute systemic inflammatory reaction including low grade fever, myalgia, arthralgia, nausea and vomiting along with ocular complications.
The patient's rheumatologist and primary care physician should be notified of this adverse effect. If the patient needs to be treated subsequently with a bisphosphonate, close monitoring should be performed to address any possible repeat inflammation. However, in general, subsequent use of bisphosphonates after this adverse reaction is discouraged.
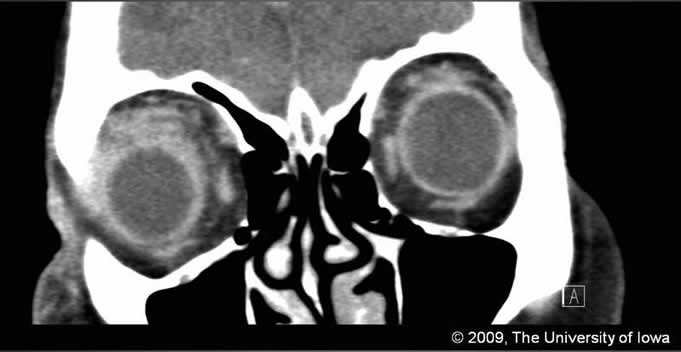
Diagnosis: Orbital inflammation related to bisphosphonate treatment.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Hong ES, Birkholz ES, Wendel L, Allen RC. Orbital inflammation secondary to bisphosphonate therapy (orbital pseudotumor). EyeRounds.org. January 4, 2010; Available from: http://www.EyeRounds.org/cases/101-orbitalpseudotumor.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.